Diagnosis is made, first by eliciting the presence of ascites, then by looking for signs and symptoms consistent with peritoneal irritation or signs of systemic infection, and finally by confirmation with peritoneal fluid testing.
History and physical exam
Patients with end-stage liver disease presenting with hepatic encephalopathy, decompensated cirrhosis, increase in ascites volume and/or frequency, or gastrointestinal (GI) bleeding are at particularly high risk for SBP. Patients who have recently had a therapeutic endoscopy are also at risk. Ascites due to malignancy, renal insufficiency, or congestive heart failure also carry a risk, albeit one that is less well-described than the risk in patients with end-stage liver disease.[78]Makharia GK, Sharma BC, Bhasin DK, et al. Spontaneous bacterial peritonitis in a patient with gastric carcinoma. J Clin Gastroenterol. 1998 Oct;27(3):269-70.
http://www.ncbi.nlm.nih.gov/pubmed/9802463?tool=bestpractice.com
The typical presentation of SBP includes abdominal pain, fever, increasing ascites, ileus and/or altered mental status in a patient with known liver disease; however, one third of patients also may be asymptomatic or present with only mild symptoms.[1]Rimola A, Garcia-Tsao G, Navasa M, et al; International Ascites Club. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. J Hepatol. 2000 Jan;32(1):142-53.
http://www.journal-of-hepatology.eu/article/S0168-8278(00)80201-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/10673079?tool=bestpractice.com
[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[79]Long B, Gottlieb M. Emergency medicine updates: spontaneous bacterial peritonitis. Am J Emerg Med. 2023 Aug;70:84-9.
https://www.sciencedirect.com/science/article/abs/pii/S0735675723002589
http://www.ncbi.nlm.nih.gov/pubmed/37244043?tool=bestpractice.com
The wide range of possible physical exam findings include symptoms of peritonitis (e.g., vomiting, diarrhea, ileus, abdominal tenderness), systemic inflammation (e.g., hypothermia, hyperthermia, tachycardia, tachypnea), shock, hepatic encephalopathy, renal failure, and GI bleeding.[80]European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010 Sep;53(3):397-417.
https://www.journal-of-hepatology.eu/article/S0168-8278(10)00478-2/fulltext
Peritoneal fluid testing is the only way to confirm or rule out SBP; signs, symptoms, and clinical gestalt are unreliable.[81]Chinnock B, Afarian H, Minnigan H, et al. Physician clinical impression does not rule out spontaneous bacterial peritonitis in patients undergoing emergency department paracentesis. Ann Emerg Med. 2008 Sep;52(3):268-73.
http://www.ncbi.nlm.nih.gov/pubmed/18433932?tool=bestpractice.com
[82]Chinnock B, Hendey GW, Minnigan H, et al. Clinical impression and ascites appearance do not rule out bacterial peritonitis. J Emerg Med. 2013 May;44(5):903-9.
http://www.ncbi.nlm.nih.gov/pubmed/23473819?tool=bestpractice.com
Detection of ascites
There are several maneuvers for the detection of ascites, including examining for flank dullness, shifting dullness, fluid wave, and auscultatory percussion.
Flank dullness is elicited by percussion of the abdominal wall starting at the periumbilical region and going outwards to the dependent areas of the flanks. If ascites is present, there is a change from tympany to dullness.
To detect shifting dullness, the abdomen should be percussed from the umbilicus laterally and the level noted at which tympany turns to dullness. Then the patient should be positioned in the right lateral decubitus position. The abdomen is percussed again, starting on the left side and going toward the right. If ascites is present, the level at which tympany turns to dullness will have shifted.
Assistance is required to detect a fluid wave. The patient should be in the supine position, and the ulnar side of the assistant's hand and forearm is placed lengthways in the midline of the anterior abdominal wall. The examiner's hands are then placed on either side of the abdomen. When one hand strikes the abdomen, a fluid wave will be felt by the other hand in a patient with ascites.
Auscultatory percussion is conducted with the patient standing. Auscultation is started just above the symphysis pubis while percussing from the costal margin down to the pelvis. Normally there is a sharp transition from quiet to loud at the pelvic border. In a patient with ascites, the transition occurs higher up.
The sensitivities and specificities of these signs for ascites vary widely. Percussion of the abdominal wall is the most sensitive of all the maneuvers for ascites, with a sensitivity of 84%.[83]McGibbon A, Chen GI, Peltekian KM, et al. An evidence-based manual for abdominal paracentesis. Dig Dis Sci. 2007 Dec;52(12):3307-15.
http://www.ncbi.nlm.nih.gov/pubmed/17393312?tool=bestpractice.com
Ultrasound is the definitive test for the detection of ascites. Up to 25% of patients thought to have ascites by physical exam techniques who go on to have an abdominal ultrasound are found to have no or minimal ascites.[84]Nazeer SF, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians versus the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005 May;23(3):363-7.
http://www.ncbi.nlm.nih.gov/pubmed/15915415?tool=bestpractice.com
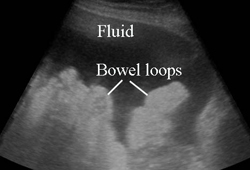
Sonography can determine adequacy of fluid for paracentesis and can help localize the procedure.[Figure caption and citation for the preceding image starts]: Abdominal ultrasound showing large amount of ascites with bowel loopsFrom the personal collection of Brian Chinnock, MD; used with permission [Citation ends].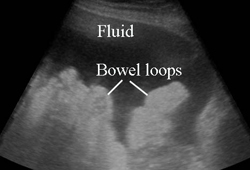
Initial investigations
Initial laboratory tests should include:[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[85]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
CBC, which may show an elevated white cell count; anemia may be a clue to a GI bleed.
Creatinine, as hepatorenal syndrome may occur concomitantly.
Liver function tests, to establish baseline labs and monitor the health of the liver.
Prothrombin time/INR, which should be performed if there is GI or other bleeding.
Blood cultures, which may assist in identifying the pathogenic organism, as the yield from peritoneal fluid culture is poor. The Infectious Diseases Society of America (IDSA) recommends 2-3 sets of blood cultures for identification of concomitant bacteremia.
Diagnostic paracentesis
Owing to the high prevalence of SBP in hospitalized patients with cirrhosis and ascites, diagnostic paracentesis should be performed on all patients with these two conditions, even in the absence of symptoms suggestive of infection.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[64]European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-60.
https://www.doi.org/10.1016/j.jhep.2018.03.024
http://www.ncbi.nlm.nih.gov/pubmed/29653741?tool=bestpractice.com
Patients with known ascites who present with GI bleed or hepatic encephalopathy should also generally be evaluated for SBP. Diagnostic paracentesis has been shown to be safe in patients with significant coagulopathy or thrombocytopenia; fresh frozen plasma or platelet transfusion is not indicated before diagnostic paracentesis in patients with coagulopathy.
Diagnostic paracentesis should be performed as early as possible.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
Early paracentesis of hospitalized patients with ascites was associated with lower all-cause mortality, SBP mortality, and 30-day re-admission rate in a large inpatient database study.[91]Rosenblatt R, Tafesh Z, Shen N, et al. Early Paracentesis in high-risk hospitalized patients: time for a new quality indicator. Am J Gastroenterol. 2019 Dec;114(12):1863-9.
https://www.doi.org/10.14309/ajg.0000000000000443
http://www.ncbi.nlm.nih.gov/pubmed/31688022?tool=bestpractice.com
Ascitic fluid laboratory analysis
The key tests on peritoneal fluid for the analysis of SBP are a cell count and culture.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
A minimum of 10 mL (and up to 50 mL if available) of peritoneal fluid should be cultured aseptically at the bedside in aerobic and anaerobic blood culture bottles before giving antibiotics.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[85]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
Additional laboratory testing should include fluid analysis for protein, lactate dehydrogenase (LDH), and pH.[85]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
The gross appearance of the fluid can also be examined by laboratory staff.
Cell count
A peritoneal fluid absolute neutrophil count (ANC) >250 cells/mm³ is the accepted criterion for the diagnosis of SBP.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[64]European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-60.
https://www.doi.org/10.1016/j.jhep.2018.03.024
http://www.ncbi.nlm.nih.gov/pubmed/29653741?tool=bestpractice.com
Although an ANC >500 cells/mm³ is more specific for the diagnosis, the danger of missing SBP in a patient with an ANC count between 250-500 cells/mm³ is unacceptably high.[1]Rimola A, Garcia-Tsao G, Navasa M, et al; International Ascites Club. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. J Hepatol. 2000 Jan;32(1):142-53.
http://www.journal-of-hepatology.eu/article/S0168-8278(00)80201-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/10673079?tool=bestpractice.com
Therefore, a patient who is felt to be at high risk for SBP should be considered for treatment.
Automated cell counters have been found to be equivalent to manual cell counts in the examination of ascitic fluid.[92]Angeloni S, Nicolini G, Merli M, et al. Validation of automated blood cell counter for the determination of polymorphonuclear cell count in the ascitic fluid of cirrhotic patients with or without spontaneous bacterial peritonitis. Am J Gastroenterol. 2003 Aug;98(8):1844-8.
http://www.ncbi.nlm.nih.gov/pubmed/12907342?tool=bestpractice.com
[93]Riggio O, Angeloni S, Parente A, et al. Accuracy of the automated cell counters for management of spontaneous bacterial peritonitis. World J Gastroenterol. 2008 Oct 7;14(37):5689-94.
https://www.wjgnet.com/1007-9327/full/v14/i37/5689.htm
http://www.ncbi.nlm.nih.gov/pubmed/18837085?tool=bestpractice.com
[94]Cereto F, Genesca J, Segura R. Validation of automated blood cell counters for the diagnosis of spontaneous bacterial peritonitis. Am J Gastroenterol. 2004 Jul;99(7):1400.
http://www.ncbi.nlm.nih.gov/pubmed/15233685?tool=bestpractice.com
Culture
Culture of ascitic fluid, even in patients with obvious SBP, has a low yield because of the low concentration of bacteria compared with infections in other organic fluids (e.g., urine).
Inoculating ascitic fluid directly into blood culture bottles at the bedside has demonstrated significantly increased yield and should be the standard method of collection.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[95]Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic fluid culture technique. Gastroenterology. 1988 Nov;95(5):1351-5.
https://www.doi.org/10.1016/0016-5085(88)90372-1
http://www.ncbi.nlm.nih.gov/pubmed/3049220?tool=bestpractice.com
However, cultures are still negative in approximately 50% of patients with an ascites ANC >250 cells/mm³.[1]Rimola A, Garcia-Tsao G, Navasa M, et al; International Ascites Club. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. J Hepatol. 2000 Jan;32(1):142-53.
http://www.journal-of-hepatology.eu/article/S0168-8278(00)80201-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/10673079?tool=bestpractice.com
[19]Boixeda D, De Luis DA, Aller R, et al. Spontaneous bacterial peritonitis: clinical and microbiological study of 233 episodes. J Clin Gastroenterol. 1996 Dec;23(4):275-9.
http://www.ncbi.nlm.nih.gov/pubmed/8957729?tool=bestpractice.com
Polymicrobial growth may be suggestive of secondary peritonitis.
Fluid appearance
Subjective descriptions of ascitic fluid by laboratory technicians as abnormal with the descriptors "hazy," "cloudy," or "bloody" have a sensitivity of between 72% and 98% for the detection of SBP.[82]Chinnock B, Hendey GW, Minnigan H, et al. Clinical impression and ascites appearance do not rule out bacterial peritonitis. J Emerg Med. 2013 May;44(5):903-9.
http://www.ncbi.nlm.nih.gov/pubmed/23473819?tool=bestpractice.com
[96]Chinnock B, Hendey GW. Can clear ascitic fluid appearance rule out spontaneous bacterial peritonitis? Am J Emerg Med. 2007 Oct;25(8):934-7.
http://www.ncbi.nlm.nih.gov/pubmed/17920980?tool=bestpractice.com
Clinical impression, including an assessment of ascitic fluid appearance, should not be used to exclude the diagnosis.[82]Chinnock B, Hendey GW, Minnigan H, et al. Clinical impression and ascites appearance do not rule out bacterial peritonitis. J Emerg Med. 2013 May;44(5):903-9.
http://www.ncbi.nlm.nih.gov/pubmed/23473819?tool=bestpractice.com
Other tests that may be performed on ascitic fluid include glucose, acid fast bacterium (AFB) stain and culture, fungal culture, and microscopy for ova and parasites, depending on the clinical context.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[85]Miller JM, Binnicker MJ, Campbell S, et al. Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. 2024 Mar 5:ciae104.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae104/7619499
http://www.ncbi.nlm.nih.gov/pubmed/38442248?tool=bestpractice.com
[97]Neungton N, Kachintorn U, Chinapak O, et al. Significance of ascitic fluid white blood cells, pH, lactate, and other chemistry in immediate diagnosis of spontaneous bacterial peritonitis. J Med Assoc Thai. 1994 May;77(5):266-70.
http://www.ncbi.nlm.nih.gov/pubmed/7869010?tool=bestpractice.com
The measurement of carcinoembryonic antigen and alkaline phosphatase can be performed to help differentiate SBP from secondary peritonitis.[98]Wu SS, Lin OS, Chin YY, et al. Ascitic fluid carcinoembryonic antigen and alkaline phosphatase levels for the differentiation of primary from secondary bacterial peritonitis with intestinal perforation. J Hepatol. 2001 Feb;34(2):215-21.
http://www.ncbi.nlm.nih.gov/pubmed/11281549?tool=bestpractice.com
Measurement of the serum-ascites albumin gradient (SAAG) and ascitic total protein concentration should be considered for a first episode of ascites, with SAAG measurement recommended if a cause of ascites different from cirrhosis is suspected.[61]Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.
https://www.doi.org/10.1002/hep.31884
http://www.ncbi.nlm.nih.gov/pubmed/33942342?tool=bestpractice.com
[64]European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-60.
https://www.doi.org/10.1016/j.jhep.2018.03.024
http://www.ncbi.nlm.nih.gov/pubmed/29653741?tool=bestpractice.com
Ascitic fluid lactoferrin can also be measured. Along with helping to identify SBP in a cirrhotic patient with ascities, an elevated lactoferrin in a cirrhotic patient without SBP can indicate a developing hepatic carcinoma.[99]Lee SS, Min HJ, Choi JY, et al. Usefulness of ascitic fluid lactoferrin levels in patients with liver cirrhosis. BMC Gastroenterol. 2016 Oct 13;16(1):132.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5062891
http://www.ncbi.nlm.nih.gov/pubmed/27733127?tool=bestpractice.com
Highly-sensitive leukocyte esterase reagent strip testing (Periscreen), a test created to examine peritoneal dialysis fluid for infection, has been studied in ascitic fluid to rule out SBP and may be of use if laboratory peritoneal fluid testing is not available. In a multicenter study that assessed 84 ascitic fluid samples from 9 outpatients (17 ascitic fluid samples) and 31 inpatients (67 ascitic fluid samples) diagnosed with SBP, the leukocyte esterase reagent strip test had a sensitivity of 92% and specificity of 57%.[100]Thévenot T, Briot C, Macé V, et al; CFEHTP, ANGH and the PerDRISLA Study Group. The Periscreen strip is highly efficient for the exclusion of spontaneous bacterial peritonitis in cirrhotic outpatients. Am J Gastroenterol. 2016 Oct;111(10):1402-9.
http://www.ncbi.nlm.nih.gov/pubmed/27619833?tool=bestpractice.com
An emergency department-based study demonstrated a sensitivity of 95%.[101]Chinnock B, Woolard RE, Hendey GW, et al. Sensitivity of a bedside reagent strip for the detection of spontaneous bacterial peritonitis in ED patients with ascites. Am J Emerg Med. 2019 Dec;37(12):2155-8.
https://www.doi.org/10.1016/j.ajem.2019.01.044
http://www.ncbi.nlm.nih.gov/pubmed/30737002?tool=bestpractice.com
Bedside (standard urine) leukocyte esterase reagent strip testing of ascitic fluid has been studied in the evaluation of SBP. The reagent strip is dipped into ascitic fluid, and after 60-120 seconds the result is analyzed according to the colorimetric scale for that reagent strip. Most studies used a strip color that gives a positive result as corresponding to between 15 (1+) and 125 leukocytes/mL (3+). One meta-analysis found sensitivities ranging from 45% to 100% and specificities ranging from 81% to 100%.[102]Koulaouzidis A, Leontiadis GI, Abdullah M, et al. Leukocyte esterase reagent strips for the diagnosis of spontaneous bacterial peritonitis: a systematic review. Eur J Gastroenterol Hepatol. 2008 Nov;20(11):1055-60.
http://www.ncbi.nlm.nih.gov/pubmed/19047835?tool=bestpractice.com
Low sensitivity demonstrates that bedside (standard urine) leukocyte esterase reagent strip testing is not suitable for rapidly ruling out SBP. At this time they are not widely used, nor recommended in current EASL or AASLD guidelines. However, they may play a role in facilitating prompt administration of antibiotic therapy, particularly in settings without available ascitic fluid microscopy testing.
CT scan abdomen
If perforation is suspected within the abdomen, CT imaging should strongly be considered.[103]Ross JT, Matthay MA, Harris HW. Secondary peritonitis: principles of diagnosis and intervention. BMJ. 2018 Jun 18;361:k1407.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6889898
http://www.ncbi.nlm.nih.gov/pubmed/29914871?tool=bestpractice.com
CT should also be considered in patients with findings suggestive of secondary peritonitis (such as bile-stained fluid, polymicrobial growth on ascites fluid culture, no clinical improvement despite appropriate antibiotics for 48 hours, and no history of liver disease or malignancy to explain the ascites) as it may demonstrate free air.[104]American College of Radiology. ACR appropriateness criteria: acute nonlocalized abdominal pain. 2018 [internet publication].
https://acsearch.acr.org/docs/69467/narrative
Clinical decision score
The chronic liver failure-sequential organ failure assessment (CLIF-SOFA) can help to determine the severity of illness in patients presenting with SBP. It is similar to the SOFA score, the predictive scoring system that assesses severity of illness in patients with sepsis. CLIF-SOFA has been shown to have better predictive value for in-hospital mortality in cirrhotic patients with infection compared to Sepsis-3 criteria or qSOFA.[105]Kim JH, Jun BG, Lee M, et al. Reappraisal of sepsis-3 and CLIF-SOFA as predictors of mortality in patients with cirrhosis and infection presenting to the emergency department: a multicenter study. Clin Mol Hepatol. 2022 Jul;28(3):540-52.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9293608
http://www.ncbi.nlm.nih.gov/pubmed/35526859?tool=bestpractice.com
Patients with CLIF-SOFA scores ≥7 have >20% mortality and so might benefit from broader empiric antibiotic therapy.[106]Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013 Jun;144(7):1426-37.
https://www.gastrojournal.org/article/S0016-5085(13)00291-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23474284?tool=bestpractice.com