Approach
Evaluation of pediatric abdominal pain can prove a diagnostic challenge. Children may be limited in their ability to give an accurate history. Parents or guardians may also have difficulty interpreting the complaints of small children. In many cases, the causes are benign with few long-term sequelae. However, some require rapid diagnosis and treatment in order to prevent significant morbidity or mortality. Consideration of the child's age helps narrow the differential diagnoses.[75]
History
The clinician should determine early on whether the abdominal pain is acute or chronic in nature, as this will help indicate the urgency of treatment. Acute abdominal pain is usually a single episode that typically lasts from hours to days. The pain may vary in severity over time and is often localized and described as sharp and/or stabbing in nature. Conversely, chronic abdominal pain typically lasts days to weeks to months, and is usually dull, diffuse, and poorly localized. There may be pain-free intervals of variable duration, and when it recurs the pain may vary in intensity.
In addition, the history should cover the following:
Age of the child
The age of the child affects some of the likely differential diagnoses:[19][104]
Neonates, infants, and toddlers: may present with abdominal pain caused by congenital causes or diseases linked to prematurity, such as necrotizing enterocolitis, Meckel diverticulum, Hirschsprung disease, volvulus, intestinal obstruction caused by congenital atresia, or stenosis. Intussusception is also common in this age group.
School-age children: idiopathic constipation and infectious causes of pain are most common in this age group. Functional abdominal pain and abdominal migraine may also present in school-age children.
Adolescents: conditions related to menstruation, sexually transmitted infections, and pregnancy should be considered. Testicular torsion, ovarian torsion, irritable bowel syndrome, and inflammatory bowel disease are more common in this age group.
Pain history
Useful mnemonics for abdominal pain are "CLAIR PRADER:" Characteristics, Location, Aggravating factors, Intensity, Relieving factors, Periodicity, Rhythmicity, Associations, Duration, Exacerbating factors, and Radiation; or "SOCRATES": Site, Onset, Character, Radiation, Associated Symptoms, Time course, Exacerbating or relieving factors, Severity.
Onset, frequency, timing, and duration of the pain episode.
Whether the pain is localized or diffuse: right lower quadrant (RLQ) pain suggests appendicitis; epigastric pain suggests peptic ulcer disease; diffuse pain may indicate perforation or peritonitis. Poorly localized pain that improves with movement is likely to be visceral pain from hollow organs. Well localized pain that worsens with movement is likely to arise from parietal peritoneum, parietal muscle, or skin.[105]
Whether the pain radiates or migrates between areas of the abdomen: abdominal pain radiating to the back is suggestive of cholecystitis or pancreatitis; pain that begins centrally and migrates to the RLQ is typical of appendicitis.
Any factors that make the pain better or worse, such as movement, defecation, food, or medication: in cholelithiasis/cholecystitis pain often occurs after eating (particularly fatty foods); epigastric pain due to peptic ulcer disease is usually related to eating meals; painful defecation may indicate constipation.
The character of the pain: pain associated with peptic ulcer disease is dull rather than burning in nature; sharp or stabbing pain is typical of appendicitis.
An acute exacerbation with a history of chronic pain can confound the diagnosis. It is important to determine if the nature of the acute pain is different (in character, location, or other factors) from the background, chronic pain. It is easy to miss or overlook an unrelated acute pathology in a patient with a chronic pain history of any sort (e.g., acute appendicitis in children with longstanding functional bowel complaints). The clinician must be wary of this trap, and there is no substitute for experience.
Associated symptoms
The clinician should enquire about the presence and severity of:
Fever, nausea, vomiting, anorexia (gastroenteritis, mesenteric adenitis)
Diarrhea (gastroenteritis)
Fatigue or jaundice (viral hepatitis)
Lethargy, headache, photophobia (abdominal migraine)
Cough, shortness of breath (pneumonia or empyema)
Pain elsewhere (e.g., sudden-onset testicular pain suggests testicular torsion)
Blood in stool (ulcerative colitis, necrotizing enterocolitis, dysentery, hemolytic uremic syndrome) or mucus in stool (suggests bacterial or parasitic infection)
Blood or bile in vomitus (small bowel obstruction)
Genitourinary symptoms: dysuria, frequency of micturition, and hematuria suggest a urinary tract infection (UTI); vaginal discharge is suggestive of pelvic inflammatory disease; current menstruation may be indicative of dysmenorrhea.
Trauma history
If there is a history of trauma, ascertain whether it is blunt or penetrating, and accidental or nonaccidental.
Travel history
Travel to a developing country increases risk of viral hepatitis infection and infectious gastroenteritis.
Stooling patterns and dietary history
The presence of bilious vomiting without passage of stool/flatus suggests complete small bowel obstruction. Bilious vomiting with passage of stool or flatus suggests partial small bowel obstruction.
Infrequent bowel action or fecal incontinence is suggestive of constipation. Infants may extend their legs and squeeze anal and buttock muscles to prevent stooling; toddlers often rise up on their toes, shift back and forth, and stiffen their legs and buttocks.
In addition to daily stooling pattern, evaluation of constipation includes pertinent medical history, onset of constipation symptoms, severity, and any previous treatments. Dietary history, paying attention to fiber and fluid intake, is helpful.
New or unusual food intake may support the diagnosis of gastroenteritis.
Past medical history (including birth and development)
This should focus on previous operations, medication use, immunizations, allergies, and current comorbidities; for example:
Patients with sickle cell disease or cystic fibrosis are at higher risk of developing gallstones
Patients with spina bifida, learning difficulties, or cerebral palsy are prone to constipation
Splenic infarction may be a consequence of sickle cell disease
Recent or current upper respiratory tract infection is suggestive of mesenteric adenitis or pulmonary cause
Failure to pass meconium in the first 36 hours of life is strongly suggestive of Hirschsprung disease
Hirschsprung disease can be associated with Down syndrome
Necrotizing enterocolitis should be considered in a premature neonate weighing less than 1500 g.
Drug history
Some medications, such as iron supplements, can cause constipation. Corticosteroids, adrenocorticotropic hormones, estrogens including contraceptives, azathioprine, asparaginase, tetracycline, chlorothiazides, and valproic acid may induce pancreatitis. Nonsteroidal anti-inflammatory drugs (NSAIDs), salicylates, and corticosteroids are associated with peptic ulcer development.
Family history
Positive family history is a risk factor for inflammatory bowel disease, nephrolithiasis, and functional abdominal pain.
Social and psychiatric history
This should include a discussion of family dynamics and may help determine if pain is functional or due to organic cause.
Psychological factors (e.g., depression, abuse, attention deficit disorder, oppositional disorder), weaning, toilet training, start of schooling, or other causes of stress may play a role in constipation.
History of nicotine, caffeine, or alcohol consumption may suggest peptic ulcer; excess alcohol consumption is a risk factor for pancreatitis.
Sexual history (in adolescents)
Adolescents may avoid answering sensitive questions regarding sexual history and drug use truthfully in the presence of parents or guardians; therefore, it may be appropriate to conduct some parts of the history with the adolescent alone.
Physical exam
This should be performed in a comfortable and nonthreatening manner. Children may need to be distracted by parents or guardians in order to obtain an accurate exam. In younger children, localization of the abdominal pain may be difficult.
Because pediatric abdominal pain may originate from other areas of the body (e.g., genitals or lungs), a comprehensive physical exam is necessary. Digital rectal exam is not routinely performed and is not needed to diagnose functional constipation.[106] UK guidelines recommend that digital rectal exam should only be performed by clinicians able to interpret features of anatomic abnormalities or Hirschsprung disease.[107] Pelvic exam is not routinely performed; history is usually a guide and digital exam should be reserved for adolescents who are sexually active.
All ages
Vital signs:
Consideration of vital signs should be based on age-appropriate normal values.
It is important to determine whether signs of volume depletion are present (tachycardia, hypotension, dry mucous membranes, poor capillary refill, sunken fontanel in infants). Children with gastroenteritis may quickly become volume depleted.
Fever may be the only presenting sign of a UTI, especially in the younger age group, and UTI should therefore be a top differential in children between 2 months and 2 years of age with fever.[108] High fever is suggestive of pyelonephritis.[108][109]
Cholecystitis, pancreatitis, and splenic infarction typically cause fever.
Patients with appendicitis do not usually have significant changes in vital signs. Body temperature may be increased by 1.8°F (1°C).
Children with constipation are usually well with normal vital signs.
Abdominal exam:
Patients presenting with central abdominal pain, with or without guarding and rigidity, that settles in the RLQ should arouse suspicion of appendicitis. Classic abdominal signs of appendicitis are RLQ abdominal tenderness (McBurney sign) and localized rebound tenderness, if the appendix is anterior. Compressing the left lower quadrant (LLQ) may elicit pain in the RLQ (Rovsing sign). Patients with appendicitis may lie still and try not to move, particularly in severe cases with significant peritoneal irritation.
Acute mesenteric adenitis often resembles acute appendicitis; however, pain in the abdomen is usually diffuse with tenderness not localized to the RLQ. Guarding may be present but rigidity is usually absent. One retrospective study found that, compared with children who have appendicitis, patients who have mesenteric adenitis are more likely to have high fever (above 102.2°F [39°C]) and dysuria, and are less likely to have migratory pain, vomiting, or typical abdominal signs of appendicitis on examination.[28]
Patients with gastroenteritis usually exhibit diffuse abdominal pain without evidence of peritonitis (no guarding or rebound tenderness). Abdominal distension and hyperactive bowel sounds are common findings.
The presence of abdominal distension and tenderness associated with decreased or absent bowel sounds is strongly suggestive of large bowel obstruction. In severe cases of constipation, abdominal distension may be present with a palpable fecal mass per abdomen or rectum.
Flank pain or costovertebral angle tenderness may indicate pyelonephritis or nephrolithiasis.
Epigastric pain may indicate peptic ulcer disease or pancreatitis. Patients with pancreatitis may lie with their knees and hips flexed and avoid moving. It is important to note that, in younger patients with pancreatitis (<3 years of age), abdominal tenderness may not be the main finding; these patients may demonstrate increased irritability and abdominal distension. With hemorrhagic pancreatitis, discoloration may be noted around the umbilical area (Cullen sign) or in the flanks (Grey-Turner sign) due to blood tracking along defined fascial planes.
Tenderness in the right upper quadrant (RUQ) is a classic sign of gallbladder disease, as is Murphy sign (cessation of inspiration during concurrent deep RUQ palpation). Patients with biliary dyskinesia usually present in a similar fashion to those with cholelithiasis and cholecystitis and may have RUQ tenderness on palpation.
Patients with splenic infarction typically present with left-sided abdominal pain and fevers. Pain may also be reported in the left side of the chest or the left shoulder. Those with a splenic cyst are either asymptomatic or present with dull left-sided abdominal pain in the absence of fever.[110]
In trauma patients, signs of accidental (e.g., seat belt mark suggesting a motor vehicle accident) and nonaccidental injury (particularly if history is suspicious) should be sought (e.g., cigarette burns, subdural hemorrhages in an infant/young toddler). The presence of seat belt marks increases the likelihood that intra-abdominal injuries are present, particularly in the presence of lumbar fracture or persistent tachycardia.[111]
If clinical findings are minimal and the child appears well, a diagnosis of functional abdominal pain should be considered. Diagnostic criteria for functional abdominal pain are symptom based, not physical exam or laboratory based.[71]
Signs of peritonitis, such as absent bowel sounds, bilious vomiting, bloody diarrhea or occult blood in stool, fever (≥100.4°F [≥38°C]), rebound tenderness, rigidity, and guarding indicate a possible need for surgery.
External genital and perineal exam:
A neonatal exam must evaluate for the presence of an anus along with the proper location within the sphincter complex.
Testicular torsion is likely in any male child with abdominal tenderness plus loss of the cremasteric reflex, diffuse testicular tenderness, elevated testes, and a horizontal rather than vertical position of the testes on exam.
Blood at the urethral meatus, or hematuria, after trauma may suggest urinary tract or kidney injury.
The presence of an anal fissure and/or hemorrhoids (rare in children; may be mistaken for skin tags from Crohn disease), imperforate anus, or anal stenosis (particularly in a neonate or infant) on inspection of the perianal skin may provide further diagnostic clues.
General examination:
Generalized lymphadenopathy is common and signs of an upper respiratory tract infection may be present in children with mesenteric adenitis (e.g., hyperemic pharynx or oropharynx suggesting pharyngitis).
Jaundice is rare with cholelithiasis or acute cholecystitis and, if present, suggests an obstruction of the common bile duct. Jaundice associated with abdominal tenderness, hepatomegaly (splenomegaly may also be present), and lymphadenopathy, particularly in a child of school age, should arouse suspicion of viral hepatitis (commonly hepatitis A).
Children with spina bifida, learning difficulties, and cerebral palsy are prone to constipation, and features of these conditions may be obvious on exam (e.g., sacral dimples or pits and/or tags/tufts indicative of abnormality of spinal cord).
Henoch-Schonlein purpura (HSP) may be the initiating factor in an older child with abdominal pain (usually <11 years of age), and therefore signs of HSP should be sought (rash of palpable purpura, blood in the stools).
Extraintestinal manifestations of inflammatory bowel disease may be evident (e.g., iritis, arthritis, sacroiliitis, erythema nodosum, pyoderma gangrenosum).
The presence of cyanosis, tachypnea, decreased breath sounds on auscultation, dullness on percussion (indicates consolidation), and abdominal tenderness and distension without guarding or rebound should arouse suspicion of a pulmonary cause such as pneumonia or empyema.
Infants and toddlers
In a neonate, the triad of abdominal distension, delayed passage of meconium (not occurring in the first 36 hours of life), and vomiting is highly suggestive of Hirschsprung disease.
Necrotizing enterocolitis should be considered in a premature neonate weighing less than 1500 g. Early signs may include inability to tolerate feeds, abdominal distension and tenderness, blood in the stool, and abdominal wall erythema. In severe cases, systemic signs of sepsis may be present.
A neonate presenting with bilious vomiting, with (partial obstruction) or without (complete obstruction) the passage of meconium, is highly suggestive of small bowel obstruction. Causes such as meconium ileus, intestinal atresia, and midgut volvulus should be excluded with further investigations.
Any abdominal exam of an infant and toddler must include a check for inguinal hernias; if a diaper is worn, remove it, as otherwise a hernia may be missed.
Meckel diverticulum should be considered in a child <2 years old with abdominal tenderness (Meckel diverticulitis); hematochezia, typically dark red, maroon, or red-brick-colored jelly-like stools (indicates intestinal bleeding as they contain heterotopic gastric tissue); or signs of obstruction such as nausea, vomiting, and constipation (intussusception, volvulus, or herniation can result).
Reproductive age
Ectopic pregnancy and miscarriage should be suspected in any female of reproductive age presenting with lower abdominal pain, amenorrhea, and vaginal bleeding. Pelvic exam may reveal a mass, eliciting cervical motion tenderness if hemoperitoneum is present; tubal rupture can cause hemodynamic instability.
Clinical features of a ruptured ovarian cyst usually occur prior to the expected time of ovulation and may mimic ectopic pregnancy. Pain arises from local peritonitis secondary to hemorrhage.[56][57][58] Signs of peritonitis may be present in the lower abdomen and pelvis; adnexal size is unremarkable due to collapsed cyst.
The presence of a tender pelvic mass associated with nausea and vomiting may suggest ovarian torsion. In addition, in patients old enough to undergo pelvic exam, cervical motion tenderness may be elicited; typically no vaginal discharge is present, but there may be some mild to moderate vaginal bleeding.
Physical findings of pelvic inflammatory disease (PID) vary widely and may include lower abdominal tenderness, adnexal tenderness, and cervical motion tenderness.[62] Fever and cervical or vaginal discharge may also be present. PID is rare in the absence of sexual activity; PID in a young child should prompt workup for possible sexual abuse.
Patients with PID may also present with RUQ pain resulting from inflammation of the liver capsule or diaphragm, referred to as Fitz-Hugh-Curtis syndrome. This is secondary to an ascending infection. Referred pain to the right shoulder may result from irritation of the diaphragm.[112]
Primary dysmenorrhea should be considered if lower abdominal tenderness is associated with current menstruation.
Laboratory tests
Challenges in the clinical evaluation of abdominal pain in the pediatric patient mean laboratory and imaging studies can play an important role.
Urinalysis is essential to exclude underlying UTI or hematuria (associated with nephrolithiasis, UTI, hemolytic uremic syndrome, urinary tract or kidney injury) and should be performed in children of all ages presenting with abdominal pain. For females of reproductive age a urine pregnancy test and/or serum human chorionic gonadotropin (beta-hCG) is necessary to exclude miscarriage and ectopic pregnancy.
Initial blood and stool tests may include:
CBC, recommended in all patients (useful in evaluating infection and inflammation).
Complete chemistry panel, recommended in all patients (electrolyte disturbances associated with GI causes are common).
Blood type and screen and rhesus status when ectopic pregnancy is suspected.
Liver function tests (LFTs) are helpful baseline investigations when considering a hepatobiliary or pancreatic cause. In abdominal trauma, results from one retrospective study suggest that LFTs may be used as a screening tool to determine need for computed tomography (CT) scan; in a hemodynamically normal patient with normal AST/ALT, it may be possible to avoid CT scan.[113]
Serum lipase, or amylase if lipase is unavailable, is indicated if pancreatitis is suspected.[114]
Inflammatory markers. Although nonspecific, erythrocyte sedimentation rate and C-reactive protein may suggest underlying infection or inflammation. Furthermore, these inflammatory markers correlate closely with disease activity in cases of inflammatory bowel disease.
A positive fecal occult blood test can support a suspicion of intussusception. However, a negative test cannot reliably rule out the diagnosis.[115]
Fecal calprotectin is used in the diagnosis and monitoring of inflammatory bowel disease and to distinguish it from functional gastrointestinal disorders.[116]
A coagulation profile, including prothrombin time and international normalized ratio (INR), is usually necessary in cases of suspected viral hepatitis to measure liver synthetic function.
Microbiologic investigations
Stool microscopy and culture may be helpful in determining an infectious etiology of gastroenteritis. Risk factors and features of the clinical presentation help guide the choice of tests for specific pathogens. Guidelines recommend that when there is fever or bloody diarrhea, investigations for enteropathogens for which antimicrobial agents may confer clinical benefit (including Salmonella enterica subspecies, Shigella, and Campylobacter) should be done.[117]
Blood cultures are indicated when sepsis is a concern. Blood cultures are recommended: in children with infectious diarrhea who are <3 months of age or who are immunocompromised; when enteric fever is suspected (including travel to enteric fever-endemic area, or contact with travelers from enteric fever-endemic areas who have a febrile illness of unknown etiology); when there are systemic manifestations of infection; and with high-risk conditions such as hemolytic anemia.[117][118]
Urine culture is necessary if urinalysis is suggestive of a UTI.
Sputum culture is indicated in patients with suspected pneumonia. Aspiration of frank pus on thoracentesis is diagnostic of empyema.
In cases of patients with suspected peptic ulcer disease, Helicobacter pylori breath test or stool antigen test may be helpful.[119][120]
Serologic markers (perinuclear antineutrophil cytoplasmic antibody and antisaccharomyces cerevisiae antibody) may be particularly useful for differentiating between Crohn disease and ulcerative colitis in the pediatric population.[121][122]
Polymorphonuclear leukocytes (PMNs) seen on wet mount of vaginal secretions confirms vaginal infection in cases of PID. All women who receive a diagnosis of PID should be tested for gonorrhea, chlamydia, HIV, and syphilis.[62] Hepatitis studies may be considered.
In patients with suspected exposure to or symptoms of hepatitis A, B, C, D, and E, the following laboratory tests are warranted: hepatitis A antibody IgM, hepatitis B surface, core, and e antigen or viral load, hepatitis C serology or viral load, hepatitis D and E serologies.
Imaging and other investigations
Imaging studies are guided by history and physical exam findings.
Abdominal and chest x-ray
Plain abdominal x-rays are often nonspecific but may suggest the presence of an obstruction; fecal impaction and duodenal atresia can be detected on x-ray. In addition, if sufficiently radiopaque, it may be possible to identify gallstones or urinary stones on a plain abdominal film. This is often the initial test, as it can be performed quickly. Supine and upright films are usually requested. Free air under the diaphragm suggests perforation and requires immediate surgical evaluation. Chest x-ray should be ordered if perforation is suspected or a respiratory cause such as pneumonia or empyema is likely.
Ultrasound
Ultrasound scans avoid radiation exposure and are typically better tolerated than other imaging modalities such as computed tomography (CT) scan. An experienced pediatric radiologist may be able to utilize ultrasound in all regions of the body (abdomen, chest, testicles). Abnormalities detected by ultrasound may not be causally related to the patient's abdominal pain.[74]
Ultrasound is usually recommended as the first imaging test for suspected appendicitis.[76][78] Ultrasound scans are considered particularly useful in evaluating pain in the RUQ (i.e., gallbladder disease), and lower abdominal pain (pelvic pain) in females.
Color Doppler may be helpful in determining ovarian blood flow in cases of suspected ovarian torsion, but is of only variable reliability in the diagnosis.[87][88] Testicular ultrasound (using duplex Doppler ultrasound) should be able to diagnose testicular torsion and provide information on the vascular integrity of the testis.
Ultrasound of the urinary tract (including kidneys) is of benefit when wanting to exclude anatomic abnormalities (e.g., when UTI is present) or nephrolithiasis and associated complications such as hydronephrosis.
Point-of-care ultrasound may be useful for detecting intussusception at an early stage.[123][124]
Focused abdominal sonography for trauma (FAST) may be useful in children with blunt abdominal trauma who are hemodynamically unstable.[125] The presence of large amounts of free fluid indicates a need for immediate operative intervention. FAST in hemodynamically stable patients has a less certain impact, as a negative scan does not preclude injury. A large multi-institutional study at pediatric trauma centers demonstrated poor FAST sensitivity (28.6%) in normotensive patients.[126] Though specificity was high (91.1%), results of FAST rarely changed management. A randomized trial comparing FAST with standard care in hemodynamically stable children and adolescents with blunt torso trauma also found no significant difference in the proportion of abdominal CT scans, missed intra-abdominal injuries, length of stay in the emergency department, and median hospital costs.[127]
Abdominal CT scan with intravenous contrast is the diagnostic test of choice for the identification of solid organ injuries, especially to the liver, kidney, and/or spleen. Oral contrast is usually not necessary when scanning a patient for trauma.
CT and magnetic resonance imaging (MRI)
CT with contrast may be appropriate in investigating suspected appendicitis if ultrasound is nondiagnostic; however, radiation exposure with its risk of malignancy should be considered.[78][128][129] MRI avoids ionizing radiation and has similar or better sensitivity and specificity than CT, though availability and longer scan times may limit its utility.[78][130][131] Increasingly, MR enterography (MRE) is being used to evaluate pediatric Crohn disease patients. This tool can evaluate extraluminal and extraintestinal manifestations of Crohn disease as well as the status of the bowel wall and presence of possible stricture formation.[132]
In general, for investigation of abdominal pain in children, CT scan of the abdomen and pelvis, with or without contrast, may provide a high yield of information, but radiation exposure should be considered.[133] Sedation or general anesthesia may be required in some children.
GI contrast studies (upper-GI or barium enema studies) are routinely used in place of CT scans, especially in infants. In evaluation of intestinal obstruction, clinical suspicion should direct which contrast study should be performed first and will be most informative.
Endoscopy
Endoscopy (esophagogastroduodenoscopy or colonoscopy) with biopsy may be required to evaluate mucosa-based diseases, such as peptic ulcer disease and inflammatory bowel disease. Rectal biopsy and anorectal manometry help confirm the diagnosis of Hirschsprung disease. These procedures may be particularly challenging when performed in a newborn.
Nuclear medicine scans
Diagnosis of biliary dyskinesia is confirmed by hepatobiliary iminodiacetic acid (HIDA) scan with an ejection fraction <35%. It is important to note that the cutoff of <35% is not universally accepted; some consider an ejection fraction <15% to be more predictive of success of surgical treatment (i.e., cholecystectomy).[134] Hyperkinetic results (very high ejection fractions) are sometimes considered an indication for cholecystectomy, as are normal scans (at some institutions). Outcomes vary widely among pediatric biliary dyskinesia patients. In retrospective studies, overall rates of symptom resolution post operation ranged from 34% to 100%.[135][136] The absence of reliable factors to predict which patients will benefit is a source of frustration to patients, families, and physicians. HIDA scan is considered a useful adjunct in the diagnosis of cholecystitis.
Technetium-99m pertechnetate scan is considered the most useful method to diagnose a suspected Meckel diverticulum; this scan identifies ectopic gastric mucosa as tracer is taken up by gastric mucin-producing cells.
Voiding cystourethrogram
The American Academy of Pediatrics (AAP) recommends that a voiding cystourethrogram is indicated in children between 2 and 24 months of age following an initial UTI if renal and bladder ultrasonography reveals hydronephrosis, scarring, or other findings that would suggest either high-grade vesicoureteral reflux or obstructive uropathy, as well as in other atypical or complex clinical circumstances.[137] Further evaluation is required if there is a recurrence of febrile UTI.[137][138][139]
Full skeletal x-rays
Skeletal survey identifies previous skeletal injuries and should be obtained if there is a high suspicion of nonaccidental trauma. This should only be performed to provide adjunctive diagnoses to support an initial injury and suspicion of abuse.
Diagnostic laparoscopy
Laparoscopy may be necessary to confirm diagnosis of pelvic inflammatory disease as it allows direct visualization of the gynecologic and abdominal structures.
[Figure caption and citation for the preceding image starts]: Abdominal x-ray of a neonate with abnormal stooling pattern and constipation. The dilated transverse and descending colon is suggestive of Hirschsprung diseaseFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Abdominal x-ray demonstrating double bubble gas pattern consistent with duodenal atresiaFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Abdominal x-ray demonstrating double bubble gas pattern consistent with duodenal atresiaFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Abdominal x-ray with opacities in the RUQ consistent with gallstonesFrom the collection of Dr Kuojen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Abdominal x-ray with opacities in the RUQ consistent with gallstonesFrom the collection of Dr Kuojen Tsao; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Gallbladder ultrasound demonstrating cholelithiasis with characteristic shadowingFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Gallbladder ultrasound demonstrating cholelithiasis with characteristic shadowingFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan demonstrating fecalith (white arrow) outside the lumen of the appendix consistent with perforated appendixFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan demonstrating fecalith (white arrow) outside the lumen of the appendix consistent with perforated appendixFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].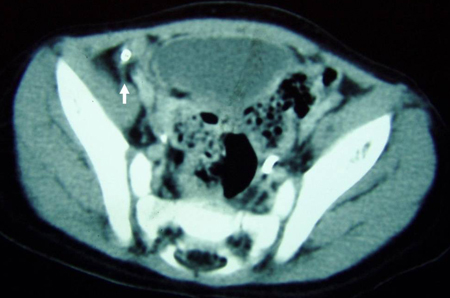 [Figure caption and citation for the preceding image starts]: Contrast enema demonstrating ileocolic intussusception (black arrow)From the collection of Dr KuoJen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Contrast enema demonstrating ileocolic intussusception (black arrow)From the collection of Dr KuoJen Tsao; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan of teenage girl presenting with mid-epigastric abdominal pain as a result of gallstone pancreatitis. The large fluid collection in the pancreatic bed (white arrow) and lack of pancreatic enhancement suggest liquefactive necrosis of the pancreasFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of teenage girl presenting with mid-epigastric abdominal pain as a result of gallstone pancreatitis. The large fluid collection in the pancreatic bed (white arrow) and lack of pancreatic enhancement suggest liquefactive necrosis of the pancreasFrom the collection of Dr KuoJen Tsao; used with permission [Citation ends].
How to insert a peripheral intravascular catheter into the dorsum of the hand.
How to take a venous blood sample from the antecubital fossa using a vacuum needle.
Use of this content is subject to our disclaimer

