Aetiology
Aetiologies include infective causes (bacterial, viral, fungal and parasitic), immune-mediated and inflammatory conditions, drug reactions, and idiopathic conditions.
Infectious causes
Bacterial infections
Impetigo is caused by group A beta-haemolytic streptococci or Staphylococcus aureus. Impetigo can occur as a primary infection or secondary to pre-existing skin conditions, such as eczema or scabies. It has 2 forms: bullous and non-bullous.[1] Bullous impetigo is toxin mediated.[Figure caption and citation for the preceding image starts]: Neonate with bullous impetigoFrom the collection of Michael Freeman; used with permission [Citation ends].
 Non-bullous impetigo is the most common paediatric skin infection; it usually starts as a pink macule, which develops into a pustule or vesicle then forms a characteristic golden crust. In a study in the UK, the annual incidence of impetigo was 2.8% in children up to 4 years of age and 1.6% in children 5 to 15 years of age.[2]
Non-bullous impetigo is the most common paediatric skin infection; it usually starts as a pink macule, which develops into a pustule or vesicle then forms a characteristic golden crust. In a study in the UK, the annual incidence of impetigo was 2.8% in children up to 4 years of age and 1.6% in children 5 to 15 years of age.[2]Ecthyma is a deeper, ulcerated infection that may occur with lymphadenitis and is part of the differential diagnosis for non-bullous impetigo.[3]
Folliculitis is a pyoderma located within a hair follicle, secondary to follicular occlusion by keratin, over-hydration, or infection (bacterial, viral, or fungal).[4][Figure caption and citation for the preceding image starts]: Superficial folliculitis with prominent erythematous papules and pustulesFrom the collection of Dr Professor Baden; used with permission [Citation ends].
 Presentations vary. Bacterial examples include Pseudomonas folliculitis, resulting from bacterial colonisation of hair follicles after exposure to contaminated water, for example, in hot tubs, swimming pools, and saunas; and Staphylococcus aureus folliculitis, a common pathogen related to a superficial follicular infection.[4] Staphylococci occasionally invade the deeper portion of the follicle, causing a deep folliculitis.[4]
Presentations vary. Bacterial examples include Pseudomonas folliculitis, resulting from bacterial colonisation of hair follicles after exposure to contaminated water, for example, in hot tubs, swimming pools, and saunas; and Staphylococcus aureus folliculitis, a common pathogen related to a superficial follicular infection.[4] Staphylococci occasionally invade the deeper portion of the follicle, causing a deep folliculitis.[4]Gram-negative folliculitis results from prolonged antibacterial treatment when gram-negative bacteria replace gram-positive flora of the facial skin and the mucous membranes of the nose. These gram-negative bacteria include Escherichia coli, Pseudomonas aeruginosa, Serratia marcescens, Klebsiella, and Proteus mirabilis.[5]
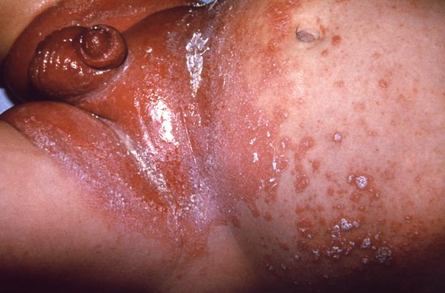
Secondary syphilis is caused by the spirochete Treponema pallidum. It is almost always transmitted by sexual contact or vertical transmission. It classically arises 6 to 10 weeks after the painless chancre of primary syphilis resolves. Secondary syphilis manifests as a mucocutaneous rash in association with vague constitutional symptoms, diffuse lymphadenopathy, and highly infectious skin lesions. The rash may have any morphology, except vesicular.[6][Figure caption and citation for the preceding image starts]: Secondary syphilitic lesions on the facePublic Health Image Library, CDC [Citation ends].
 Lesions result from the haematogenous dissemination of treponemes from syphilitic chancres. The US Centers for Disease Control and Prevention (CDC) reported that in 2018, the rate of primary and secondary syphilis in the US was 10.8 cases per 100,000 population.[7]
Lesions result from the haematogenous dissemination of treponemes from syphilitic chancres. The US Centers for Disease Control and Prevention (CDC) reported that in 2018, the rate of primary and secondary syphilis in the US was 10.8 cases per 100,000 population.[7]
Viral infections
Herpes simplex virus (HSV) can cause primary and recurrent infections. The rash usually starts as a vesicular rash and then becomes pustular. HSV-1 is responsible for most cases of herpes labialis. Urogenital herpes is generally caused by HSV-2. In the US, the estimated prevalence of HSV-1 and HSV-2 in people aged 14 to 49 years is 8% and 12%, respectively.[8] Transmission is by direct skin-to-skin contact. The incubation period ranges from 2 to 20 days in patients experiencing a primary infection. Re-activation of latent herpetic infection from neural ganglia is often heralded by a tingling or burning sensation before the appearance of any overt skin changes. Re-activation may be triggered by physical or emotional stress, UV radiation, fever, or immunosuppression.[9]
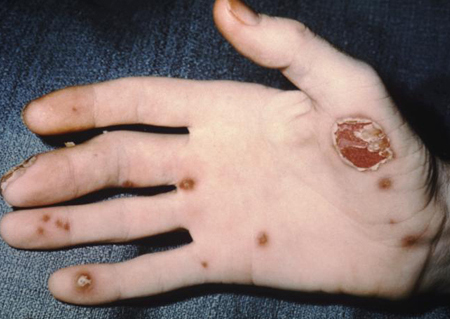
Ecthyma contagiosum, also termed Orf, is a DNA parapox viral disease. It usually infects sheep and goats. Humans become infected following contact with lesions on animals or contaminated fomites. It is commonly known as a professional disease of shepherds, farmers, and veterinarians. The virus incubates for less than 4 weeks, with the infection resolving in 6 weeks after onset.[10]
Fungal infections
Folliculitis: Pityrosporum folliculitis is a follicular infection caused by overgrowth of the yeast Malassezia furfur that thrives in a sebaceous environment. Eruptions are associated with conditions that alter the skin flora, such as immunosuppression and antibiotic use. It presents as a pruritic eruption of follicular papules and pustules, often on the upper back, chest and shoulder.[11]
Candidal infection and disseminated candidiasis: disseminated candidiasis is defined as candidal infection in sterile target organs, with or without positive blood culture results.[12]
Invasive candidiasis is a problem of increasing relevance in the healthcare setting and in particular for ICUs. Candidal invasion can occur through a break in the skin or mucosa, which is then colonised, and/or via the gastrointestinal wall, where organisms pass directly into the bloodstream.[13]
Risk factors associated with invasive candidiasis include Candida colonisation, treatment with broad-spectrum antibiotics, central venous catheter, parenteral nutrition, gastrointestinal or cardiac surgery, prolonged hospital stay, ICU stay, burns, necrotising pancreatitis, dialysis, premature birth, and immunosuppression (caused by neutropenia, corticosteroid treatment, HIV infection, and diabetes mellitus).[12]
Papulopustular satellite lesions develop when candida affects a skin fold.
Congenital cutaneous candidiasis presents at birth or in the first few hours of life; it can occur in extremely low birth weight infants (under 1000 g).[14]
[Figure caption and citation for the preceding image starts]: Infant presenting with rash formerly known as moniliasis, now called candidiasis, caused by Candida sppPublic Health Image Library, CDC [Citation ends].
Dermatophytosis: Because dermatophytes require keratin for growth, they are restricted to hair, nails, and superficial skin.[Figure caption and citation for the preceding image starts]: Tinea manuum. On the extensor surface of the hand there is extensive inflammation, scaling, hyperkeratosis, and erythemaDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Tinea corporis of the axilla. Central clearing with an active border of inflammation noted. Satellite lesion is presentDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Tinea corporis of the axilla. Central clearing with an active border of inflammation noted. Satellite lesion is presentDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Tinea barbae. Note the pustules in the follicles, redness, and scalingDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Tinea barbae. Note the pustules in the follicles, redness, and scalingDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends]. Thus, these fungi do not infect mucosal surfaces. Dermatophytoses are referred to as 'tinea' infections. They are also named for the body site involved.[15] Tinea infections typically cause circumscribed scaly lesions, but pustules can occur.
Thus, these fungi do not infect mucosal surfaces. Dermatophytoses are referred to as 'tinea' infections. They are also named for the body site involved.[15] Tinea infections typically cause circumscribed scaly lesions, but pustules can occur. In tinea pedis fissuring permits streptococci to colonise web spaces between the toes. Clinical features of symptomatic athlete's foot are caused by interaction of fungi and bacteria.[Figure caption and citation for the preceding image starts]: Tinea pedis. Intense inflammation produces hyperpigmentation and vesicle formation. Vesiculobullous form of tinea pedisDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].
 Bullous tinea pedis may occur on feet, usually on the soles, and presents with vesicles, pustules, and sometimes bullae.[15] Clinical presentation depends on the anatomical site and aetiological agents.
Bullous tinea pedis may occur on feet, usually on the soles, and presents with vesicles, pustules, and sometimes bullae.[15] Clinical presentation depends on the anatomical site and aetiological agents.
Parasitic infections
Infantile scabies is caused by infestation by Sarcoptes scabiei.[16][Figure caption and citation for the preceding image starts]: Scabies: characteristic linear burrows in skinFrom the collection of Dr Laura Ferris; used with permission [Citation ends].
 Scabies in infants and young children differs from infection in adulthood. Scabies rarely affects the skin above the neck in adults. In infants and children, scabies can affect the entire body, including the palms, soles of the feet, and head and scalp. In infants, scabies can manifest as sterile pustules on the palms and soles.
Scabies in infants and young children differs from infection in adulthood. Scabies rarely affects the skin above the neck in adults. In infants and children, scabies can affect the entire body, including the palms, soles of the feet, and head and scalp. In infants, scabies can manifest as sterile pustules on the palms and soles.
Immune-mediated and inflammatory conditions
This group of rashes can occur in inherited or acquired inflammatory conditions. The diseases in this group vary in terms of the presentation of the rash.
Acne vulgaris:
Multi-factorial disease affecting the pilosebaceous unit. Prevalence in adolescents and young adults approaches 60%.[17]
The interaction of 4 main pathogenic factors leads to its development. These are 1) the production of sebum by androgen-mediated stimulation of sebaceous glands, 2) abnormal hyper-keratinisation of the follicles leading to follicular plugging and comedone formation, 3) colonisation of the pilosebaceous unit by the gram-positive bacterium Propionibacterium acnes, and (4) stimulation of an inflammatory cascade and release of inflammatory mediators by P acnes into the follicle and surrounding dermis.[18]
Acne morphology is variable and includes pustules, papules, open and closed comedones, nodules and pseudocysts. [Figure caption and citation for the preceding image starts]: Nodulocystic acneUniversity of Michigan Department of Dermatology [Citation ends].

Congenital adrenal hyperplasia, polycystic ovarian syndrome, and other endocrine disorders with excess androgens may trigger the development of acne vulgaris.[18]
Medications that can promote acne include corticosteroids, lithium, some antiepileptics, and iodides.[19]
Eosinophilic folliculitis:
A descriptive histopathological term applied to a heterogeneous group of disorders occurring as a result of an autoimmune process directed against the sebocytes, or some component of the sebum. The characteristic histopathological features are eosinophilic spongiosis and pustulosis involving the infundibular region of the hair follicle.
Can be associated with the following conditions: Ofuji's disease, seen often in Japanese males; patients with AIDS and other conditions of immunosuppression; and in infants, usually within the first 24 hours of life.[20][21]
Behcet's disease:
Chronic relapsing multi-system disease of unknown aetiology.
Patients from the Middle East, Mediterranean region and eastern Asia are most commonly affected. The prevalence in North America and Europe is 1 case per 15,000-500,000 population. [22]
Characterised by recurrent aphthous stomatitis, genital ulcerations, and ocular disease, as well as mucocutaneous, articular, neurological, urogenital, vascular, intestinal, and pulmonary manifestations.[23]
Skin lesions may be papulopustular, nodular or acneiform. Acneiform lesions are similar to acne vulgaris but may arise in atypical locations, such as arms and legs. [Figure caption and citation for the preceding image starts]: Mouth and genital ulcers in Behcet's diseaseFrom the collection of Dr Yusuf Yazici; used with permission [Citation ends].
Pseudofolliculitis barbae (also known as pili incarnati, folliculitis barbae traumatica, and sycosis barbae):
Common dermatological condition affecting men and women of black and Hispanic origin who have tightly coiled hair.
Not a true folliculitis, in that a pathogenic microorganism is not involved in its aetiology. Rather, the basis of its aetiology is an inflammatory reaction to a hair shaft, and the shape, direction, and nature of its growth. After shaving, the sharp edge of the hair shaft transects the wall of the hair follicle or re-enters the epidermis. The same mechanism occurs in certain hair-bearing areas (scalp, axillae, pubis, and legs) of predisposed people who shave, tweeze, or wax hairs.[26] Pustules and papulopustules are thought to be secondary lesions caused by infection with Staphylococcus epidermidis.[26]
Sub-corneal pustular dermatosis (Sneddon-Wilkinson's disease):
Benign inflammatory skin disorder of unknown aetiology. It is associated with various systemic disorders, including immunoglobinopathies and lymphoproliferative disorders.[27]
In sub-corneal pustular dermatosis type IgA pemphigus, the target of these IgA autoantibodies is desmocollin 1. It is characterised by intra-epidermal neutrophilic pustules and intercellular IgA deposition, and resembles IgA pemphigus.
Infantile acropustulosis (IA):
Condition of young children characterised by recurrent episodes of pruritic vesicles and pustules in an acral distribution.
It begins in infancy and resolves at around 2 to 3 years of age. Most cases occur after scabies infestation. One study showed co-existence of atopic dermatitis in over 50% of IA cases.[28][29]
Erythema toxicum neonatorum:
Acute, self-limiting skin manifestation that develops in 50% to 70% of all healthy newborn infants, particularly those born at term. It starts soon after birth and disappears spontaneously within a few weeks without sequelae.
Its aetiology is uncertain. It is a non-infectious condition and has been attributed to haematological, toxic, and allergic factors.[30][31]
Fire ant bites:
Predominant species is Solenopsis invicta. The ant usually nests in mounds formed in the ground.[Figure caption and citation for the preceding image starts]: Pseudopustule formation following fire ant stingFrom the collection of Theodore Freeman; used with permission [Citation ends].

The venom of the fire ant contains aliphatic substituted alkaloids that are cytotoxic. These compounds cause the epithelial damage that results in the sterile pustule. Fire ant venom also contains the enzyme hyaluronidase, which could activate the complement, coagulation, or kinin systems in some people.[32]
Neonatal cephalic pustulosis:
This is a pustular eruption arising on the face and/or scalp of newborn babies, usually during the third week of life.
Benign cephalic pustulosis is differentiated from infantile acne by its lack of comedonal lesions and earlier onset.[33]
Miliaria rubra or 'prickly heat':
Presents in over-heated and febrile infants.[33] It affects up to 40% of infants and usually appears during the first month of life.[34] It also presents uncommonly in adults.[35][Figure caption and citation for the preceding image starts]: Miliaria rubraFrom the collection of Brian L. Swick; used with permission [Citation ends].

Deeper intra-epidermal occlusion of the eccrine duct causes mild inflammation, producing the erythema associated with miliaria rubra.[33]
Rosacea:
Chronic dermatosis characterised by facial flushing, erythema, telangiectasia, inflammatory episodes with papules and pustules, and, in severe cases, rhinophyma.[36][Figure caption and citation for the preceding image starts]: Rosacea fulminansCourtesy of Dr Richard Allen Johnson (MD, CM. Harvard Medical School); used with permission [Citation ends].

Most commonly manifests in patients between the ages of 30 and 60 years. Rosacea affects as many as 14 million people in the US.[37]
Four different sub-types (erythematotelangiectatic, papulopustular, phymatous, and ocular rosacea) describe the most common patterns of signs.[36]
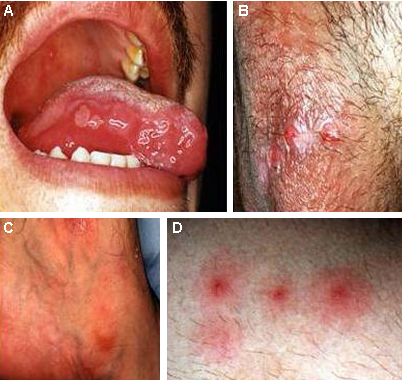
Reactive arthritis:
Genetic disease which may be related to HLA-B27. In addition, there is familial clustering with other seronegative spondylarthropathies. It results from an immune response, usually after an infection of the gastrointestinal or urinary tract.[Figure caption and citation for the preceding image starts]: Pustules in a patient with reactive arthritisPublic Health Image Library, CDC [Citation ends].
Associated enteric organisms include Shigella flexneri (types 2a and 1b), Salmonella typhimurium, Salmonella paratyphi, Salmonella cholerae, Salmonella suis, Salmonella enteritidis, Salmonella heidelberg, Yersinia enterocolitica, Yersinia pseudotuberculosis, Campylobacter fetus, Campylobacter jejuni, and Clostridium difficile.[38]
Associated urogenital organisms include Ureaplasma urealyticum, Chlamydia psittaci, Chlamydia trachomatis (D-K), and Neisseria gonorrhoeae.[38]
Acrodermatitis continua of Hallopeau (ACH):
Chronic skin disorder characterised by recurrent, sterile, pustular eruptions of the digits with marked involvement of the nail beds. ACH can be precipitated by trauma or infection.
Typically begins on 1 digit, but other digits may become involved during the chronic course of the disease. The intermittent pustulations may lead to atrophy, onychodystrophy, and even osteolysis. Furthermore, the lesions can be very painful and disabling.
The pathomechanism of this rare disease is still unknown, but most authors consider it to be a variation of pustular psoriasis rather than a separate entity.[39]
Peri-oral dermatitis:
Chronic facial eruption characterised by grouped reddish papules, papulovesicles, and papulopustules over an erythematous area around the mouth.
Although peri-oral is the most frequent location, the peri-ocular areas, nasolabial folds, and glabella may also be affected.[40]
Peri-oral dermatitis usually occurs in children and in young women between 20 and 45 years of age.
Aetiology is still unknown, although many factors have been proposed, such as contact allergy, hormonal factors, cosmetics, topical or systemic corticosteroids, pregnancy, malabsorption, infective agents (e.g., Candida, Demodex, Fusobacterium species), skin barrier disorders, or atopy.[40]
Infective agents have been implicated in pathogenesis, a proliferation of skin flora (e.g., fusiform bacteria) possibly being supported by overuse of cosmetic products.
Amicrobial pustulosis of the folds (APF):
A relapsing condition of pustular lesions predominantly involving the cutaneous flexures and scalp.
This syndrome typically occurs in association with an autoimmune or connective tissue disease, including SLE, scleroderma overlap syndrome, discoid lupus erythematosus, sicca syndrome, coeliac disease, idiopathic thrombocytopenia, or myasthenia gravis.[41]
An amicrobial pustulosis-like rash has been reported in a patient with Crohn’s disease on anti-TNF-alpha blocker therapy.[42]
Drug related
Drug rashes and the drugs implicated in causing a pustular rash include the following:
Epidermal growth factor receptor (EGFR) inhibitors (such as cetuximab, erlotinib, and gefitinib) are used to treat colorectal and non-small cell lung cancers refractory to chemotherapy.[43] They can cause a sterile follicular and pustular rash, which can be a visible marker of therapeutic efficacy.[43][44] The rash onset is between weeks 1 and 3 of treatment, peaking between weeks 3 and 5, and resolves 4 weeks after withdrawal of treatment. The rash is seen in 60% to 80% of treated patients.[43]
Acute generalised exanthematous pustulosis (AGEP) has a varied aetiology, although the mechanism of action is still unknown. Drugs (largely anti-bacterials, but also anti-convulsants and anti-inflammatory agents) and viral infections are implicated in the development of AGEP.[45]
Drug rash with eosinophilia and systemic symptoms (DRESS) presents with triad of fever, dermatitis, and internal organ involvement. It presents 3 to 8 weeks after initial exposure to the inciting drug, and may involve human herpesvirus-6 reactivation.[46]
The typical syndrome is diagnosed if the following criteria for DRESS syndrome are met: acute drug-induced generalised eruption, associated systemic involvement (lymph node or visceral), fever and presence of eosinophilia, thrombocytosis, or lymphocyte count above or below normal.[47]
Aromatic anticonvulsants (phenytoin, phenobarbital, carbamazepine) and sulphonamides are the most common cause of DRESS syndrome. Other drugs, including lamotrigine, allopurinol, NSAIDs, captopril, calcium channel blockers, mexiletine, fluoxetine, dapsone, terbinafine, metronidazole, minocycline, and antiretroviral drugs, have also been associated with DRESS sydrome.[46][47]
The pathophysiology of DRESS syndrome is not fully known but may be linked to a genetically determined inability to detoxify reactive drug metabolites.[46]
Full recovery is usual, but symptoms can evolve for weeks, particularly hepatitis, eruption, and eosinophilia.[46]
Corticosteroid-induced rosacea-like eruption, or corticosteroid-induced acne, is characterised by the development of rosacea-like dermatitis of the face (particularly the central facial, peri-oral, and peri-ocular areas) in patients who have been treated for relatively long periods with topical corticosteroids (particularly fluorinated corticosteroids). The average duration of corticosteroid treatment required to produce such adverse effects is 2 months.[48] Corticosteroid acne can also form following systemic corticosteroids.
Idiopathic
Generalised pustular psoriasis (von Zumbusch type):
This is a variant of psoriasis and usually occurs in patients with classic psoriasis with a sudden eruption (within a few hours) of generalised sterile pustules. Impetigo herpetiformis is a rare form of generalised pustular psoriasis during pregnancy. It can recur with subsequent pregnancies.
Patients more often have a family history of psoriasis and/or a history of drug administration.
Its aetiology is unknown, but it is generally perceived to be caused by 1 or 2 triggering factors including infections such as upper respiratory infection, drugs (such as corticosteroid withdrawal, coal tar, iodides, and minocycline), pregnancy, hypocalcaemia, and hypoparathyroidism.[49][50]
An increased incidence of HLA-Cw1 and HLA-DQB1*0303 has been found among patients with pustular psoriasis.[51]
Pyoderma gangrenosum (PG):
Ulcerative disease of the skin that can occur at any age, but most commonly in young-to-middle-aged adults. It affects women more frequently than men. The condition begins with painful pustules and nodules which then ulcerate.
Cause is unknown. In approximately 50% of patients, the disorder is associated with underlying disease, e.g., rheumatoid arthritis, inflammatory bowel disease, haematological and lymphoreticular malignancies, or immunosuppressive conditions.[52]
An atypical form of pyoderma gangrenosum (APG) exists that is more superficial. It is often associated with acute leukaemia and other myeloproliferative diseases. APG lesions may resemble those of Sweet's syndrome, both clinically and histopathologically, but APG will often ulcerate and heal with scarring.[53]
Transient neonatal pustular melanosis:
Benign non-infectious condition seen most commonly in black people; it occurs predominantly on the forehead, back, posterior neck, and shins.[31][33][54]
The fragile sterile vesiculopustules are filled predominantly with neutrophils.
Palmoplantar pustulosis (PPP):
Characterised by sterile pustules localised in the lowest part of stratum corneum, and erythematous scaly skin confined to the palms and soles. It has some common features with other pustular forms of psoriasis and is often classified as a localised form of pustular psoriasis.
Up to 24% of PPP patients have psoriasis, which is much higher than the normal population prevalence of psoriasis.[55]
Onset is usually between 30 and 50 years of age; it is more common in women and is strongly associated with tobacco smoking. The disease is persistent and painful, leading to a considerable functional impairment.[56]
Erosive pustular dermatosis:
Rare cutaneous inflammatory disease with an unknown cause.
Presents with chronic sterile pustules, erosions, and crusted lesions. Typically confined to the scalp that has actinic damage, with resulting scarring alopecia. It may mimic a bacterial infection, which is usually a secondary occurrence.[57]
Use of this content is subject to our disclaimer