Urgent considerations
See Differentials for more details
Generalised pustular psoriasis
Generalised pustular psoriasis (von Zumbusch type) is a variant of psoriasis that can be life-threatening and is characterised by the sudden eruption (occurring within a few hours) of generalised sterile pustules on a red base. Treatment includes acitretin (with or without phototherapy), ciclosporin, or methotrexate, and should be initiated promptly under specialist guidance.[58]
Impetigo herpetiformis is a rare form of generalised pustular psoriasis that occurs during pregnancy.[59] It is associated with increased fetal morbidity and mortality, and there is an increased risk of recurrence with subsequent pregnancies.[59] Treatment is with systemic steroids. The condition resolves after delivery, but recurrence in future pregnancies can occur.[58]
Drug rash with eosinophilia and systemic symptoms
Death rate is about 10%, mostly due to liver damage thought to be mediated by infiltration of eosinophils.[46] Corticosteroids are administered for severe symptoms.[60]
Inflammatory pustular reaction in Behcet's disease
Chronic ophthalmic involvement can result in blindness.[26][54][61][62][63] Specialist-administered treatment includes oral colchicine, oral dapsone, oral thalidomide, methotrexate, prednisone (prednisolone), azathioprine, cyclophosphamide, ciclosporin, and tumour necrosis factor alpha inhibitors.[60][Figure caption and citation for the preceding image starts]: Mouth and genital ulcers in Behcet's diseaseFrom the collection of Dr Yusuf Yazici; used with permission [Citation ends].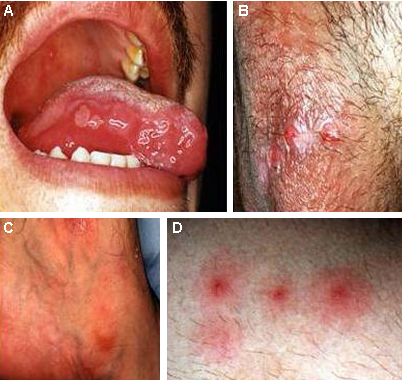
Herpes simplex virus (HSV)
In immunocompromised patients and newborn children there may be disseminated disease with systemic involvement. Most neonatal infections are caused by HSV-1. Viraemia associated with disseminated HSV disease results in the spread of the virus to multiple organs.[64] Treatment is with aciclovir. In aciclovir-resistant HSV, foscarnet is indicated.[60]
Candidal infection and disseminated candidiasis
Invasive fungal dermatitis is a severe, often fatal, form of cutaneous fungal infection that is seen in very-low-birth-weight infants and is characterised by invasion of fungus below the stratum corneum.[65][Figure caption and citation for the preceding image starts]: Infant presenting with rash formerly known as moniliasis, now called candidiasis, caused by Candida sppPublic Health Image Library, CDC [Citation ends].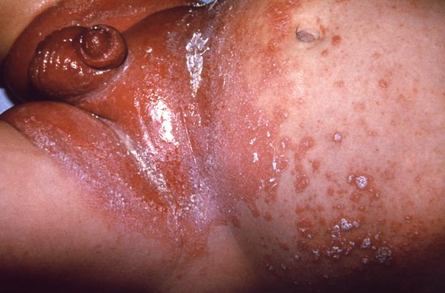 Attributable mortality of as much as 40% for invasive candidiasis.[12]
Attributable mortality of as much as 40% for invasive candidiasis.[12]
Invasive candidiasis is more common in very premature infants, especially those delivered vaginally or receiving long-term glucocorticoid therapy, and is usually seen within the first 2 weeks of life. Other risk factors for invasive candidiasis include the long-term use of broad-spectrum antibiotics, postnatal corticosteroids, parenteral nutrition, intravenous lipids, indwelling catheters, necrotising enterocolitis and abdominal surgery. Recalcitrant or recurrent cutaneous Candida infections may be early indicators of congenital or acquired immunodeficiency.
In invasive fungal infections, early antifungal treatment is critical to reduce morbidity and mortality.[66] Choice of antifungals include amphotericin B, itraconazole, fluconazole, voriconazole, and caspofungin.[60]
Use of this content is subject to our disclaimer