Approach
When a patient presents with sensory changes, pain, and/or weakness in the upper extremity, the first task is to localize the level of the lesion in the nervous system as this narrows down the list of possible causes.[Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on palmFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].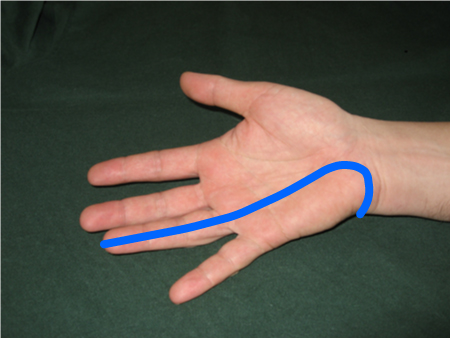 [Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on dorsum of handFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
[Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on dorsum of handFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].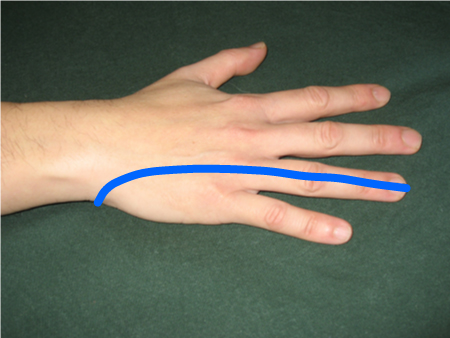 [Figure caption and citation for the preceding image starts]: Approximate distribution of radial sensory nerveFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
[Figure caption and citation for the preceding image starts]: Approximate distribution of radial sensory nerveFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends]. [Figure caption and citation for the preceding image starts]: Approximate distribution of median sensory nerve on palmFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
[Figure caption and citation for the preceding image starts]: Approximate distribution of median sensory nerve on palmFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].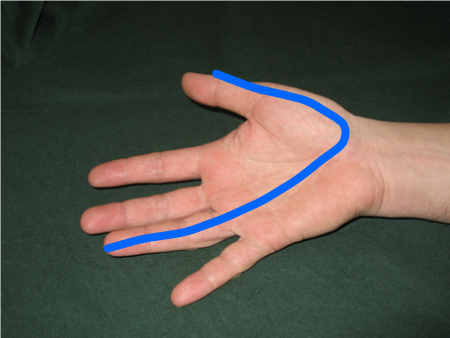
Localization of lesions
Localization usually requires a careful history and physical exam followed by electromyography (EMG) to confirm or refute clinical suspicions. EMG is potentially useful not only in localizing the level of the lesion but also in helping to determine whether the lesion is acute or chronic and whether the etiology is axonal or demyelinating.[2] This is important, as demyelinating lesions tend to have a better chance of complete recovery than do axonal lesions. Also, a different underlying etiology is implied in demyelinating lesions (e.g., multifocal chronic inflammatory demyelinating polyneuropathy) compared with axonal (e.g., peripheral nerve vasculitis).
Once the location of nerve pathology is determined, there is usually only a limited set of possible etiologies that direct further workup and/or management.[Figure caption and citation for the preceding image starts]: Testing thumb abduction strength in assessment of carpal tunnel syndrome: with palm facing up, patient lifts thumb toward ceiling, and resistance is applied as shownFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
Initial tests
Electrodiagnostic testing (nerve conduction studies and EMG)[2]
Can confirm the diagnosis of mononeuropathy
Localizes the site of the entrapment or other pathology
Helps to assess timing of nerve damage (acute, subacute, chronic)
Provides prognostic value in combination with history and clinical examination; more severe axonal loss, neurotmesis, longer duration of symptoms, older patient age, increased patient height, and more proximal lesions are poor prognostic indicators.
Can evaluate more widespread nerve disease.
Laboratory evaluation
Erythrocyte sedimentation rate, C-reactive protein, and complement levels can be checked in patients with signs and symptoms suggestive of peripheral nerve vasculitis.
Imaging studies
MRI or CT is indicated when there is concern about central nervous system disorders (e.g., cervical myelopathy, multiple sclerosis, stroke), spinal nerve root impingement, or brachial plexus lesion. Generally, MRI is more sensitive than CT for these types of lesions.
Rarely patients have ulnar neuropathy at the wrist or palm caused by a ganglion cyst or other structural mass lesion. If EMG localizes the lesion to the distal branches of the ulnar nerve, or if palpation suggests the presence of a ganglion cyst, this can be further evaluated by ultrasound or MRI of the wrist and/or palm.
MRI and/or ultrasound are appropriate investigations for brachial plexus pathology and/or ganglion cysts. Although electrodiagnostic testing remains the gold standard for diagnosis of compression neuropathies, studies have demonstrated that median nerve ultrasound has good sensitivity and specificity in the diagnosis of carpal tunnel syndrome.[4][15]
Further specific tests
Other tests are used for more specific diagnoses, depending on the results of nerve conduction studies and EMG in the context of the history and exam:
CBC with differential for hematocrit in peripheral nerve vasculitis
Antinuclear antibody and anti-DNA antibodies for peripheral nerve vasculitis
Antineutrophil cytoplasmic antibody and rheumatoid factor for peripheral nerve vasculitis
Cryoglobulins for peripheral nerve vasculitis
Hepatitis B and C antibodies for peripheral nerve vasculitis
Nerve and muscle biopsy for peripheral nerve vasculitis or sarcoidosis
Cervical spine x-ray for cervical rib for neurogenic thoracic outlet syndrome
Biopsy of skin lesions or affected nerve for leprosy
HIV/CD4 testing
Polymerase chain reaction cytomegalovirus testing
Lyme serology
Serum and urine protein electrophoresis for amyloidosis
Tissue biopsy of abdominal fat pad, rectal mucosa, or affected nerve for amyloidosis
Lumbar puncture for multifocal chronic inflammatory demyelinating polyneuropathy
Genetic testing for hereditary neuropathy with liability to pressure palsies.
Evidence-based workup
Very few studies exist to guide the practitioner through workup of these symptoms in a systematic and evidence-based manner. Most published recommendations result from expert consensus rather than from the results of published studies. If, based on the history and exam findings, there is a high risk of malignancy, infection, or vasculitis, initial workup should entail urgent imaging studies (malignancy) or appropriate blood tests (infection, vasculitis). Based on the imaging and/or blood test results, biopsy may then be indicated before starting treatment. If these conditions are unlikely, often little workup is necessary, other than EMG to confirm the clinical suspicion of a compressive mononeuropathy.
Musculoskeletal pathologies
Osteoarthritis, tendinitis, or repetitive strain symptoms are often confused with carpal tunnel syndrome and/or ulnar neuropathy, as the distribution of pain can be similar in these entities. Electrophysiologic studies can help identify or exclude an associated mononeuropathy in these cases.
Use of this content is subject to our disclaimer