Approach
Initial assessment of infants with cyanosis should include:[4]
History
Physical exam
Chest x-ray
Complete blood count (CBC) with differential count
Blood glucose
Calcium (hypocalcemia associated with central nervous system irritability/cyanotic heart disease)
Pulse oximetry (preductal [with probe in the right upper extremity] and postductal [with probe in the lower extremity])
Arterial blood gases (ABG) with lactate
Blood culture/sepsis screen
ECG and echocardiogram.
Maternal history
Important features of maternal history, which are associated with neonatal cyanotic disorders, include:
Diabetes mellitus
Transient tachypnea of newborn
Respiratory distress syndrome (RDS)
Hypoglycemia
Large for gestational age
Asthma
Transient tachypnea of newborn
Use of opiates
Respiratory depression from opiates
Pregnancy-induced hypertension
Intrauterine growth retardation
Polycythemia
Hypoglycemia
Polyhydramnios
Tracheoesophageal fistula/esophageal atresia
Congenital diaphragmatic hernia
Delivery of previous sibling with RDS
RDS
Surfactant protein B deficiency or adenosine triphosphate-binding cassette, subfamily A mutations
Group B streptococcal pneumonia
Oligohydramnios
Pulmonary hypoplasia.
Factors relating to labor and delivery
Premature and prolonged rupture of membranes
Sepsis/pneumonia
Pulmonary hypoplasia
Epidural anesthesia
Fever
Anesthesia/analgesia
Respiratory depression
Apnea
Asphyxia
Cerebral edema
Metabolic acidosis
Chorioamnionitis
Sepsis
Pneumonia
Cesarean section without labor
Transient tachypnea of the newborn
RDS
Breech delivery (trauma)
Erb palsy with phrenic nerve palsy.
Physical examination: overview
Cyanosis can develop immediately or several hours after birth.
Immediate:
Transient tachypnea of the newborn
RDS
Pneumothorax or air leak
Meconium aspiration syndrome
Congenital diaphragmatic hernia
Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])
Persistent pulmonary hypertension of the newborn.
Onset hours after birth:
Cyanotic congenital heart disease
Aspiration
Tracheoesophageal fistula
Pneumonia.
General examination
In a cold environment, acrocyanosis is common. Exam should be performed under a radiant warmer in a well-lit room.[12] Prolonged capillary refill time is often evident when peripheral perfusion is suboptimal in:
Hypoplastic left heart syndrome
Sepsis/pneumonia
Polycythemia
Acidosis
Hypovolemic states
Hypothermia.
Respiratory examination
Tachypnea, retractions, nasal flaring, and grunting generally indicate a pulmonary cause. However, these symptoms may also occur in cardiac conditions with significant left-to-right shunt or in sepsis/shock syndromes. The respiratory rate may be normal in infants with cyanotic heart disease or methemoglobinemia. Apnea and cyanosis may be due to sepsis, asphyxia, or seizures.
Upper airway obstruction may be evident from stridulous breathing due to:
Laryngotracheomalacia
Subglottic stenosis
Vocal cord paralysis
Glossoptosis with micrognathia (Pierre-Robin syndrome).
Upper airway obstruction can also give rise to supraclavicular, submandibular, and suprasternal retractions. Bilateral choanal atresia generally gives rise to significant retractions at birth, but the symptoms are relieved by an oral airway. Cyanosis due to parenchymal lung disease is associated with intercostal and subcostal retractions.
Absent/poor aeration of one side of chest on auscultation may be due to:
Pneumothorax
Pleural effusion
Atelectasis
Congenital diaphragmatic hernia.
Cardiovascular examination
Normal heart rate in full-term newborns is approximately 120 beats per minute (bpm), with a range of 100 to 140 bpm. During quiet states it may be as low as 90 bpm. Heart rates >160 bpm during quiet state are abnormal. In supraventricular tachycardia, heart rates >200 bpm are usually seen. Heart rate variability is also important: in severe sepsis and asphyxia, the beat-to-beat variability will be lost. S2 is loud and narrowly split in pulmonary hypertension.
A single S2 is generally indicative of:
Severe pulmonary stenosis
Pulmonary atresia
Abnormal single valve position (transposition of great arteries)
A large semilunar valve, as in truncus arteriosus.
It is important to record the type and quality of murmurs. The location of apical impulse should be noted to rule out dextrocardia. Precordial thrill indicates significant murmur of grade >3/6. Precordial hyperactivity is generally due to increased ventricular activity. It should be remembered that not all heart murmurs are pathologic and that many serious congenital cardiac conditions do not cause murmurs.
Abdominal examination
The abdomen may appear scaphoid in congenital diaphragmatic hernia. Abdominal distention due to bowel obstruction or ascites can give rise to respiratory distress. Hepatosplenomegaly with ascites and hydrops fetalis may occur in cases of severe hemolytic disease of the newborn, a potential cause of severe respiratory distress. Hepatomegaly can coexist with pulmonary congestion in conditions such as total anomalous pulmonary venous return. Absence of bowel sounds indicates ileus and is associated with sepsis, gangrenous bowel, or peritonitis.
Central nervous system examination
Hypotonia is one of the earliest signs of:
Sepsis
Asphyxia
Metabolic disorders.
Phrenic nerve paresis/paralysis can precipitate respiratory distress and is associated with Erb palsy following traumatic vaginal delivery. Excessive traction on the neck or vaginal breech extraction are the common etiologies.
Chest x-ray
Chest x-ray is integral to initial assessment of respiratory distress.[4][20][21] The location of stomach, liver, and heart should be ascertained to rule out dextrocardia and situs inversus.
The size and shape of the heart may yield some clues to the diagnosis:
A small heart may be due to hypovolemia, adrenal insufficiency from asphyxia or adrenal hemorrhage, significant pulmonary interstitial emphysema, and congenital lobar emphysema.
Severe cardiomegaly is present in Ebstein anomaly. Moderate cardiomegaly is seen in infants with diabetic mothers (hyperinsulinemia) and in cardiomyopathy (infections, metabolic disorders, or asphyxia) and congestive cardiac failure. Congestive heart failure without intrinsic cardiac anomaly is seen in coarctation of the aorta and arteriovenous malformation.
The commonly described cardiac silhouettes in congenital heart disease are:
"Egg on end" appearance of transposition of the great vessels
"Snowman" sign (a rounded, figure-of-eight-like cardiac contour) of unobstructed total anomalous pulmonary venous return, surrounded by "snowy" lung fields due to pulmonary congestion
Boot-shaped heart of tetralogy of Fallot.
Pulmonary vascular markings may yield further clues toward the diagnosis:
Increased pulmonary vascular markings and pulmonary congestion are indicative of left-to-right shunt
Decreased pulmonary vascular markings (oligemic lung fields) indicate pulmonary stenosis or pulmonary atresia with inadequate ductal shunting. They may also occur in persistent pulmonary hypertension of the newborn.
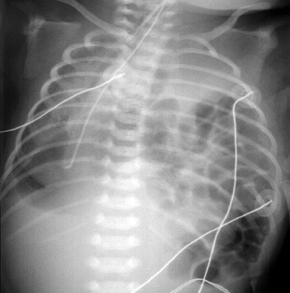
The expansion of lungs (lung volume) on both sides should be checked. Normal inspiratory films should have 8 intercostal spaces of lung fields on both sides. Diaphragmatic paralysis (more commonly seen on the right side) is manifested by elevation of the right hemidiaphragm by more than 2 intercostal spaces compared with the left side. This may simulate right lower lobe atelectasis. Hyperinflated lung fields are seen occasionally in lobar emphysema or cystic lesions of lungs. The prevalence of spontaneous air leaks giving rise to pneumothorax and pneumomediastinum in full-term newborns is approximately 1% to 2%.[Figure caption and citation for the preceding image starts]: Pneumothorax (right side)From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].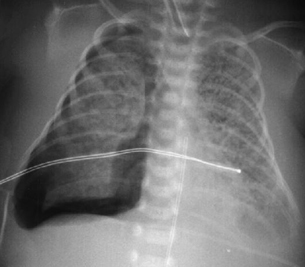 [Figure caption and citation for the preceding image starts]: Pneumomediastinum without pneumothoraxFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
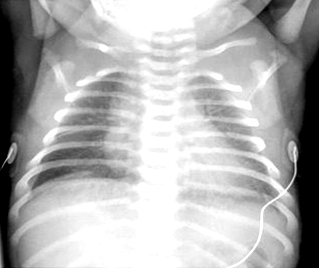
[Figure caption and citation for the preceding image starts]: Pneumomediastinum without pneumothoraxFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Pneumomediastinum with pneumothorax (left side)From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Pneumomediastinum with pneumothorax (left side)From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].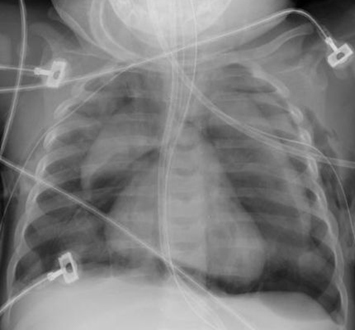
Some characteristic pulmonary findings on chest x-ray are associated with specific pathologies:
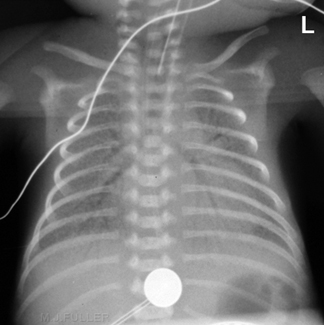
Transient tachypnea of the newborn: lung fields may appear hazy with normal lung volume and increased perihilar markings, frequently with fluid in the horizontal fissure.[Figure caption and citation for the preceding image starts]: Transient tachypnea of the newborn (respiratory distress syndrome type 2): perihilar streakiness and horizontal fissural fluid on the rightFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
RDS: chest x-ray may appear relatively normal in the initial stages. As RDS worsens, the characteristic reticular granular pattern and air bronchograms become evident. Lung volume is reduced significantly in severe RDS.[Figure caption and citation for the preceding image starts]: Hyaline membrane disease (respiratory distress syndrome type 1): air bronchograms and a reticular granular patternFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
Meconium aspiration syndrome: fluffy infiltrates, patchy areas of atelectasis, and areas of hyperinflation due to air trapping may be evident.[Figure caption and citation for the preceding image starts]: Meconium aspiration syndromeFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].

Pleural effusion (due to chylothorax or other causes): visible on lateral aspect of lung fields as a linear opacity. In large effusions, a whole lobe may appear opaque, with mediastinal shift to the contralateral side.[Figure caption and citation for the preceding image starts]: Pleural effusion (right side) with mediastinal shift to the leftFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].

Lobar atelectasis: mediastinal shift toward the ipsilateral side is seen. In pneumonic consolidation, which may simulate atelectasis, no mediastinal shift is present.
Congenital diaphragmatic hernia: soon after birth, a large area of opacity may be the only finding instead of the classical finding of bowel gas in the thorax. This should be differentiated from CPAM (formerly known as CCAM).[Figure caption and citation for the preceding image starts]: Congenital diaphragmatic herniaFrom the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Congenital pulmonary airway malformation (CPAM; formerly known as congenital cystic adenomatoid malformation [CCAM])From the collection of Ponthenkandath Sasidharan, MD; used with permission [Citation ends].
CPAM: may appear as a multicystic air-filled lesion.
It is important to check the bony thoracic cage. In asphyxiating thoracic dystrophy, the thoracic cage will be small and narrow. The thorax may have a bell-shaped appearance in infants with severe hypotonia. Fractures of the ribs, humerus, or clavicles should be looked for following difficult vaginal deliveries, as infants may develop respiratory distress from the pain and splinting of the chest.
Ultrasound
Ultrasound examination of diaphragmatic motion during spontaneous breathing can detect paradoxical motion in diaphragmatic paralysis. Pleural effusion, eventration of the diaphragm (an abnormal elevation of an intact diaphragm), and size/location of the liver/spleen can also be determined.
Other imaging
Computed tomography scan of the chest is occasionally helpful if diagnosis is not clear, and it can identify congenital abnormalities and tumors of the mediastinum, lungs, and heart. Feeding-associated cyanosis may be due to incoordination of sucking and swallowing, gastroesophageal reflux, vocal cord paralysis, laryngeal cleft, severe birth asphyxia, or tracheoesophageal fistula. A pediatric gastroenterologist may recommend a pH probe test or upper gastrointestinal contrast study to rule out severe gastroesophageal reflux.
Pulse oximetry
Pulse oximetry monitoring is recommended for all infants with respiratory distress and cyanosis, because clinician assessment of color at birth varies.[22] It is an accurate, reliable, and noninvasive method for monitoring oxygen saturation in infants.[23][24][25][26] In severe cyanosis with respiratory distress, both preductal and postductal oxygen saturations should be monitored to detect the gradient across the ductus arteriosus. For this procedure, the pulse oximeter probes should be placed over the right hand and a lower extremity (never the left hand). Acrocyanosis is a common finding in young newborns. This generally resolves spontaneously.
Pulse oximetry screening is now accepted practice for early detection of critical congenital heart disease (CCHD) in the newborn, and may detect life-threatening malformations before symptoms develop.[27][28]
[  ]
A significant body of evidence demonstrates the effectiveness of this strategy for reducing morbidity and mortality rates in young children.[28][29] CCHD screening has been widely implemented in the US and Europe, and complements physical exams with relatively few false positive screens.[28][30]
]
A significant body of evidence demonstrates the effectiveness of this strategy for reducing morbidity and mortality rates in young children.[28][29] CCHD screening has been widely implemented in the US and Europe, and complements physical exams with relatively few false positive screens.[28][30]
Laboratory tests
ABG can help in determining the oxygenation, ventilation, and acid-base status of the infant. In methemoglobinemia, the PaO₂ is normal even with cyanosis. Elevated serum lactate is indicative of inadequate oxygen delivery.
CBC with differential count is an important test to rule out polycythemia, anemia, neutropenia, leukopenia, abnormal I:T (immature to total neutrophil count) ratio, and thrombocytopenia as signs of sepsis.
If sepsis is suspected, a blood culture should be obtained immediately and antibiotic therapy started. A spinal tap should be performed in stable infants, but without delaying the start of antibiotic therapy.
Significant metabolic acidosis may indicate cardiac failure, sepsis, asphyxia, or metabolic disorders. Closure of the ductus arteriosus in an infant with a ductal-dependent cardiac lesion can lead to shock and severe metabolic acidosis with cyanosis and respiratory distress.
Accurate blood glucose measurement is essential for diagnosis and management of neonatal hypoglycemia. Local protocols and guidelines on optimal blood sampling and measurement should be followed.[31]
Calcium and magnesium levels should be obtained where other causes have been ruled out. Hypocalcemia and hypomagnesemia are both associated with central nervous system irritability and seizures.
Metabolic screening of urine and drug screening of urine/meconium should be performed as clinically indicated.
ECG
An ECG is an important test, but of limited value except in the diagnosis of arrhythmias.[32][33] Normally, there is right ventricular predominance in the newborn, and many cases of cyanotic congenital heart disease will have similar findings. Left axis deviation with left ventricular dominance is seen in tricuspid atresia or pulmonary atresia with an intact ventricular septum. Left axis deviation is frequently seen in arteriovenous canal malformation due to anatomical defects in the atrioventricular conduction system.
Echocardiogram
Echocardiogram is the definitive test in the diagnosis of congenital cardiac lesions and pulmonary hypertension. A technician who is trained in performing echocardiograms in newborns and a pediatric cardiologist are required for this procedure.
Use of this content is subject to our disclaimer