Approach
The most common presenting condition associated with sporadic vestibular schwannoma is unilateral sensorineural hearing loss. Patients presenting with unilateral sudden or progressive sensorineural hearing loss should undergo diagnostic testing with contrast-enhanced head magnetic resonance imaging (MRI). Although some consider use of auditory brainstem response testing or repeat audiometry for screening, fine-cut contrast-enhanced head MRI is considered the gold standard.[13] Only if MRI is not available or contraindicated (e.g., certain types of pacemakers) should head computed tomography (CT) be considered. Notably, contrast-enhanced head CT cannot reliably detect tumors <1 cm in cerebellopontine angle extension.
Several additional relevant considerations deserve mention. First, there is a somewhat commonly held misconception that patients who experience an episode of sudden sensorineural hearing loss and subsequently improve (either spontaneously or following glucocorticoid administration) do not require an MRI. Importantly, recovery of hearing after sudden sensorineural hearing loss does not exclude the diagnosis of a vestibular schwannoma.[42] Additionally, if no vestibular schwannoma is seen on MRI, the labyrinth should also be scrutinized, as a subset of patients develop small intralabyrinthine schwannomas that are sometimes missed on the official diagnostic read.[43] Lastly, up to 20% of tumors today are found incidentally after imaging is obtained for seemingly unrelated reasons such as headache or other unrelated neurologic or visual symptoms.[19][44]
History
A detailed history pertaining to potential risk factors, the duration and character of relevant symptoms, and potential comorbidities that may impact management decision-making should be obtained.
Risk factors:
Personal or family history of other brain, spinal, or neurogenic tumors such as schwannomas or meningiomas
Family history of neurofibromatosis-related schwannomatosis
History of prior radiation exposure such as head or neck therapeutic radiation for cancer
Most people with sporadic vestibular schwannomas do not have identifiable risk factors.
Relevant symptoms:
Onset, duration, and laterality of hearing loss (e.g., sudden, slowly progressive over years) or tinnitus
Presence and character of dizziness, imbalance, or vertigo
History of facial spasm or facial nerve weakness; specifically asking about prior Bell palsy may be helpful in eliciting relevant history
Presence, distribution, severity, and laterality of facial numbness or facial pain
Presence and character of headaches or vision loss.
Comorbidities:
Conditions associated with increased anesthetic or wound-healing risk should be elicited such as hypertension, diabetes, smoking, malnutrition, or cardiac disease
Medications that increase risk of hemorrhage such as antiplatelet therapy or anticoagulation
Pregnancy, as this impacts tumor management decision-making and may potentially impact natural history of disease.
Physical exam
Although a more extensive physical exam may be performed based on clinical concerns or necessity, depending on tumor size and history, a focused examination relevant to vestibular schwannoma includes:
Eye examination to examine for spontaneous or gaze-induced nystagmus
Examination of facial sensation and distribution of any potential facial hypoesthesia
Presence of facial nerve weakness, spasm, or synkinesis; diminished fast or casual blink is among the most sensitive measures of early facial nerve weakness
Otoscopy to examine for other visible causes of hearing loss
Romberg and tandem gait to assess for cerebellar findings
Fundoscopic examination for papilledema if concern for hydrocephalus exists.
Investigations
Patients with unilateral hearing loss (especially if progressive) not responding to local ear care warrant referral for audiology testing (e.g., behavioral audiogram) and ear, nose, and throat consultation. Patients who exhibit asymmetric sensorineural hearing loss should undergo contrast-enhanced head MRI.[45] Up to 3% of people presenting with these symptoms will have a vestibular schwannoma detected on imaging.[45] MRI is considered the definitive test, as it is more sensitive than CT. Positive findings on MRI include an avidly enhancing lesion located within the internal auditory canal or a lesion in the cerebellopontine angle centered on the opening of the internal auditory canal.
[Figure caption and citation for the preceding image starts]: Contrast-enhanced T1-weighted axial MRI studies demonstrating various sizes of left-sided sporadic vestibular schwannoma. (A) small intracanalicular vestibular schwannoma; (B-C) medium-sized vestibular schwannomas; (D) large cystic vestibular schwannomaFrom the personal collection of Michael J. Link and Matthew L. Carlson, Mayo Clinic, Rochester, MN; used with permission [Citation ends].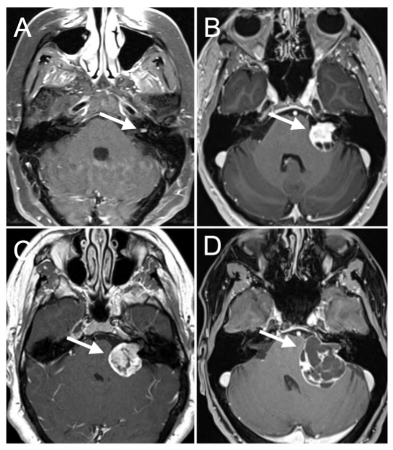 MRI determines the size and location of the tumor, which assists in formulating a management plan. The second most common lesion of the internal auditory canal and cerebellopontine angle is meningioma. Generally, meningiomas are eccentric to the internal auditory canal, display more homogenous contrast enhancement, and have prominent dural enhancement along the petrous dura. Less common lesions in this region include epidermoid tumors, arachnoid cyst, lipoma, other cranial nerve schwannomas, hemangiomas, or metastasis.
MRI determines the size and location of the tumor, which assists in formulating a management plan. The second most common lesion of the internal auditory canal and cerebellopontine angle is meningioma. Generally, meningiomas are eccentric to the internal auditory canal, display more homogenous contrast enhancement, and have prominent dural enhancement along the petrous dura. Less common lesions in this region include epidermoid tumors, arachnoid cyst, lipoma, other cranial nerve schwannomas, hemangiomas, or metastasis.
Patients with neurofibromatosis-related schwannomatosis require more frequent imaging because the tumor growth rate is variable.[45]
The diagnosis of neurofibromatosis-related schwannomatosis can be established based on clinical criteria (e.g., modified Manchester criteria) and genetic testing. Establishing a diagnosis of neurofibromatosis-related schwannomatosis is generally straightforward in people with a known family history through screening tests including audiograms, MRI, and genetic testing. In such cases, people are often diagnosed at a younger age, even before becoming symptomatic. Patients with neurofibromatosis-related schwannomatosis without a family history of disease most commonly present with multiple tumors at diagnosis, although a small subset may initially present at a younger age with a solitary vestibular schwannoma and only later develop additional tumors.
Use of this content is subject to our disclaimer