Tests
1st tests to order
maternal blood type
Test
All Rh-negative pregnant women are at potential risk for alloimmunization and erythroblastosis.
Result
Rh-negative
maternal serum Rh antibody screen
Test
Positive red blood cell antibody screen must prompt further investigation for possible alloimmunization due to Rh antibodies.[14]
Result
positive screen
Tests to consider
maternal serum antibody titer
Test
As methods vary between laboratories performing this test, each should report the titer below which severe fetal Rh incompatibility is unlikely and above which further investigations and monitoring are indicated.[36]
The maternal serum antibody titer is a guide to disease severity. The American College of Obstetricians and Gynecologists states that a critical titer (titer associated with a significant risk for severe hemolytic disease of the fetus and newborn, and hydrops) is considered to be between 1:8 and 1:32 in most centers.[32] If the initial antibody titer is 1:8 or less, the patient may be monitored with titer assessment every 4 weeks.[32] However, serial titers are not adequate for monitoring fetal status when the mother has had a previously affected fetus or neonate.[32]
Result
critical titer: between 1:8 and 1:32 (may vary among laboratories)
paternal blood type
Test
An Rh-positive partner of an Rh-negative mother creates blood group incompatibility in the fetus.
Result
Rh-positive
paternal zygosity
Test
Heterozygosity denotes a 50% risk of the offspring having an Rh-negative blood type and no risk of Rh incompatibility. Homozygosity denotes a 100% chance of an Rh-positive fetus, at risk of Rh incompatibility. Zygosity is determined by assay of plasma DNA in the case of RhD; serologic testing of paternal red cells can be used for analysis of other red cell antigen systems.
Result
homozygous or heterozygous
fetal ultrasound
Test
Fluid in serous cavities of the fetus is easily detected with ultrasonography.[30][35][37][38]
These findings are consistent with severe fetal anemia in an affected fetus.[37][Figure caption and citation for the preceding image starts]: Fetal hydrops, with ascites and hepatomegaly (arrow) diagnosed on prenatal ultrasoundThe Ottawa Hospital; used with consent of the patient [Citation ends].
Result
may show subcutaneous edema, ascites, pleural effusion, or pericardial effusion
Doppler velocimetry of fetal middle cerebral artery (peak systolic velocity)
Test
Measured Doppler sonography with estimation of peak systolic velocity in the fetal middle cerebral artery (MCA) can be used to predict moderate to severe anemia in the fetus. MCA peak systolic velocity is increased in fetuses with significant anemia. Elevated blood flow velocity for gestational age should prompt percutaneous umbilical blood sampling (if anemia is strongly suspected).[35][Figure caption and citation for the preceding image starts]: Increased velocity in the middle cerebral artery consistent with severe fetal anemiaThe Ottawa Hospital; used with consent of the patient [Citation ends].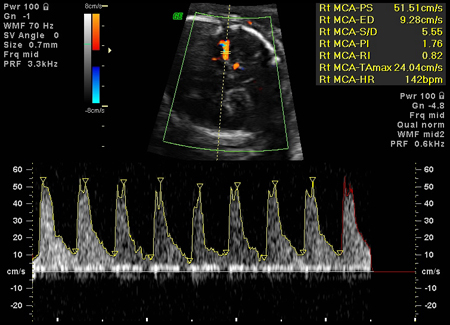
Result
≥1.5 MoM
fetal blood typing (from amniocentesis or maternal circulation)
Test
If the father is heterozygous RhD-positive, or paternity is uncertain, the fetus' RhD type is determined by genetic testing of amniotic fluid cells or it can be estimated using cell-free fetal DNA in the maternal circulation.[33]
Result
Rh type
direct assessment of fetal anemia
Test
Through umbilical cord venipuncture (cordocentesis) or the intrahepatic vein.
If fetal hemoglobin is within 2 g/dL (2 standard deviations) of gestational age norms and direct antiglobulin test is positive, the fetus is only mildly affected. Hemoglobin deficit of 2 to 7 g/dL suggests moderate anemia. Fetal anemia is severe with hemoglobin deficits >7 g/dL.
Result
fetal hemoglobin and hematocrit
rosette test
Test
A rosette test can be used to rule out significant fetomaternal hemorrhage.
Result
may be positive
Kleihauer-Betke test/flow cytometry
Test
Can measure the amount of fetal blood in the maternal circulation.
Result
variable
Use of this content is subject to our disclaimer