Joint dislocation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
shoulder dislocation
reduction and immobilization ± surgical referral
Once the diagnosis has been confirmed, reduction should be attempted. For a successful outcome, adequate analgesia and sedation are necessary before the reduction procedure is attempted. There are numerous reduction maneuvers for shoulder injuries, which are usually performed under local anesthesia (i.e., intra-articular lidocaine) combined with procedural sedation (e.g., intravenous morphine, midazolam, or etomidate).
[  ]
Is there randomized controlled trial evidence to support the use of intra-articular lidocaine instead of intravenous analgesia for manual reduction of acute anterior shoulder dislocation?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.384/fullShow me the answer
]
Is there randomized controlled trial evidence to support the use of intra-articular lidocaine instead of intravenous analgesia for manual reduction of acute anterior shoulder dislocation?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.384/fullShow me the answer
The choice for sedation depends on the treating physician and must be accompanied by continuous monitoring of the patient with capnography and pulse oximetry, as well as frequent blood pressure measurements.
Local anesthesia on its own should be reserved for patients with contraindications to procedural sedation.
Each of the reduction methods works by abduction and external rotation to disengage the humeral head from the glenoid, with axial traction to reduce it. Irrespective of the technique used, the physician should feel a distinct clunk as the shoulder reduces.
The arm should be immobilized and placed in a sling or a sling and swathe.
An anteroposterior (AP) and lateral radiograph should be obtained to confirm reduction of the humeral head, and to ensure that no iatrogenic fractures have occurred during the reduction.[74]Rozzi SL, Anderson JM, Doberstein ST, et al. National Athletic Trainers' Association position statement: immediate management of appendicular joint dislocations. J Athl Train. 2018 Dec;53(12):1117-28.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6365071
http://www.ncbi.nlm.nih.gov/pubmed/30609383?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Normal axillary x-ray view of a reduced shoulder dislocation, showing congruency of the glenohumeral jointPersonal collection of Dr Paul Novakovich [Citation ends].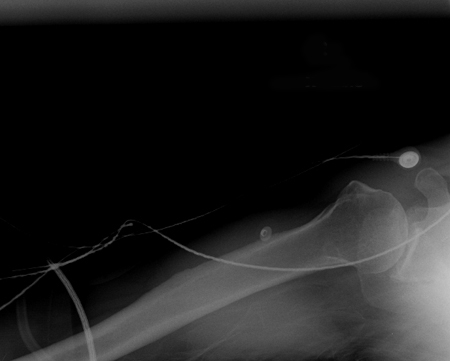
Once the patient is alert, it is important to perform a neurologic and vascular exam.
The patient should wear the sling for approximately 3 weeks.
Patients under 25 years of age should be referred to an orthopedic surgeon for consideration of further intervention (i.e., possible arthroscopic or open repair), as this age group is at significant risk for recurrence. Long-term data support primary stabilization via anatomic Bankart repair (over simple arthroscopic lavage or nonoperative treatment) for young, high-risk patients with a first-time shoulder dislocation.[75]Yapp LZ, Nicholson JA, Robinson CM. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: long-term follow-up of a randomized, double-blinded trial. J Bone Joint Surg Am. 2020 Mar 18;102(6):460-7. http://www.ncbi.nlm.nih.gov/pubmed/31895236?tool=bestpractice.com [76]Adam M, Attia AK, Alhammoud A, et al. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: systematic review and meta-analysis. Int Orthop. 2018 Oct;42(10):2413-22. http://www.ncbi.nlm.nih.gov/pubmed/29982868?tool=bestpractice.com One systematic review found that patients, particularly active men in their 20s and 30s, undergoing treatment for a first-time anterior shoulder dislocation with a surgical stabilization procedure, can be expected to experience significantly lower rates of recurrent instability and a significantly decreased need for a future stabilization procedure when compared with patients treated nonoperatively.[77]Belk JW, Wharton BR, Houck DA, et al. Shoulder stabilization versus immobilization for first-time anterior shoulder dislocation: a systematic review and meta-analysis of level 1 randomized controlled trials. Am J Sports Med. 2023 May;51(6):1634-43. http://www.ncbi.nlm.nih.gov/pubmed/35148222?tool=bestpractice.com
The Latarjet procedure is a commonly used approach for managing chronic and recurrent anterior shoulder dislocation, especially in the presence of bone loss.[78]Alkhelaifi K, Alzobi OZ, Mahmoud SA, et al. Recurrent instability after the Latarjet procedure. J Am Acad Orthop Surg Glob Res Rev. 2023 Nov 27;7(12):e23.00205. https://journals.lww.com/jaaosglobal/fulltext/2023/12000/recurrent_instability_after_the_latarjet_procedure.1.aspx http://www.ncbi.nlm.nih.gov/pubmed/38011051?tool=bestpractice.com It involves transplant of the coracoid process to the scapular neck and has demonstrated excellent long-term clinical outcomes and return to sport rate.[79]Hasebroock AW, Brinkman J, Foster L, et al. Management of primary anterior shoulder dislocations: a narrative review. Sports Med Open. 2019 Jul 11;5(1):31. https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-019-0203-2 http://www.ncbi.nlm.nih.gov/pubmed/31297678?tool=bestpractice.com It may be more effective than Bankart repair for recurrent instability of the shoulder.[80]An VV, Sivakumar BS, Phan K, et al. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016 May;25(5):853-63. http://www.ncbi.nlm.nih.gov/pubmed/26809355?tool=bestpractice.com Both open and arthroscopic Latarjet procedures result in significantly improved function and outcome in patients with anterior shoulder instability.[81]Hurley ET, Lim Fat D, Farrington SK, et al. Open versus arthroscopic Latarjet procedure for anterior shoulder instability: a systematic review and meta-analysis. Am J Sports Med. 2019 Apr;47(5):1248-53. http://www.ncbi.nlm.nih.gov/pubmed/29558168?tool=bestpractice.com However, the Latarjet procedure has been associated with a complication rate of 15% to 30%; specific complications include graft-related issues (11.7%), hardware-related complications (6.5%), nerve injuries (0.7% to 4%), recurrent instability (8%), and revision (5%).[78]Alkhelaifi K, Alzobi OZ, Mahmoud SA, et al. Recurrent instability after the Latarjet procedure. J Am Acad Orthop Surg Glob Res Rev. 2023 Nov 27;7(12):e23.00205. https://journals.lww.com/jaaosglobal/fulltext/2023/12000/recurrent_instability_after_the_latarjet_procedure.1.aspx http://www.ncbi.nlm.nih.gov/pubmed/38011051?tool=bestpractice.com
rehabilitation
Treatment recommended for ALL patients in selected patient group
In subsequent weeks, active-assisted range of motion and isometric strengthening exercises should be advised.
finger dislocation
reduction and immobilization
Reduction of finger dislocation often requires the use of a local anesthetic, typically lidocaine 1%. A neurovascular exam of the digit is essential before reduction is performed because the local anesthetic may cause complete hypoesthesia of the finger.
The first step in reduction is to recreate the injury by hyperextending the proximal interphalangeal (PIP) or distal interphalangeal joint.
This should be followed by light axial traction applied to the finger with pressure applied to the base of the dislocated digit until the joint is relocated.
If the joint is stable, buddy taping to an adjacent digit or placement of a splint in slight flexion is an appropriate measure.
Neutral splinting for dorsal PIP dislocation can also be used and is reported to avoid postsplinting flexion contractures.[82]Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: High prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007 Oct;26(4):983-91. http://www.ncbi.nlm.nih.gov/pubmed/17896393?tool=bestpractice.com
Postreduction x-ray films should be obtained to confirm congruency of the joint and to ensure there are no associated fractures.[15]Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004 Jul-Aug;32(5):1114-21. http://www.ncbi.nlm.nih.gov/pubmed/15262631?tool=bestpractice.com
Following reduction, the physician should ensure adequate perfusion to the finger by assessing capillary refill.
If attempts at reduction fail, consult a specialist hand surgeon.
rehabilitation
Treatment recommended for ALL patients in selected patient group
Postreduction, patients should begin protected range of motion as pain permits. In treating finger dislocations, instituting early motion and providing stability must be balanced.
reduction and immobilization
These are more likely to be unstable.
Reduction of finger dislocation often requires the use of a local anesthetic, typically lidocaine 1%. A neurovascular exam of the digit is essential before reduction is performed because the local anesthetic may cause complete hypoesthesia of the finger.
The finger should be flexed with mild axial traction applied to the digit.
The physician should then apply pressure to the base of the digit until reduction is complete.
Postreduction x-ray films should be obtained to confirm congruence of the joint and to ensure there are no associated fractures.
The finger should be placed in an extension splint immobilizing the smallest number of joints possible.
Following reduction, the physician should ensure adequate perfusion to the finger by assessing capillary refill.
rehabilitation
Treatment recommended for ALL patients in selected patient group
Postreduction, patients should begin protected range of motion as pain permits. In treating finger dislocations, instituting early motion and providing stability must be balanced.
reduction and immobilization
Reduction of finger dislocation often requires the use of a local anesthetic, typically lidocaine 1%. A neurovascular exam of the digit is essential before reduction is performed because the local anesthetic may cause complete hypoesthesia of the finger.
With simple dislocations, the finger is usually held in extension, and there is some contact between the joint surfaces.
The patient's wrist should be flexed to relax the flexor tendons, and the affected digit should then be hyperextended.
The physician should then apply a volar-directed pressure to the dorsum of the affected digit.
It is paramount that excessive traction not be applied, as a simple dislocation can be converted into a complex metacarpophalangeal dislocation with significant soft tissue entrapment.
Simple dislocations can be buddy taped, while fracture dislocations require immobilization in a splint
Postreduction x-ray films should be obtained to confirm congruence of the joint and to ensure there are no associated fractures.
Following reduction, the physician should ensure adequate perfusion to the finger by assessing capillary refill.
If attempts at reduction fail, consult a specialist hand surgeon.
rehabilitation
Treatment recommended for ALL patients in selected patient group
Postreduction, patients should begin protected range of motion as pain permits. In treating finger dislocations, instituting early motion and providing stability must be balanced.
patellar dislocation
reduction and immobilization
Patellar dislocation often presents to the emergency room or to the clinic having already spontaneously reduced.
In a patient presenting with an acute patellar dislocation, a reduction should be performed with the goal being the concentric reduction of the patella into the femoral notch. In cases of intra-articular lesions, orthopedic consultation is warranted, as open reduction surgery may be required.
Lateral dislocation is easily managed using local anesthesia (i.e., intra-articular lidocaine) combined with procedural sedation (e.g., intravenous morphine, midazolam, or etomidate). The choice for sedation depends on the treating physician and must be accompanied by continuous monitoring of the patient with capnography and pulse oximetry, as well as frequent blood pressure measurements.
Local anesthesia on its own should be reserved for patients with contraindications to procedural sedation.
Following adequate analgesia, the patient should be placed either supine or in a seated position.
The affected knee should be flexed to decrease the tension on the quadriceps muscle.
The physician should apply a medial-directed force to the lateral aspect of the patella while slowly extending the leg.
A palpable clunk should confirm reduction of the patella.
Upon successful reduction, the affected extremity should be placed in a knee immobilizer and patient advised to bear weight on the joint as tolerated.
Merchant, anteroposterior (AP), and lateral knee plain x-ray films should be ordered to ensure that the patella is reduced. The x-rays should be closely examined for evidence of any osteochondral defects that may have been created during the reduction.
A Cochrane review concluded that large multicenter clinical trials are needed to determine whether a surgical or nonoperative approach is preferred for the management of patellar dislocations.[84]Smith TO, Gaukroger A, Metcalfe A, et al. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2023 Jan 24;(1):CD008106. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008106.pub4/full http://www.ncbi.nlm.nih.gov/pubmed/36692346?tool=bestpractice.com A systematic review of overlapping meta-analyses found that operative treatment of first-time patellar dislocations results in a lower recurrence rate but no improvement in functional outcome scores compared with nonoperative management.[85]Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy. 2015 Jun;31(6):1207-15. http://www.ncbi.nlm.nih.gov/pubmed/25636989?tool=bestpractice.com
Medial patellofemoral ligament reconstruction for patellofemoral instability was associated with a high rate of success in one systematic review.[86]Shah JN, Howard JS, Flanigan DC, et al. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012 Aug;40(8):1916-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3615712 http://www.ncbi.nlm.nih.gov/pubmed/22679297?tool=bestpractice.com Complications were, however, common (complication rate 26.1%).
rehabilitation
Treatment recommended for ALL patients in selected patient group
In subsequent weeks, active-assisted range of motion exercises and isometric strengthening exercises should be advised.
elbow dislocation
reduction and immobilization
Reduction is usually performed using local anesthesia (i.e., intra-articular lidocaine) combined with procedural sedation (e.g., intravenous morphine, midazolam, or etomidate). The choice for sedation depends on the treating physician and must be accompanied by continuous monitoring of the patient with capnography and pulse oximetry, as well as frequent blood pressure measurements.
Local anesthesia on its own should be reserved for patients with contraindications to procedural sedation.
The patient should be supine on the bed with the physician positioned on the affected side with an assistant close to the head of the bed. In young children, management of radial head subluxation/dislocation (nursemaid elbow) may be more effective and less painful when performed with the arm in pronation as opposed to supination.[87]Krul M, van der Wouden JC, van Suijlekom-Smit LW, et al. Manipulative interventions for reducing pulled elbow in young children. Cochrane Database Syst Rev. 2017 Jul 28;(7):CD007759.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007759.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/28753234?tool=bestpractice.com
[  ]
How does hyperpronation compare with supination plus flexion for reducing pulled elbow in young children?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1848/fullShow me the answer
]
How does hyperpronation compare with supination plus flexion for reducing pulled elbow in young children?/cca.html?targetUrl=https://cochranelibrary.com/cca/doi/10.1002/cca.1848/fullShow me the answer
The arm should be initially extended to 30° flexion.
The overall gross alignment of the elbow is then manipulated so that the olecranon appears centered between the medial and lateral condyle of the humerus.
The forearm is then slowly flexed to approximately 90° with the physician providing longitudinal traction to the forearm while the assistant provides countertraction to the patient's humerus.
The arm is then flexed even further with direct downward pressure applied to the olecranon.[44]Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients 40 years of age and younger: a prospective 25-year follow-up. J Bone Joint Surg Am. 2008 May;90(5):945-52. http://www.ncbi.nlm.nih.gov/pubmed/18451384?tool=bestpractice.com
If reduction is successful, the physician should feel an audible clunk as the elbow is reduced.
It is important not to flex the arm forcefully if there is significant resistance because the coronoid process is typically perched on the distal humerus. Forceful flexion without adequate traction can cause a fracture of this structure, which will result in future instability.
Upon reduction, the arm is placed in a posterior splint at 90° flexion with neutral rotation of the forearm.[44]Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients 40 years of age and younger: a prospective 25-year follow-up. J Bone Joint Surg Am. 2008 May;90(5):945-52. http://www.ncbi.nlm.nih.gov/pubmed/18451384?tool=bestpractice.com
An anteroposterior (AP) and lateral plain film radiograph of the elbow should be obtained to ensure that the joint is concentrically reduced. [Figure caption and citation for the preceding image starts]: Anteroposterior x-ray view of a reduced elbow dislocationPersonal collection of Dr Paul Novakovich [Citation ends].
Once the patient is alert, it is important to perform a neurologic and vascular exam.
rehabilitation
Treatment recommended for ALL patients in selected patient group
Several studies have shown better outcomes with early range of motion than with immobilization in patients with simple dislocations.
Patients should initially be splinted in a posterior splint for comfort with instructions to begin range of motion when pain allows.
Immobilization should last no longer than 2 weeks.[33]Kälicke T, Muhr G, Frangen TM. Dislocation of the elbow with fractures of the coronoid process and radial head. Arch Orthop Trauma Surg. 2007 Dec;127(10):925-31. http://www.ncbi.nlm.nih.gov/pubmed/17713772?tool=bestpractice.com [88]Cohen MS, Hastings H 2nd. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998 Jan-Feb;6(1):15-23. http://www.ncbi.nlm.nih.gov/pubmed/9692937?tool=bestpractice.com [89]Ross G, McDevitt ER, Chronister R, et al. Treatment of simple elbow dislocation using an immediate motion protocol. Am J Sports Med. 1999 May-Jun;27(3):308-11. http://www.ncbi.nlm.nih.gov/pubmed/10352765?tool=bestpractice.com [90]Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002 Jul;21(3):499-519. http://www.ncbi.nlm.nih.gov/pubmed/12365240?tool=bestpractice.com [91]Sillanpää P, Mattila VM, Iivonen T, et al. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008 Apr;40(4):606-11. http://www.ncbi.nlm.nih.gov/pubmed/18317388?tool=bestpractice.com
hip dislocation
reduction and bracing
Every effort should be made to obtain reduction of the dislocated hip within 6 hours from injury, via closed or open reduction techniques to maximize functional recovery.[4]Sanders S, Tejwani N, Egol KA. Traumatic hip dislocation - a review. Bull NYU Hosp Jt Dis. 2010;68(2):91-6. http://hjdbulletin.org/files/archive/pdfs/281.pdf http://www.ncbi.nlm.nih.gov/pubmed/20632983?tool=bestpractice.com Urgent reduction of the femoral head into the acetabulum is indicated in almost all cases.
Unless an associated hip or femoral neck fracture is known to exist, a closed reduction under sedation or anesthesia can be attempted in the emergency department.[92]Stewart MJ, Milford LW. Fracture-dislocation of the hip; an end-result study. J Bone Joint Surg Am. 1954 Apr;36(A:2):315-42. http://www.ncbi.nlm.nih.gov/pubmed/13152141?tool=bestpractice.com
Allis method: traction is applied in line with the deformity. The patient is placed supine, with the surgeon standing above the patient on the stretcher. Initially, the surgeon applies inline traction, while the assistant applies countertraction, stabilizing the pelvis. While increasing the traction force, the surgeon slowly increases the degree of flexion to approximately 70°. Gentle rotational motions of the hip and slight adduction will often help the femoral head clear the lip of the acetabulum. A lateral force to the proximal thigh may assist in reduction. An audible "clunk" is a sign of a successful closed reduction.[93]DeLee JC. Fractures and dislocations of the hip. In: Rockwood CA Jr, Green DP, Bucholz R, eds. Fractures in adults. Vol 2. 4th ed. Philadelphia, PA: Lippincott-Raven; 1996:1756-1803.
Stimson gravity technique: the patient is placed prone on the stretcher, with the affected leg hanging off the side of the stretcher. This brings the extremity into a position of 90° of both hip and knee flexion. In this position, the assistant immobilizes the pelvis and the surgeon applies an anteriorly directed force on the proximal calf. Gentle rotation of the limb may assist in reduction.[93]DeLee JC. Fractures and dislocations of the hip. In: Rockwood CA Jr, Green DP, Bucholz R, eds. Fractures in adults. Vol 2. 4th ed. Philadelphia, PA: Lippincott-Raven; 1996:1756-1803.
rehabilitation
Treatment recommended for ALL patients in selected patient group
Hip immobilization is difficult. Patients usually do well with assisted ambulation using crutches, and bear weight as tolerated. Crutches should be used until the patient can walk relatively pain free, and the knee immobilizer should be kept in place until strength improves and symptoms abate. Moderate quadriceps strengthening should begin when the patient is comfortable.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer