Aetiology
The solitary pulmonary nodule is a relatively round lesion that is <3 cm in diameter and completely surrounded by lung parenchyma. Based on this definition, an estimated 70% to 97% of solitary pulmonary nodules encountered will be benign.[4][5] The clinician determines the probability of malignancy in the individual by evaluating the clinical characteristics of the patient, along with the radiographic features of the nodule. The aim is to diagnose malignancy quickly while avoiding invasive procedures in the evaluation of benign nodules.[6] The likelihood of the potential aetiologies of solitary pulmonary nodules varies with the characteristics of the patient involved.
Benign causes of a solitary pulmonary nodule include:
Granulomatous infections (e.g., mycobacteria)
Other infections (e.g., fungi, septic emboli)
Non-infectious granulomatous conditions (e.g., sarcoidosis, lymphoid granulomatosis)
Inflammatory diseases
Vasculitides
Benign tumours (e.g., hamartoma, lipoma)
Pulmonary amyloidosis
Mucoid impaction
Arteriovenous malformations
Bronchogenic cysts
Bronchoceles
Intrapulmonary lymph nodes
Malignant causes of a solitary pulmonary nodule include:
Primary lung tumours
Metastasis from extra-thoracic cancers
Lymphoma
Sarcoma
Carcinoid
The most likely cause of benign solitary pulmonary nodules will depend on the local epidemiology of disease. For example, at a US academic centre, 23% of patients undergoing resection of a suspicious nodule had benign pathology, with granulomatous disease, such as tuberculosis and fungal infections (e.g., histoplasmosis, coccidioidomycosis, aspergillosis), identified as the most common cause.[7] Non-infectious granulomas are usually due to granulomatosis with polyangiitis (formerly known as Wegener's granulomatosis), sarcoidosis, or rheumatoid arthritis.[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a right upper lobe posterior cavitating nodule, with biopsy confirming granulomatosis with polyangiitisFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a right upper lobe apical solid nodule with a surrounding ‘ground glass’ halo, in a patient with seropositive rheumatoid arthritis on methotrexate. Other similar nodules were seen throughout both lungs, and remain stable for >2 years, consistent with inflammatory benign rheumatoid nodulesFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a right upper lobe apical solid nodule with a surrounding ‘ground glass’ halo, in a patient with seropositive rheumatoid arthritis on methotrexate. Other similar nodules were seen throughout both lungs, and remain stable for >2 years, consistent with inflammatory benign rheumatoid nodulesFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].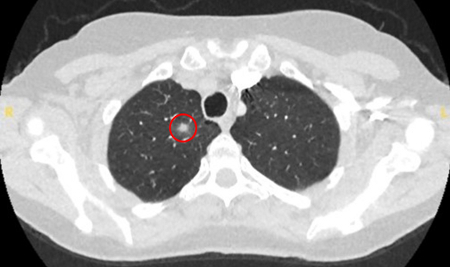
Adenocarcinoma and squamous cell carcinomas are responsible for most malignant solitary pulmonary nodules. Bronchoalveolar cell carcinoma, carcinoid tumours, lymphomas, sarcomas, and metastases from other solid organ malignancies should also be considered.[8]
The remaining causes are infrequent and include mucoid impaction, septic emboli, arteriovenous malformations, and pulmonary amyloidosis.
[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing two areas (red circles) of mucoid impaction of the left upper lobe subsegmental bronchi, resulting in appearance that mimics a noduleFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].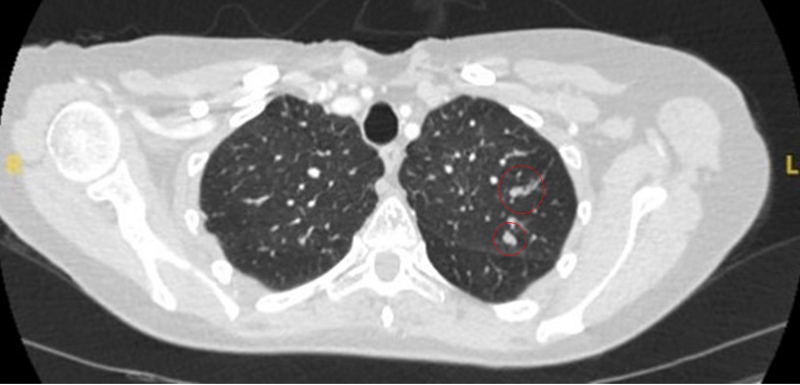 [Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing two left lower lobe peripheral nodules (one slightly spiculated and the other with smoother margins) in a patient presenting with fever, high inflammatory serum markers, and blood cultures confirming Streptococcus intermedius. Both nodules completely resolved following a course of linezolid, consistent with septic emboliFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing two left lower lobe peripheral nodules (one slightly spiculated and the other with smoother margins) in a patient presenting with fever, high inflammatory serum markers, and blood cultures confirming Streptococcus intermedius. Both nodules completely resolved following a course of linezolid, consistent with septic emboliFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a left upper lobe peripheral elongated nodule, with contrast enhancement and a clear feeding and draining side, consistent with a small arteriovenous malformationFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a left upper lobe peripheral elongated nodule, with contrast enhancement and a clear feeding and draining side, consistent with a small arteriovenous malformationFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].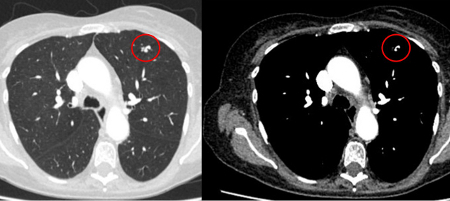 [Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a right lower lobe large nodule, with contrast enhancement and a clear feeding and draining side, consistent with an arteriovenous malformationFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography (CT) showing a right lower lobe large nodule, with contrast enhancement and a clear feeding and draining side, consistent with an arteriovenous malformationFrom the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission [Citation ends].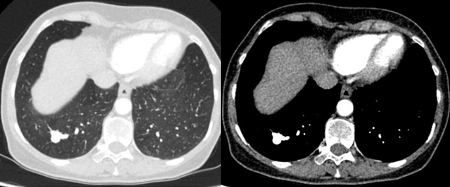
Use of this content is subject to our disclaimer