Images and videos
Images
Assessment of solitary pulmonary nodule
Computed tomography (CT) section capturing the transthoracic core biopsy needle targeting a left lower lobe lobulated nodule. Histopathology confirmed a well-differentiated squamous cell lung cancer
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
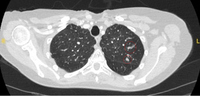
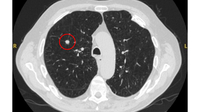
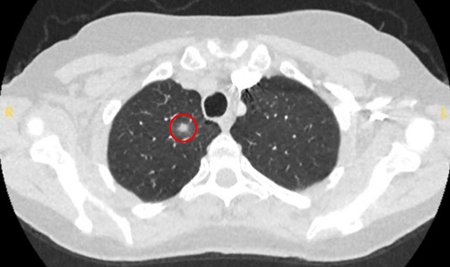
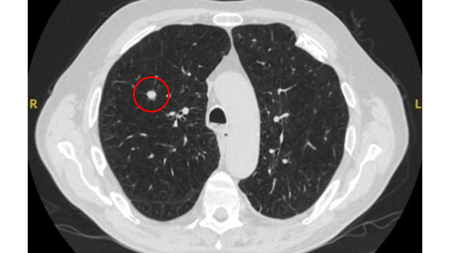
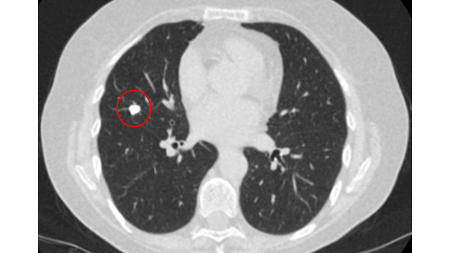
Computed tomography (CT) showing a right upper lobe apical solid nodule with a surrounding ‘ground glass’ halo, in a patient with seropositive rheumatoid arthritis on methotrexate. Other similar nodules were seen throughout both lungs, and remain stable for >2 years, consistent with inflammatory benign rheumatoid nodules
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
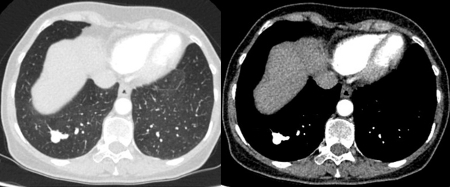
Computed tomography (CT) showing a right lower lobe large nodule, with contrast enhancement and a clear feeding and draining side, consistent with an arteriovenous malformation
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:

Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a left upper lobe ground-glass nodule. This was eventually resected 2 years into surveillance because of growth and the histopathology confirmed adenocarcinoma of lung with mixed mucinous-lepidic pattern
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
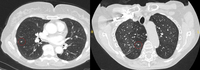
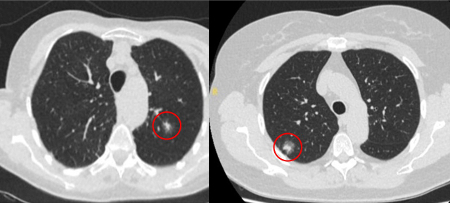
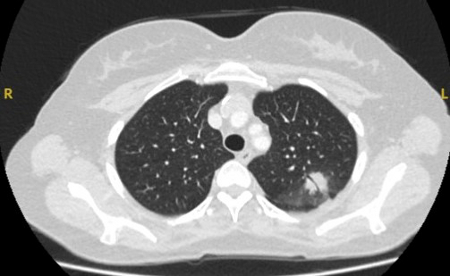
Computed tomography (CT) sections from two cases with benign perifissural nodules. Note the smooth margins and the normal undisturbed adjacent fissure
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a left upper lobe peripheral nodule with several pleural ‘tags’ and element of retraction of the adjacent pleura. Resection histopathology confirmed a well-differentiated squamous cell lung cancer
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Initial approach to solid pulmonary nodules
Callister MEJ et al. Thorax 2015;70:ii1-ii54; used with permission
See this image in context in the following section/s:

Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a right upper lobe posterior cavitating nodule, with biopsy confirming granulomatosis with polyangiitis
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Solid pulmonary nodule surveillance algorithm. VDT, volume doubling time
Callister MEJ et al. Thorax 2015;70:ii1-ii54; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
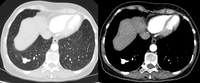
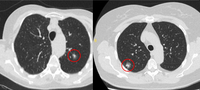
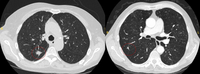
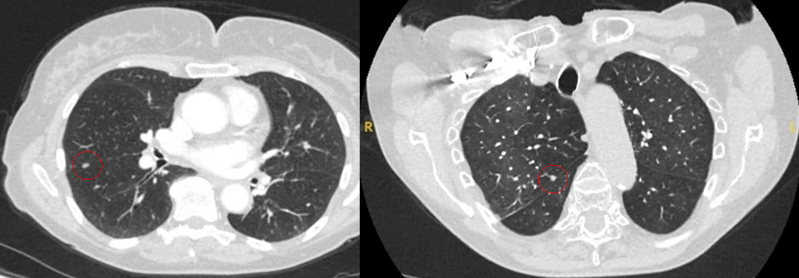
Computed tomography (CT) showing examples of malignant perifissural nodules. Note the spiculated edge of the nodules and the evident retraction of the adjacent fissure. Both resection tissue analyses confirmed adenocarcinoma of lung
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:

Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a small peripheral triangular nodule in the right lower lobe, consistent with an intrapulmonary lymph node
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
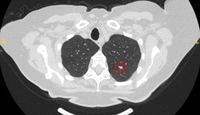
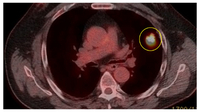
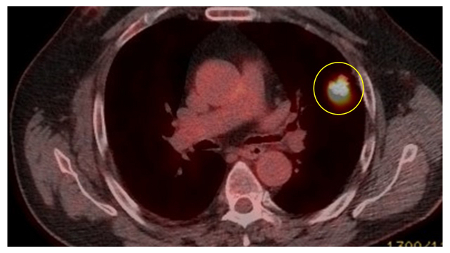
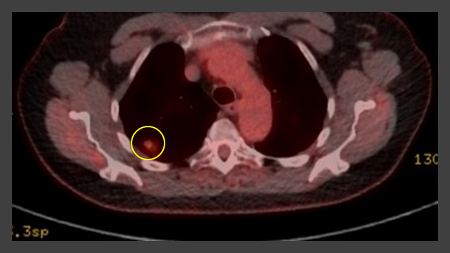
PET CT scan with 18-fluorodeoxyglucose (18-FDG) showing a high uptake peripheral left lung lesion. Surgical resection confirmed a moderately differentiated squamous cell lung cancer
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:

Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a small left upper lobe nodule with smooth margins, subsequently found to be a solitary colorectal metastasis on resection
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
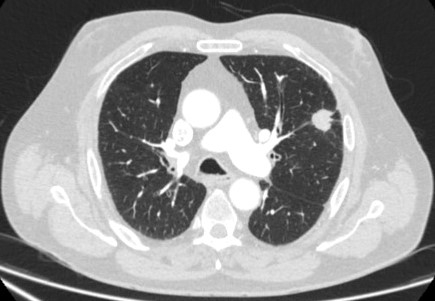
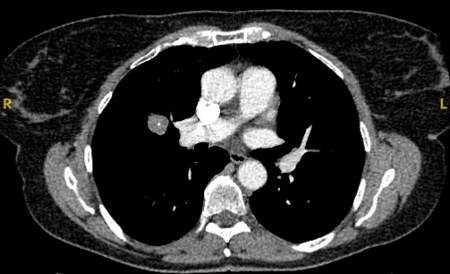
Computed tomography (CT) showing a right upper lobe spiculated solitary nodule within emphysema, in a current smoker with previous asbestos exposure. Note the visible pleural plaque on the left side. Resection histology revealed adenocarcinoma of the lung
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
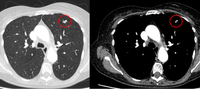
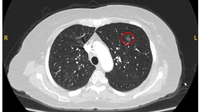
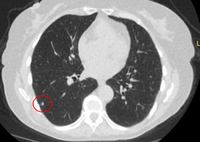
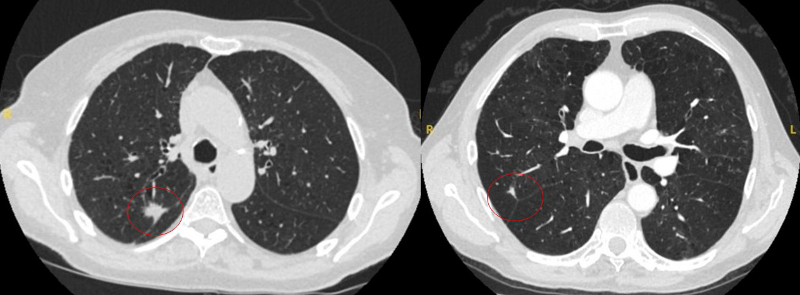
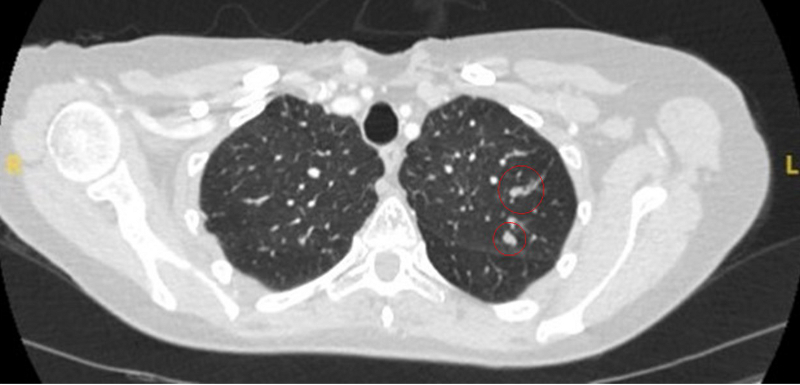
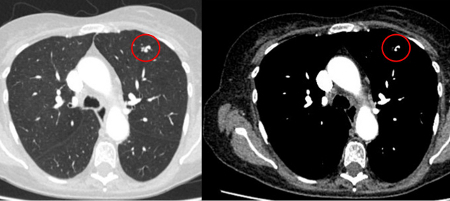
Computed tomography (CT) showing two areas (red circles) of mucoid impaction of the left upper lobe subsegmental bronchi, resulting in appearance that mimics a nodule
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
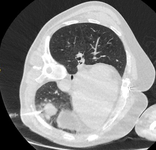
PET CT scan with 18-fluorodeoxyglucose (18-FDG) showing a low uptake in a semi-solid right upper lobe posterior lesion. Surgical resection confirmed adenocarcinoma with primarily lepidic pattern
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:

Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a left upper lobe spiculated nodule with a pleural ‘tag’. Resection histopathology confirmed a moderately-differentiated squamous cell lung cancer
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) section with soft tissue configuration, showing a right lung hamartoma, as incidental finding in an asymptomatic patient. Note the central calcification and several small spots of fat within the nodule. This nodule was stable over a 12 year period and no intervention required
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
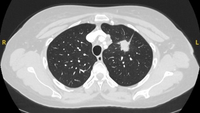
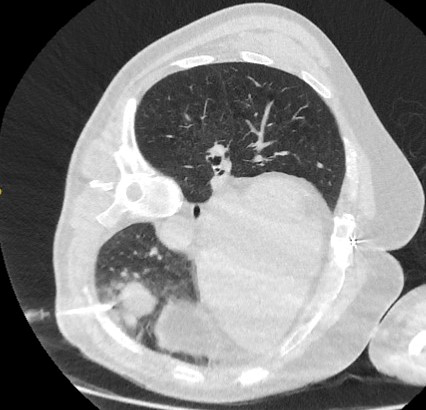
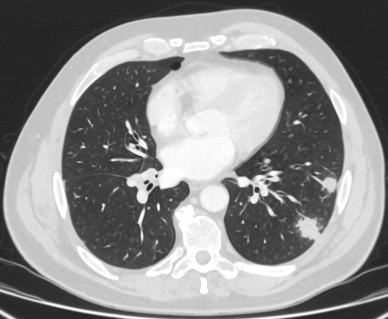
Computed tomography (CT) sections with examples of semi-solid solitary nodules
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
A-D: calcification patterns of benign nodules; E, F: may be seen in malignant nodules
Mazzone P.J., Stoller J.K. Semin Thorac Cardiovasc Surg. 2002;14:250-260; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a left upper lobe peripheral elongated nodule, with contrast enhancement and a clear feeding and draining side, consistent with a small arteriovenous malformation
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) showing two left lower lobe peripheral nodules (one slightly spiculated and the other with smoother margins) in a patient presenting with fever, high inflammatory serum markers, and blood cultures confirming Streptococcus intermedius. Both nodules completely resolved following a course of linezolid, consistent with septic emboli
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a posterior left upper lobe spiculated nodule, with ‘bronchus sign’ in a female non-smoker. Bronchoscopic forceps biopsy and brushing assisted by radial EBUS miniprobe localisation, confirmed a non-Hodgkin’s lymphoma
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Computed tomography (CT) showing a benign calcified granuloma in the right middle lobe, stable >10 years. The patient reported previous pneumonia on the same side
From the collection of Dr George Tsaknis, MD, PhD, FRCP(London), MRQA, MAcadMEd, PGCert; used with permission
See this image in context in the following section/s:
Assessment of solitary pulmonary nodule
Sub-solid pulmonary nodules algorithm. PSNs, part solid nodules; SSN, sub-solid nodules
Callister MEJ et al. Thorax 2015;70:ii1-ii54; used with permission
See this image in context in the following section/s:
Use of this content is subject to our disclaimer