Approach
For information on diagnosis of Fusarium fungal meningitis associated with procedures performed under epidural anesthesia in Matamoros, Mexico, see specific guidance. Fungus Education Hub: interim recommendations for diagnosis and management of cases of fungal meningitis associated with epidural anesthesia administered in Matamoros, Mexico Opens in new window
Diagnosis involves collation of symptoms, signs, and investigation results. Often, empiric treatment may need to be initiated before definitive diagnosis is made.
Key tests include brain imaging, cerebrospinal fluid (CSF) analysis, and blood cultures. If repeated examination of the CSF, blood, and urine remains inconclusive, histopathologic examination for fungi and culture of the brain, meninges, and cisternal or ventricular fluid may be considered.[27]
Clinical history
Cryptococcal meningitis
May present in a variety of ways; clinical features are not specific.
Meningoencephalitis is the most frequent manifestation of cryptococcosis.
HIV-infected individuals and organ transplant recipients are the major risk groups, but it can also present in immunocompetent adults and children.
Typically presents with progressive headache (70% to 90%), and fever (50% to 90%) of several weeks' duration.[59][61]
Symptoms may progress to include nausea, vomiting, behavioral change, drowsiness, and seizures.
Diplopia and subsequently reduced visual acuity reflect the development of elevated intracranial pressure.
Cough and dyspnea are not infrequent and may reflect pulmonary involvement.
The rate of progression of symptoms may depend on host immunity so that some patients without major immune deficits present a more chronic course.
Significant incidence and higher mortality when associated with immune reconstitution inflammatory syndrome after initiation of antiretroviral therapy.[77]
Histoplasmal meningitis
Fever, headache, and neck stiffness due to a subacute or chronic meningitis.[27]
Focal neurologic symptoms due to focal brain or spinal cord lesions and stroke syndromes.[27]
Behavioral and mental status changes secondary to encephalitis.[27]
Patients with central nervous system (CNS) involvement associated with disseminated infection may also report high fevers, weight loss, and mouth ulcers.
Coccidioidal meningitis
Headache, fever, nausea, vomiting, and behavioral changes.[78]
The most common complication of coccidioidal meningitis is hydrocephalus, which can occur as a presenting feature or as a late complication.[11]
Symptoms of hydrocephalus include headache, nausea, blurred or double vision, coordination or gait disturbance, memory loss, confusion, changes in personality, and urinary incontinence.
May also present with focal neurologic symptoms secondary to cerebral infarction due to arteritis of small- to mid-sized blood vessels.
Candidal meningitis
Adult candidal meningitis may present with acute or subacute symptoms of meningitis, with fever and headache being the most common reported symptoms.[79]
Neonates with candidal meningitis are often premature and present initially with symptoms of respiratory distress.[35][36][37]
Mucormycosis
Rhino-orbito-cerebral disease commonly presents with facial pain, sinusitis, eye pain, blurred vision, and proptosis. Any of these clinical findings in a patient with diabetes necessitates prompt investigation for mucormycosis.[46]
Clinical signs
Cryptococcal meningitis
Signs may be absent or minimal.
Meningismus is only present in 20% to 50% of patients on presentation.[59][61]
Additional signs may include: altered mental status, reduced visual acuity, papilledema, cranial nerve palsies, and other focal neurologic deficits.
In children, headache and fever are most common symptoms.[80]
Atypical features include subacute dementia and visual loss.
Histoplasmal meningitis
Meningismus and focal neurologic signs.
Signs of disseminated histoplasmosis include splenomegaly, hepatomegaly, and lymphadenopathy.
Histoplasmosis is the most endemic mycosis in Europe.[81]
Coccidioidal meningitis
Meningismus (about 50%).[82]
Signs of hydrocephalus (altered mental status and gait).
Focal neurologic signs related to cerebral infarction.
Candidal meningitis
Meningismus may be found, although it is not common in neurosurgical patients with candidal meningitis.
Patients commonly present with altered mental status.
Focal clinical presentations, cranial nerve involvement, papilledema, and seizures are uncommon manifestations of candidal meningitis.
An examination of the patient should be performed looking for signs of disseminated candidiasis. For example, fundoscopy may reveal invasion of the retina; the Infectious Diseases Society of America recommends at least one ophthalmologic examination in patients with suspected disseminated candidiasis.[75]
Mucormycosis
A specific sign in the later stages of mucormycosis infection is necrotic eschar on the skin, palate, or nasal turbinates.[46]
Investigations
Brain imaging with computed tomography (CT) or magnetic resonance imaging is performed in all patients with suspected fungal meningitis.[Figure caption and citation for the preceding image starts]: Cryptococcal meningoencephalitis. (A) Cranial magnetic resonance imaging (MRI) shows cerebellar hyperintensities (arrows) in FLAIR sequences (fluid-attenuated inversion recovery) and (B) meningeal contrast enhancement (arrows) in T1 weighted MRI. (C) Indian ink stain, (D) fungal culture, and (E) Gram stain of cerebrospinal fluid were positiveBraun J. Headache, personality changes and fine motor disturbances. BMJ Case Reports. 2009; doi:10.1136/bcr.06.2008.0093. Used with permission. [Citation ends].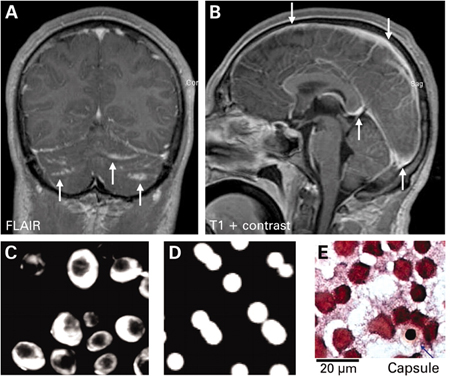 If cryptococcal meningitis is suspected, imaging should always precede lumbar puncture.[83] Imaging may be normal or may demonstrate, for example, communicating hydrocephalus (also common with coccidioidal meningitis), fungal granuloma, or vasculitic complications. The role of 18F-fluorodeoxyglucose positron emission tomography (PET)/CT in the diagnosis and management of fungal meningitis is being explored.[84][85]
If cryptococcal meningitis is suspected, imaging should always precede lumbar puncture.[83] Imaging may be normal or may demonstrate, for example, communicating hydrocephalus (also common with coccidioidal meningitis), fungal granuloma, or vasculitic complications. The role of 18F-fluorodeoxyglucose positron emission tomography (PET)/CT in the diagnosis and management of fungal meningitis is being explored.[84][85]
Lumbar puncture is part of the routine evaluation. CSF is tested for glucose, white blood cell count and differential, protein, culture, antibodies/antigens, India ink stain (Cryptococcus), and opening pressure. However, repeated sampling of large volumes of CSF is often required for the diagnosis of non-HIV-associated cryptococcal meningitis, coccidioidal meningitis, histoplasmosis, candidal meningitis, and Aspergillus meningitis. Culture positivity of Aspergillus meningitis is reported in less than one third of all cases but galactomannan antigen test in CSF has a higher sensitivity.[54][86] Cryptococcal meningitis by noncapsulated forms of cryptococci is rare but would be difficult to diagnose without CSF culture.[87]
Up to three sets of blood cultures should be taken in all patients; they may be positive when candidal, histoplasmal, or cryptococcal meningitis is associated with disseminated disease.
Specific tests include:
CSF cryptococcal antigen test.
Serum antibody and antigen testing for histoplasmosis.
Urine antigen testing for histoplasmosis.
Immunodiffusion tests (IgM and IgG) and the complement fixation test (IgG) for coccidioidomycosis: positive results support the diagnosis of coccidioidal meningitis when other causes of meningitis are excluded, and the presence of coccidioidal IgG antibody in the CSF is virtually diagnostic of coccidioidal meningitis.[11] Negative results from an experienced laboratory in patients with untreated disseminated disease are rare.
Positive cultures together with microscopy and immunological testing in serum and CSF remain the current standard for diagnosis of fungal CNS infections. However, specific diagnosis may be delayed due to slow growth in culture, cross-reactivity in case of antigen detection, and inadequate antibody response.
There are early data favoring CSF polymerase chain reaction as an adjunctive diagnostic tool.[88][89] Emerging data also suggest that CSF (1-3)-beta-D-glucan may play a role in the diagnosis of fungal meningitis.[90] During the 2012 Exserohilum rostratum meningitis outbreak from contaminated methylprednisolone, CSF (1-3)-beta-D-glucan also demonstrated potential utility in monitoring treatment response.[91]
Histopathologic examination
If repeated examination of the CSF, blood, and urine remains inconclusive, histopathologic examination for fungi and culture of the brain, meninges, and cisternal or ventricular fluid may be considered.[27] Meningeal biopsy or stereotactic lesional biopsy of intracranial mass may allow specific pathogen diagnosis in appropriate cases of chronic meningitis.
Use of this content is subject to our disclaimer