Tests
1st tests to order
erythrocyte sedimentation rate (ESR)
Test
The World Health Organization criteria include only elevated ESR or leukocyte count as acute-phase reactants. The Jones criteria include only elevated CRP or elevated ESR.[2]
Australian data found that CRP and ESR were commonly elevated in patients with confirmed acute rheumatic fever (excluding chorea), whereas the leukocyte count usually was not elevated.[64] By contrast <4% of patients had both a serum CRP level of <3 mg/dL and an ESR of <30 mm/hour.[60][64]
Result
≥60 mm/hour (low-risk populations) or ≥30 mm/hour (moderate- to high-risk populations) is taken as evidence of elevated inflammatory markers (minor criterion)
CRP
Test
The World Health Organization criteria include only elevated erythrocyte sedimentation rate (ESR) or leukocyte count as acute-phase reactants. The Jones criteria include only elevated CRP or elevated ESR.[2]
Australian data found that CRP and ESR were commonly elevated in patients with confirmed acute rheumatic fever (excluding chorea), whereas the leukocyte count usually was not elevated.[64] By contrast <4% of patients had both a serum CRP level of <3 mg/dL and an ESR of <30 mm/hour.[60][64]
Result
≥3 mg/dL is taken as evidence of elevated inflammatory markers (minor criterion)
WBC count
Test
The World Health Organization criteria include only elevated erythrocyte sedimentation rate (ESR) or leukocyte count as acute-phase reactants. The Jones criteria include only elevated CRP or elevated ESR.[2]
Australian data found that CRP and ESR were commonly elevated in patients with confirmed acute rheumatic fever (excluding chorea), whereas the leukocyte count usually was not elevated.[64] Only 25% of patients with acute rheumatic fever had a leukocyte count >15 x 10⁹/L, and only 7% had a count >20 x 10⁹/L. The authors do not suggest including elevated leukocyte count as an acute-phase reactant.
Result
may be elevated, but not recommended as meeting the minor criterion
blood cultures
Test
Useful, if patient is febrile, to exclude bacteremia. Both osteoarticular infection and infective endocarditis may present in similar patterns to acute rheumatic fever.
Result
no growth
electrocardiogram
Test
The duration of the PR interval increases with age; therefore, it is important to use age-standardized values.
Some healthy people have benign and incidental first-degree heart block, but a prolonged PR interval that resolves over 2-3 weeks may be a useful diagnostic feature in cases when the other clinical features are not definitive. First-degree heart block sometimes leads to a junctional rhythm, usually with a heart rate similar to the sinus rate. Second-degree and even complete block (also known as advanced atrioventricular block) are less common but can occur. In a resurgence of acute rheumatic fever in the US, 32% of patients had abnormal atrioventricular conduction, usually a prolonged PR interval.[11][Figure caption and citation for the preceding image starts]: ECG showing heart block in acute rheumatic feverAust N Z J Med. 1996 Apr;26(2):241-2; used with permission [Citation ends].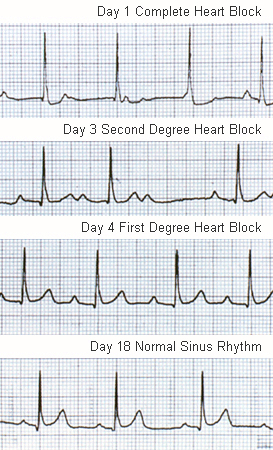
Result
prolonged PR interval is a minor criterion of acute rheumatic fever
chest x-ray
Test
A chest x-ray should be performed in all cases in which carditis is suspected. Cardiomegaly and/or congestive heart failure in acute rheumatic fever as seen on chest x-ray, results from severe valvular dysfunction secondary to valvulitis. Pericardial effusion should also be considered in cases where significant cardiomegaly is present.[77][Figure caption and citation for the preceding image starts]: Chest x-ray of biventricular heart failure due to acute carditis in rheumatic feverLancet. 2006 Jun 24;367(9528):2118; used with permission [Citation ends].
Result
may demonstrate chamber enlargement and congestive cardiac failure
echocardiogram
Test
An echocardiogram improves the specificity of the clinical diagnosis (e.g., suspected mitral regurgitation may in fact be a flow murmur or even congenital heart disease on echocardiography).[58]
It may also improve sensitivity, as increasing recognition is being given to the phenomenon of subclinical carditis (pathological regurgitation detected on echocardiography in the absence of clinical findings) occurring in approximately 17% of cases of acute rheumatic fever.[67][68][78][79]
In addition to improving specificity and sensitivity, echocardiography also enables more accurate grading of the severity of carditis and can evaluate cardiac dimensions and function.
The interpretation of echocardiography in patients with rheumatic fever requires a great deal of expertise.
There are published morphological and Doppler findings that are characteristic of rheumatic carditis.[2]
Result
may reveal morphological changes to the mitral and/or aortic valves; severity of regurgitation (mitral, aortic, and tricuspid); pericardial effusion if pericarditis present
throat culture
Test
A throat culture should be sent in all patients with acute rheumatic fever. However, <10% of throat cultures are positive for group A streptococci, reflecting the postinfectious nature of the disease; group A streptococci have usually been eradicated before onset of the disease.[69]
Result
growth of beta-hemolytic group A streptococci
rapid antigen test for group A streptococci
Test
If available, a rapid antigen test can be performed; however, data from New Zealand suggest that some of the tests may perform poorly compared with throat cultures.[80]
Result
positive
anti-streptococcal serology
Test
Positive serology is the most important means of demonstrating antecedent infection. The most commonly used tests are the anti-streptolysin O titer and the anti-deoxyribonuclease B titer. It is generally recommended that paired titers be taken: an acute titer and a convalescent titer (usually taken 14-28 days after the initial sample). Elevated titers and/or a 4-fold rise or fall in titers are required as proof of a recent immunologic response to group A streptococcal infection. The upper limit of normal is different between regions, but has been defined for the US and Australian pediatric population.[81][82]
Result
above normal range (region dependent)
Use of this content is subject to our disclaimer