History and exam
Key diagnostic factors
common
dyspnea on exertion
There are no pathognomonic features to diagnose MR by history; however, this is a common presenting symptom of mitral regurgitation.
decreased exercise tolerance
There are no pathognomonic features to diagnose MR by history; however, this is a common presenting symptom of mitral regurgitation.
lower extremity edema
There are no pathognomonic features to diagnose MR by history; however, this is a common presenting symptom of mitral regurgitation.
holosystolic murmur
MR usually presents as a holosystolic, blowing murmur at the apex that radiates to the axilla.
Auscultation sounds: Mitral regurgitation (severe)
Other diagnostic factors
common
fatigue
There are no pathognomonic features to diagnose MR by history; however, this is a common presenting symptom of mitral regurgitation.
displaced point of maximal impulse
Indicates severe and chronic MR.
uncommon
orthopnea
There are no pathognomonic features to diagnose MR by history; however, this is a common presenting symptom of mitral regurgitation.
paroxysmal nocturnal dyspnea
There are no pathognomonic features to diagnose MR by history; however, this is a presenting symptom of mitral regurgitation.
palpitations
There are no pathognomonic features to diagnose MR by history; however, this is a presenting symptom of mitral regurgitation.
diaphoresis
In severe cases, usually with acute MR.
pulmonary closure is louder than aortic closure
Occurs as right-sided pressures increase.
S3 heart sound
Occurs in the presence of left ventricular dysfunction.
Auscultation sounds: Third heart sound gallop
diminished S1 heart sound
Chronic MR is also associated with laterally displaced apical impulse (with left ventricular dilation) and diminished S1.
Risk factors
strong
mitral valve prolapse
May result from abnormal elasticity with redundancy and enlargement of various portions of the mitral valvular apparatus, including the mitral annulus, chordae tendineae, and leaflets.[5][6][7][Figure caption and citation for the preceding image starts]: Posterior mitral valve prolapse on M-mode echoFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].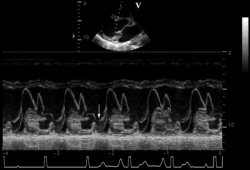 [Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal long-axis view showing posterior mitral leaflet prolapseFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends]. [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 2D viewFrom the collection of Prakash P. Punjabi [Citation ends].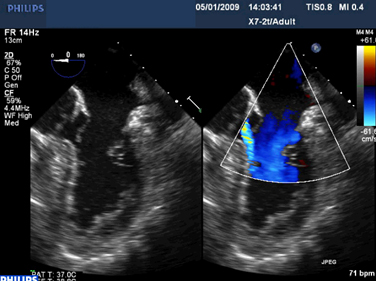 [Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
[Figure caption and citation for the preceding image starts]: Mitral valve P2 leaflet prolapse: 3D viewFrom the collection of Prakash P. Punjabi [Citation ends].
history of rheumatic heart disease
Leads to leaflet thickening and valvular and subvalvular fibrosis, and various degrees of systolic and diastolic restriction of leaflet motion.
In most cases of restriction involving both leaflets, the jet of MR is central. In some patients, the posterior leaflet is more restricted and the jet direction is posterior.
infective endocarditis
There is leaflet or chordal disruption, flail, and perforations. These often cause MR with associated nodular hypermobile densities (vegetations) that are the echocardiographic hallmarks of the disease.
history of cardiac trauma
Sharp or blunt trauma may result in structural damage to the mitral valve apparatus.
history of myocardial infarction
Myocardial infarction may result in structural damage to the mitral valve apparatus.
history of congenital heart disease
Such as anterior mitral valve cleft, which is commonly associated with septum primum atrial septal defect.
history of ischemic heart disease
In the setting of myocardial infarction and ischemic heart disease, the left ventricle undergoes remodeling and enlargement, which leads to MR. This is caused by apical tethering of normal leaflets.
The length of mitral tissue, including the leaflets, chordae, and papillary muscle, is fixed. As the left ventricle dilates, often after myocardial infarction, the left ventricular wall and papillary muscles are displaced outward, which tethers the joining surfaces of the mitral valve downward, reducing the amount of leaflet tissue available for coaptation.
In many cases, the result is a central, or in some cases a posterior, direction of the MR jet.
In rare cases, a focal infarction may cause elongation or disruption of the papillary muscle, leading to excessive leaflet motion (often involving both leaflets), most commonly on the medial side of both leaflets from medial papillary muscle abnormalities.
left ventricular systolic dysfunction
The mechanism for this risk factor is the same as for ischemic heart disease.
hypertrophic cardiomyopathy
Caused by systolic anterior motion of the mitral valve.[Figure caption and citation for the preceding image starts]: Apical 3-chamber view of hypertrophic cardiomyopathy with systolic anterior motionFrom the collection of Samir Kapadia and Mehdi H. Shishehbor [Citation ends].
anorectic/dopaminergic drugs
Certain anorectic and other dopaminergic or serotonergic drugs such as ergotamine, pergolide, and cabergoline have been shown to cause MR.
Use of this content is subject to our disclaimer

