Differentials
Common
Acute coronary syndrome
History
central chest pressure, squeezing, or heaviness; radiation to jaw or upper extremities; associated nausea, vomiting, dyspnea, dizziness, weakness; occurs at rest or accelerating tempo (crescendo); risk factors: smoking, age (men >45, women >55 years), positive family history of premature coronary artery disease, hypertension, hyperlipidemia, diabetes, stroke, or peripheral arterial disease; preeclampsia, gestational diabetes, polycystic ovary syndrome, early menopause and autoimmune diseases are additional risk factors in women; women, older people (>75 years), and people with diabetes may be more likely to present with atypical symptoms such as nausea or dyspnea
Exam
exam may be normal; jugular venous distention, S4 gallop, holosystolic murmur (mitral regurgitation), bibasilar rales; hypotensive, may be tachycardic, bradycardic, or hypoxic depending on severity of ischemia
1st investigation
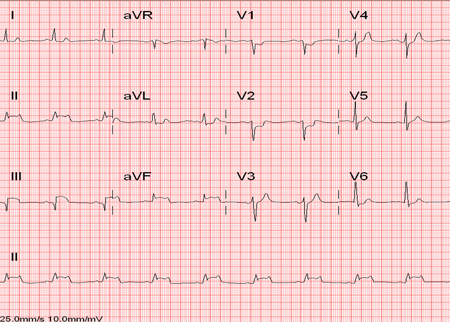
- ECG:
ST-elevation myocardial infarction (STEMI): ST-segment elevation >1 mm in ≥2 anatomically contiguous leads or new left bundle-branch block; non-STEMI (NSTEMI) or unstable angina: nonspecific; ST-segment depression or T-wave inversion
More - chest x-ray:
normal or signs of heart failure, such as increased alveolar markings, blood diversion to upper lobes, cardiomegaly, Kerley B lines, pleural effusions
More - cardiac biomarkers:
elevated in STEMI and NSTEMI; not elevated in unstable angina
More
Stable angina
History
may be known history of coronary artery disease; chest discomfort on exertion, relieved by nitroglycerine or rest; no change in intensity, frequency, or duration; no associated diaphoresis, nausea/vomiting, or shortness of breath; risk factors: smoking, age (men >45, women >55 years), positive family history of premature coronary artery disease (CAD), hypertension, hyperlipidemia, diabetes, stroke, or peripheral arterial disease
Exam
no specific findings for CAD, may have abnormal pulses if peripheral vascular disease present
1st investigation
- ECG:
no acute changes; may have evidence of previous infarction, such as Q waves
- chest x-ray:
normal or cardiomegaly
- cardiac biomarkers:
not elevated
Other investigations
- stress testing:
≥1 mm of horizontal or down-sloping ST-segment depression or ST-segment elevation during or after exercise is considered positive for ischemia; high-risk disease: regional wall motion abnormalities and left ventricular dysfunction
More - coronary angiography:
evidence of coronary artery narrowing
More - CT coronary angiography:
identification of stenosis
More
Pneumonia
History
productive or dry cough, fever, pleuritic pain associated with shortness of breath; may have rigors, myalgias, and arthralgias; may be recent history of travel or infectious exposures
Exam
decreased breath sounds, rales, wheezing, bronchial breath sounds, dullness to percussion, and increased tactile fremitus observed with severe consolidation
1st investigation
- chest x-ray:
pulmonary infiltration, air bronchograms, and/or pleural effusion
Other investigations
- CBC:
elevated white blood cell count with left shift (increased neutrophil count)
- sputum culture:
may reveal culprit organisms, but not sensitive or specific; recommended in patients with severe disease as well as in all patients empirically treated for MRSA or Pseudomonas aeruginosa
More - blood culture:
may reveal culprit organisms, but not sensitive or specific; recommended in patients with severe disease as well as in all patients empirically treated for MRSA or P aeruginosa
More
Viral pleuritis
History
prodrome of viral illness (myalgias, malaise, rhinorrhea, cough, nasal congestion, low-grade temperatures); sick contacts
Exam
pleural friction rub with or without low-grade fever; sometimes reproducible tenderness to palpation of chest when perichondritis or pleurodynia accompanies pleuritis
1st investigation
- chest x-ray:
usually normal but can uncommonly have effusion
More
Other investigations
- CBC:
normal, or leukocytosis with lymphocytic predominance
GERD
History
may have chest pain, typically retrosternal burning with eating large or fatty meals that can be reproduced with lying supine and relieved by sitting up; relieved by antacids; reflux symptoms
Exam
no specific physical findings
1st investigation
- therapeutic trial of proton-pump inhibitor:
relief of symptoms with 8-week trial of proton-pump inhibitor
More
Other investigations
- esophagogastroduodenoscopy:
esophageal inflammation or erosions
More
Costochondritis
History
focal chest wall pain, may have known precipitating injury; aggravated by sneezing, coughing, deep inspiration, or twisting of the chest
Exam
reproducible pain on chest wall palpation, especially at the costochondral junctions
1st investigation
- none:
clinical diagnosis
More
Other investigations
- chest x-ray:
no specific findings
More
Anxiety or panic disorder
History
sharp chest pain with anxiety, dizziness or faintness, palpitations, sweating, trembling or shaking, fear of dying or going insane, paresthesiae, chills or hot flashes, breathlessness or choking sensation
Exam
hyperventilation, exam otherwise normal
1st investigation
- ECG:
normal
Other investigations
- chest x-ray:
normal
- HADS (hospital anxiety and depression scale) score:
may have a score >11
Uncommon
Pulmonary embolism
History
chest pain that is sharp and pleuritic in nature; shortness of breath; hemoptysis may occur if pulmonary infarction develops; massive pulmonary embolism (PE) results in syncope; risk factors: history of immobilization, orthopedic procedures, oral contraceptive use, previous PE, hypercoagulable states, or recent travel over long distances; unilateral swollen lower leg that is red and painful suggests deep venous thrombosis; use of the Wells (or Geneva) Score can help to categorize the patient as "PE likely" (Wells Score >4) or "PE unlikely"
Exam
may have tachycardia, loud P2, right-sided S4 gallop, jugular venous distention, fever, right ventricular lift; massive PE may cause hypotension
1st investigation
- ECG:
sinus tachycardia; usually nonspecific but may show S1, Q3, and T3 pattern
- D-dimer:
nonspecific if positive; PE excluded if result negative in patients with low probability of having a PE
More - chest x-ray:
may show decreased perfusion in a segment of pulmonary vasculature (Westermark sign); may show pleural effusion
- CT pulmonary angiography:
may identify thrombus in the pulmonary circulation
More
Pericarditis
History
usually viral prodrome; sharp pleuritic chest discomfort provoked by lying supine and improved with sitting up; associated dry cough, fever, myalgias, or arthralgias; history of possible causes such as radiation exposure, collagen vascular disease, recent myocardial infarction, or uremia
Exam
tachycardia and friction rub; jugular venous distention and pulsus paradoxus indicate effusion causing tamponade
1st investigation
- ECG:
diffuse concave-up ST-elevation, associated PR depression; changes evolve over time
More
Other investigations
- chest x-ray:
usually normal; enlarged cardiac silhouette (globular heart) if pericardial effusion present
- echocardiography:
normal or shows small effusion
Cardiac tamponade
History
history of underlying cause such as myocardial infarction, aortic dissection, or trauma; may present insidiously as a result of hypothyroidism or pericarditis; dizziness; dyspnea; fatigue
Exam
hypotension, distended neck veins, muffled heart sounds; pulsus paradoxus (a drop of ≥10 mmHg in arterial blood pressure on inspiration)
1st investigation
- ECG:
low-voltage QRS; electrical alternans; other changes depend on underlying cause (e.g., ST elevation in acute myocardial infarction or nonspecific ST changes in pericarditis)
- chest x-ray:
globular heart (if large effusion)
More - echocardiography:
pericardial effusion causing collapse of great vessels, atria, and ventricles
Other investigations
Aortic dissection
History
acute substernal tearing sensation, with radiation to interscapular region of the back; pain may migrate with the propagation of the dissection; stroke, acute myocardial infarction due to obstruction of aortic branches; dyspnea due to acute aortic regurgitation; hypotension due to cardiac tamponade; history of hypertension, Marfan syndrome, Ehlers-Danlos syndrome, or syphilis
Exam
unequal pulses or blood pressures in both arms; new diastolic murmur due to aortic regurgitation; muffled heart sounds if the dissection is complicated by cardiac tamponade; new focal neurologic findings due to involvement of the carotid or vertebral arteries
1st investigation
- chest x-ray:
widened mediastinum
More
Other investigations
- transesophageal echocardiography:
false lumen or flap in the ascending or descending aorta; new aortic regurgitation or pericardial tamponade
- CT chest with contrast:
false lumen or flap in the ascending or descending aorta
- MRI angiography:
false lumen or flap in the ascending or descending aorta
More
Aortic stenosis
History
age >60 years; typical angina; chest pain is usually progressive; shortness of breath; syncope (if severe); patients with significant aortic stenosis and heart failure are at high risk of cardiogenic shock or sudden death
Exam
ejection systolic murmur that radiates to the neck; obliteration of S2 indicates severe stenosis; delayed upstroke on palpation of carotid pulse
1st investigation
- ECG:
voltage criteria for left ventricular hypertrophy; enlarged P wave suggesting left atrial enlargement
Other investigations
- chest x-ray:
calcified aortic valve; pulmonary edema
- echocardiogram:
poor excursion of aortic valve leaflets; elevated velocities through the aortic valve; possible left ventricular systolic dysfunction
Mitral valve prolapse
History
usually asymptomatic, but may cause palpitations, chest pain, dyspnea, headache, or fatigue
Exam
midsystolic click and late systolic murmur at the apex
1st investigation
- ECG:
usually normal, may show atrial fibrillation or other arrhythmias
Other investigations
- chest x-ray:
usually normal, may show enlarged pulmonary artery or left atrium
- echocardiogram:
mitral regurgitation and valve prolapse
Pneumothorax
History
acute, pleuritic chest pain, shortness of breath; primary spontaneous between ages 20 and 40 years; secondary spontaneous in patients with COPD; traumatic due to acute trauma or iatrogenic; shock may occur if rapidly increasing (tension pneumothorax)
Exam
absent breath sounds, increased resonance to percussion; jugular venous distention, tracheal deviation, and hypotension if tension pneumothorax (due to compromise of the great vessels)
1st investigation
- chest x-ray:
air in the pleural space, visible pleural line from collapsed lung, or mediastinal shift
More
Other investigations
Pulmonary hypertension
History
cardiac-sounding chest pain on exertion, dyspnea; palpitations, fatigue; symptoms of right-sided heart failure such as lower extremity edema, abdominal bloating, or ascites; syncope if severe
Exam
accentuated pulmonic component (P2) to the second heart sound; palpable P2; right ventricular heave; lower extremity edema; jugular venous distention
1st investigation
- ECG:
right axis deviation; right ventricular hypertrophy or right atrial enlargement
Other investigations
- chest x-ray:
large, prominent pulmonary arteries
- echocardiogram:
tricuspid regurgitation; estimated right ventricular systolic pressure >35 mmHg; right ventricular and right atrial dilation; pericardial effusion
Peptic ulcer disease
History
gastric ulcers: epigastric pain or burning with onset 5 to 15 minutes after eating and may last for several hours; duodenal ulcers: epigastric pain is relieved by eating and may return 1 to 4 hours postprandially; pain from any ulcer is relieved by antacid; risk factors: cigarette smoking, nonsteroidal anti-inflammatory drugs, and chronic alcohol consumption
Exam
epigastric tenderness; if significant bleeding is present there may be tachycardia, hypotension, and conjunctival pallor
1st investigation
- esophagogastroduodenoscopy:
gastric or duodenal erosions or ulceration
Other investigations
- Helicobacter pylori urea breath test or stool antigen test:
may be positive
More
Esophageal spasm
History
crushing substernal chest pain, associated dysphagia, pain does not always correlate with swallowing, dysphagia precipitated by very hot or cold foods, nitroglycerin can relieve the pain
Exam
no specific findings
1st investigation
- barium swallow:
corkscrew or rosary bead appearance on barium swallow
Other investigations
- esophageal manometry:
simultaneous contractions on >30% of wet swallows
Acute cholecystitis
History
right upper quadrant pain, radiation to interscapular area or right shoulder, associated with nausea and vomiting, fevers, anorexia often accompanies pain, signs of peritoneal inflammation such as abdominal pain with jarring
Exam
right upper quadrant tenderness (Murphy sign), abdominal rigidity and guarding if perforation of the gallbladder, rarely have jaundice early in the course of cholecystitis
1st investigation
Other investigations
- hydroxy-iminodiacetic acid (HIDA) scan:
decreased radionuclide uptake in the gallbladder due to cystic duct obstruction
More
Acute pancreatitis
History
epigastric or periumbilical abdominal pain that radiates to the back; may be severe; associated nausea and vomiting; history of alcohol consumption or gallstones
Exam
tachycardic, hypotensive, febrile, acute distress; ecchymosis in the periumbilical region (Cullen sign) and the flank (Grey-Turner sign)
1st investigation
- serum lipase or amylase:
>3 times the upper limit of the normal range
More
Other investigations
- CBC:
leukocytosis
More - electrolytes and renal function:
elevated creatinine, high anion gap
- ABG:
acidosis, low pH
More - abdominal ultrasound:
determines possible cause, such as gallstones
More - abdominal CT scan:
stage the severity of the pancreatitis; pancreatic necrosis; pseudocyst
More - magnetic imaging/magnetic resonance cholangiopancreatography (MRI/MRCP):
findings may include stones, tumors, diffuse or segmental enlargement of the pancreas with irregular contour and obliteration of the peripancreatic fat, necrosis, or pseudocysts
More
Herpes zoster
History
unilateral, burning pain in typical dermatome distribution that may occur before appearance of rash and may persist for more than 1 month
Exam
vesicular rash on erythematous base, in unilateral distribution of a dermatome
1st investigation
- none:
diagnosis is clinical
Other investigations
- swab for viral culture and polymerase chain reaction (PCR):
varicella-zoster positive on culture, immunofluorescence, or PCR
Gastritis
History
dyspepsia/epigastric discomfort; nausea, vomiting, loss of appetite; history of nonsteroidal anti-inflammatory drug use or alcohol misuse; history of Helicobacter pylori infection; history of previous gastric or abdominal surgery
Exam
epigastric gastric discomfort may be present; may have signs associated with vitamin B12 deficiency and pernicious anemia (e.g., abnormal neurologic exam, presence of cognitive impairment, angular cheilitis, atrophic glossitis
1st investigation
- Helicobacter pylori urea breath test:
positive in H pylori infection
Other investigations
- esophagogastroduodenoscopy:
results can be variable; may show atrophy and/or erosions
- gastric mucosal biopsy:
variable; positive for H pylori; features of acute or chronic gastritis
E-cigarette or Vaping product use Associated Lung injury (EVALI)
History
dyspnea, chest pain, cough, hemoptysis, e-cigarette/vaping use in last 90 days (particularly cannabis) frequently associated abdominal pain, nausea, vomiting, and diarrhea
Exam
tachycardia, tachypnea, fever, hypoxemia
1st investigation
- CBC:
leukocytosis with neutrophil predominance
- comprehensive metabolic panel:
inflammatory markers (ESR, CRP, Procalcitonin) may be elevated
- urine toxicology:
may be positive for cannabis
- CXR:
basilar predominance with subpleural sparing
Other investigations
- blood cultures, respiratory viral testing:
excludes infectious causes
- CT chest:
may show bilateral, diffuse, ground-glass infiltrates with basilar predominance and subpleural sparing
- bronchoalveolar lavage:
cell count often reveals a neutrophilic predominance
More
Vasospastic angina
History
characteristic chest pain usually nocturnal, between 12 a.m. and 8 a.m., relieved by nitrates; cluster pattern of pain, dyspnea, palpitations, presyncope, nausea, diaphoresis, waxing and waning episodes
Exam
diaphoresis and tachycardia may be present; otherwise exam is usually unremarkable
1st investigation
- ECG:
may show ST-elevation or ST-depression, especially during episodes of pain
- CBC, basic metabolic panel, cardiac troponins:
important to exclude other causes of pain
- CXR:
important to exclude other causes of pain
Other investigations
- coronary angiography with provoked arterial spasm:
coronary artery spasm
More
Use of this content is subject to our disclaimer