Tests
1st tests to order
Tests to consider
chest x-ray
Test
Reserve chest radiography for any patient who is hospitalized for severe or complicated CAP.[1][3][9] It may also be indicated if the child fails to respond to initial outpatient treatment.[18]
Avoid routine chest radiography in children referred to the hospital with CAP.[3][9] There is poor correlation between x-ray appearance and clinical signs and outcome. The main role of imaging in CAP is to detect complications such as pleural effusion, lung abscess, and bronchopleural fistula.[18]
Do not order chest x-rays to confirm suspected CAP in a child who is assessed as well enough to be treated as an outpatient (based on evaluation in the community or in a hospital emergency department).[1][9]
[Figure caption and citation for the preceding image starts]: Chest radiographs confirming pneumonia. Image A: a 6-year-old girl with widespread interstitial changes in both lungs caused by S pneumoniae. Image B: a 1-year-old boy with alveolar changes in the right lower lobe caused by S pneumoniae. Image C: a 2-year-old girl with alveolar changes in the left lower lobe associated with rhinovirus. Image D: a 4-month-old girl with alveolar changes in the right upper lobe associated with parainfluenza 2 and human herpes virusVirkki R, et al. Thorax 2002; 57: 438-41; used with permission [Citation ends].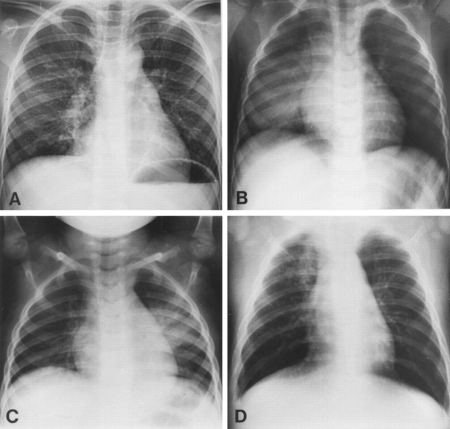 [Figure caption and citation for the preceding image starts]: Chest x-ray of complicated pneumonia, showing opacification of the left lung field consistent with a large pleural effusion and empyema. There is associated right-sided bronchial wall thickening and consolidationHaq IJ, et al. BMJ 2017 Mar 2; 356: j686. doi: 10.1136/bmj.j686; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray of complicated pneumonia, showing opacification of the left lung field consistent with a large pleural effusion and empyema. There is associated right-sided bronchial wall thickening and consolidationHaq IJ, et al. BMJ 2017 Mar 2; 356: j686. doi: 10.1136/bmj.j686; used with permission [Citation ends].
Result
consolidation, opacity, or infiltrate provides radiographic confirmation of pneumonia in the presence of typical symptoms/signs; may reveal signs of complicated CAP (e.g., parapneumonic effusion, lung abscess)
CBC
Test
Order for any patient with severe pneumonia. Interpret the results in the context of the clinical exam and other laboratory and imaging studies.[1][9]
Routine CBC is not needed in children with suspected CAP who are managed in the community.[1]
Note that the combination of mild anemia and hypoalbuminemia are characteristic signs of necrotizing pneumonia.[2]
Result
WBC count is typically elevated, but the degree of elevation does not reliably distinguish bacterial from viral infection; anemia or thrombocytopenia may raise concern for hemolytic-uremic syndrome, a rare complication of pneumococcal pneumonia
serum electrolytes/BUN
Test
Order serum electrolytes/BUN for any patient with severe pneumonia. Interpret the results in the context of the clinical exam and other laboratory and imaging studies.[1][9]
Result
may be helpful in assessing hydration status in children with reduced fluid intake; hyponatremia is common in children with CAP
acute phase reactants
Test
Acute phase reactants (WBC count, erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], procalcitonin) may be useful in severe CAP when measured serially to monitor response to treatment.[2] Results must be interpreted in the context of the clinical exam and other laboratory and imaging studies.[1] Recommendations on measuring acute phase reactants vary, so check your local protocol.
Acute phase reactants are unreliable for distinguishing bacterial from viral etiology.
In the US, the Pediatric Infectious Diseases Society/Infectious Diseases Society of America (PIDS/IDSA) 2011 guideline: recommends against using ESR, CRP, and serum procalcitonin as the sole means to distinguish viral from bacterial causes of CAP; states that measurement of ESR, CRP, and procalcitonin is not necessary for fully immunized children with suspected CAP managed in the community but may provide useful information for those with more severe disease; recommends to consider using serial results in conjunction with clinical findings to assess response to therapy.[1]
Subsequent findings have suggested that procalcitonin may be useful to identify children with a likely viral etiology, in whom antibiotics are unlikely to be beneficial.[7][40][41][42]
Result
WBC count and ESR are typically elevated, but the degree of elevation does not reliably distinguish bacterial from viral infection; elevated procalcitonin may be a marker of serious bacterial infection, although values vary widely; low procalcitonin (<0.25 nanograms/mL) suggests viral etiology; high procalcitonin in a child with confirmed viral cause raises suspicion of bacterial coinfection; declining levels of CRP and/or procalcitonin on serial measurements suggest positive response to treatment
blood cultures
Test
Only order blood cultures for children who are hospitalized for severe CAP or complicated CAP (ideally before any antibiotics are given).[1][9] Samples are rarely positive; hence, the impact on clinical management is usually small. Nonetheless, culture-directed antimicrobial therapy may be associated with improved clinical outcome in those who do have a pathogen identified.[9]
Microbiologic tests are not needed for nonsevere disease in a fully immunized child.[1][9]
Result
growth of causative bacterial species
polymerase chain reaction (PCR) assays
Test
Rapid diagnostic tests using PCR-based assays can be performed on samples from the nasopharynx, throat, or pleural fluid.[9] This can be particularly useful to avoid inappropriate antibiotic therapy if a viral or atypical bacterial etiology is suspected.[1] Nasopharyngeal secretions are relatively easy to obtain, and the use of PCR testing has been reported to result in pathogen identification in 65% to 83% of cases.[3]
Use of rapid multiplex point-of-care PCR tests for individuals who present with respiratory tract infection has become routine in many hospitals since the COVID-19 pandemic. These enable nasal or nasopharyngeal specimens to be tested simultaneously for multiple pathogens, with results available within 1-2 hours.[36][37] However, one randomized trial involving 1243 children presenting to an emergency department with fever and/or respiratory symptoms or signs failed to show any significant impact on the proportion of children who were prescribed antibiotics.[38]
Rapid diagnostic tests for influenza virus and other respiratory viruses may be useful, if available, in the evaluation of children with CAP in outpatient settings.[1]
Be aware that identification of a viral etiology (e.g., influenza) does not exclude a bacterial pathogen because of the high incidence of coinfection.
Result
detection of viral/atypical pathogen
sputum culture
Test
Used rarely in older children or adolescents who have been hospitalized with severe CAP and can produce a sputum sample for culture and Gram stain.[1] Many younger children cannot produce an adequate specimen.
If the child has a lymphocytic effusion or risk factors for tuberculosis (TB) or lives in an area with high incidence of TB, test for Mycobacterium tuberculosis, using induced sputum if feasible.[2]
Result
growth of causative bacterial pathogen
pleural fluid culture
Test
If pleural fluid is obtained (e.g., because of severe CAP or evidence of pleural effusion), send it for: microscopy and culture (including Gram staining, acid-fast bacilli staining, Mycobacterium tuberculosis testing, antibiotic sensitivity testing); and pneumococcal antigen detection and/or PCR. PCR on pleural fluid is more specific and more sensitive than PCR on blood samples, and pleural fluid testing for pneumococcal antigen has a high positive predictive value for pneumococcal empyema.[1][2][9]
Result
growth of causative bacterial species in case of empyema
endotracheal aspirate culture/PCR testing
Test
If a child requires mechanical ventilation for severe or life-threatening CAP, obtain tracheal aspirates at the time of endotracheal tube placement. Send them for Gram stain and culture and for guided testing for viral pathogens.[1]
For children with influenza virus as the suspected etiology for CAP, rapid PCR testing of endotracheal tube secretions may yield positive results despite negative nasopharyngeal test results.
Result
identification of causative organism
bronchoscopy
Test
Reserve bronchoscopy with bronchoalveolar lavage (BAL) for immunocompetent children with severe CAP whose initial diagnostic test results fail to yield any positive results.[1]
BAL is complex in children, particularly neonates, because of small airways.
Flexible bronchoscopy is well tolerated. However, this investigation is only available in some centers and has a small pathogenic yield in children who are not immunosuppressed.[2]
Result
identification of causative organism
chest ultrasound
Test
If there is suspicion on chest x-ray of a parapneumonic effusion, chest ultrasound is recommended for confirmation.[18] Chest ultrasound may also be appropriate for a child who does not respond to initial outpatient treatment.[18]
Ultrasound is more sensitive than chest radiography to evaluate the pleural space.[2] It can be used to detect small pleural effusions, estimate the size of the effusion, and show any fibrinous septations, and can differentiate pleural effusions from consolidated lung.[2] It can also differentiate empyema from peripheral lung abscess.[2] Doppler ultrasound can detect necrotic changes before they become apparent on CT.[2]
Result
may detect complications of CAP (e.g., pleural effusions, empyema, or early necrotic changes)
chest CT
Test
CT chest with intravenous contrast may be useful in limited circumstances in a small subgroup of children with complicated pneumonia, particularly if necrotizing pneumonia is suspected.[2][18]
In most children with complicated CAP, chest CT does not provide any useful clinical information to guide management or indicate prognosis over and above that gained from ultrasound.[2]
Reserve chest CT with intravenous contrast for diagnostic doubt (e.g., suspicion of malignancy) or for when appropriate treatment does not lead to clinical improvement.[2]
Result
necrotizing pneumonia will show as a rapid transition from a thin-walled fluid-filled compartment to cavitation; lung abscess will show as a thick-walled compartment with the fluid, with or without air
Use of this content is subject to our disclaimer