The usual standard of care for the management of uncomplicated appendicitis in adults continues to be operative.
There is emerging evidence to suggest that a nonoperative, antibiotic-only approach may be feasible in select patient populations, who wish to avoid surgery, and who accept the risk of up to 39% recurrence.[86]de Almeida Leite RM, Seo DJ, Gomez-Eslava B, et al. Nonoperative vs operative management of uncomplicated acute appendicitis: a systematic review and meta-analysis. JAMA Surg. 2022 Sep 1;157(9):828-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9330355
http://www.ncbi.nlm.nih.gov/pubmed/35895073?tool=bestpractice.com
In such cases, it is recommended that the diagnosis of uncomplicated appendicitis be confirmed by imaging, and that patient expectations be managed via a shared decision-making process.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[87]Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018 Sep 25;320(12):1259-65.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233612
http://www.ncbi.nlm.nih.gov/pubmed/30264120?tool=bestpractice.com
[88]Sakran JV, Mylonas KS, Gryparis A, et al. Operation versus antibiotics: the "appendicitis conundrum" continues - a meta-analysis. J Trauma Acute Care Surg. 2017 Jun;82(6):1129-37.
http://www.ncbi.nlm.nih.gov/pubmed/28338596?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
The evidence supporting nonoperative management of appendicitis continues to be conflicting, and further research is warranted.[90]Emile SH, Sakr A, Shalaby M, et al. Efficacy and safety of non-operative management of uncomplicated acute appendicitis compared to appendectomy: an umbrella review of systematic reviews and meta-analyses. World J Surg. 2022 May;46(5):1022-38.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8756749
http://www.ncbi.nlm.nih.gov/pubmed/35024922?tool=bestpractice.com
[91]Herrod PJJ, Kwok AT, Lobo DN. Randomized clinical trials comparing antibiotic therapy with appendicectomy for uncomplicated acute appendicitis: meta-analysis. BJS Open. 2022 Jul 7;6(4):zrac100.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9379374
http://www.ncbi.nlm.nih.gov/pubmed/35971796?tool=bestpractice.com
[92]Talan DA, Di Saverio S. Treatment of acute uncomplicated appendicitis. N Engl J Med. 2021 Sep 16;385(12):1116-23.
http://www.ncbi.nlm.nih.gov/pubmed/34525287?tool=bestpractice.com
[93]Meier J, Stevens A, Bhat A, et al. Outcomes of nonoperative vs operative management of acute appendicitis in older adults in the US. JAMA Surg. 2023 Jun 1;158(6):625-32.
https://jamanetwork.com/journals/jamasurgery/fullarticle/2802834
http://www.ncbi.nlm.nih.gov/pubmed/37017955?tool=bestpractice.com
There is more evidence to support a nonoperative approach in children than in adults.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[87]Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018 Sep 25;320(12):1259-65.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233612
http://www.ncbi.nlm.nih.gov/pubmed/30264120?tool=bestpractice.com
[88]Sakran JV, Mylonas KS, Gryparis A, et al. Operation versus antibiotics: the "appendicitis conundrum" continues - a meta-analysis. J Trauma Acute Care Surg. 2017 Jun;82(6):1129-37.
http://www.ncbi.nlm.nih.gov/pubmed/28338596?tool=bestpractice.com
[94]Georgiou R, Eaton S, Stanton MP, et al. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics. 2017 Mar;139(3):e20163003.
https://publications.aap.org/pediatrics/article-abstract/139/3/e20163003/53676/Efficacy-and-Safety-of-Nonoperative-Treatment-for
http://www.ncbi.nlm.nih.gov/pubmed/28213607?tool=bestpractice.com
[95]Gorter RR, The SML, Gorter-Stam MAW, et al. Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg. 2017 Aug;52(8):1219-27.
http://www.ncbi.nlm.nih.gov/pubmed/28449821?tool=bestpractice.com
[96]Podda M, Cillara N, Di Saverio S, et al. Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017 Oct;15(5):303-14.
http://www.ncbi.nlm.nih.gov/pubmed/28284517?tool=bestpractice.com
[97]Kessler U, Mosbahi S, Walker B, et al. Conservative treatment versus surgery for uncomplicated appendicitis in children: a systematic review and meta-analysis. Arch Dis Child. 2017 Dec;102(12):1118-24.
http://www.ncbi.nlm.nih.gov/pubmed/28818844?tool=bestpractice.com
[98]Harnoss JC, Zelienka I, Probst P, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017 May;265(5):889-900.
http://www.ncbi.nlm.nih.gov/pubmed/27759621?tool=bestpractice.com
[99]Rollins KE, Varadhan KK, Neal KR, et al. Antibiotics versus appendicectomy for the treatment of uncomplicated acute appendicitis: an updated meta-analysis of randomised controlled trials. World J Surg. 2016 Oct;40(10):2305-18.
http://www.ncbi.nlm.nih.gov/pubmed/27199000?tool=bestpractice.com
Pregnant patients with acute appendicitis should be managed with obstetric support.[100]Weston P, Moroz P. Appendicitis in pregnancy: how to manage and whether to deliver. Obstet Gynaecol. 2015 Apr;17(2):105-10.
https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/tog.12188
Uncomplicated presentation
Once the diagnosis of acute appendicitis is made, patients should be given nothing by mouth.
Intravenous fluids should be started.[101]Miller TE, Myles PS. Perioperative fluid therapy for major surgery. Anesthesiology. 2019 May;130(5):825-32.
https://pubs.asahq.org/anesthesiology/article/130/5/825/18881/Perioperative-Fluid-Therapy-for-Major-Surgery
http://www.ncbi.nlm.nih.gov/pubmed/30789364?tool=bestpractice.com
Give patients adequate analgesia.[12]Snyder MJ, Guthrie M, Cagle S. Acute appendicitis: efficient diagnosis and management. Am Fam Physician. 2018 Jul 1;98(1):25-33.
https://www.aafp.org/afp/2018/0701/p25.html
http://www.ncbi.nlm.nih.gov/pubmed/30215950?tool=bestpractice.com
[45]Manterola C, Vial M, Moraga J, et al. Analgesia in patients with acute abdominal pain. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD005660.
https://www.doi.org/10.1002/14651858.CD005660.pub3
http://www.ncbi.nlm.nih.gov/pubmed/21249672?tool=bestpractice.com
Adults
Prompt appendectomy remains the treatment of choice in international guidelines and should be recommended in most cases.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
A single preoperative dose of a broad-spectrum antibiotic such as ceftriaxone or cefotaxime plus metronidazole should be given to patients with uncomplicated appendicitis undergoing appendectomy.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
An alternative is cefotetan plus metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
In patients with a beta-lactam allergy or contraindication to these regimens, ciprofloxacin or levofloxacin plus metronidazole can be used.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Postoperative antibiotics are not indicated.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
Cefotetan is a less desirable option because of the increasing resistance of anaerobic bacteria to this agent and possible decreased efficacy.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
An antibiotic-only approach may be reasonable for select groups with uncomplicated appendicitis (suspected or confirmed on computed tomographic scan), where patients understand the risk of recurrent appendicitis.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[86]de Almeida Leite RM, Seo DJ, Gomez-Eslava B, et al. Nonoperative vs operative management of uncomplicated acute appendicitis: a systematic review and meta-analysis. JAMA Surg. 2022 Sep 1;157(9):828-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9330355
http://www.ncbi.nlm.nih.gov/pubmed/35895073?tool=bestpractice.com
[87]Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018 Sep 25;320(12):1259-65.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233612
http://www.ncbi.nlm.nih.gov/pubmed/30264120?tool=bestpractice.com
[88]Sakran JV, Mylonas KS, Gryparis A, et al. Operation versus antibiotics: the "appendicitis conundrum" continues - a meta-analysis. J Trauma Acute Care Surg. 2017 Jun;82(6):1129-37.
http://www.ncbi.nlm.nih.gov/pubmed/28338596?tool=bestpractice.com
[91]Herrod PJJ, Kwok AT, Lobo DN. Randomized clinical trials comparing antibiotic therapy with appendicectomy for uncomplicated acute appendicitis: meta-analysis. BJS Open. 2022 Jul 7;6(4):zrac100.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9379374
http://www.ncbi.nlm.nih.gov/pubmed/35971796?tool=bestpractice.com
In this scenario, initial antibiotic therapy should be with a broad-spectrum antibiotic regimen such as ceftriaxone, cefotaxime, cefepime, or ceftazidime plus metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Piperacillin/tazobactam is also an option.[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Ciprofloxacin or levofloxacin plus metronidazole may be used if beta-lactams are contraindicated.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
In patients at risk of infection by antimicrobial resistant organisms, antibiotic options include ertapenem, imipenem/cilastatin, meropenem, or aztreonam plus vancomycin and metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
After clinical improvement in 1 to 2 days, antibiotics can be swapped to an oral regimen to complete a total duration of 7 to 10 days. Oral options include ciprofloxacin or levofloxacin plus metronidazole, or amoxicillin/clavulanate (if local rates of Escherichia coli resistance are <10%).[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
An antibiotic-only approach is not recommended if an appendicolith is present since nonoperative management carries a significant failure rate.[2]Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: A Review. JAMA. 2021 Dec 14;326(22):2299-311.
http://www.ncbi.nlm.nih.gov/pubmed/34905026?tool=bestpractice.com
[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[103]CODA Collaborative., Flum DR, Davidson GH, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020 Nov 12;383(20):1907-19.
https://www.doi.org/10.1056/NEJMoa2014320
http://www.ncbi.nlm.nih.gov/pubmed/33017106?tool=bestpractice.com
A conservative antibiotic-only approach should be avoided in pregnant patients.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Systemic fluoroquinolone antibiotics (e.g., ciprofloxacin, levofloxacin) may cause serious, disabling, and potentially long-lasting or irreversible adverse events. This includes, but is not limited to: tendinopathy/tendon rupture; peripheral neuropathy; arthropathy/arthralgia; aortic aneurysm and dissection; heart valve regurgitation; dysglycemia; and central nervous system effects including seizures, depression, psychosis, and suicidal thoughts and behavior.[104]Rusu A, Munteanu AC, Arbănași EM, et al. Overview of side-effects of antibacterial fluoroquinolones: new drugs versus old drugs, a step forward in the safety profile? Pharmaceutics. 2023 Mar 1;15(3):804.
https://www.doi.org/10.3390/pharmaceutics15030804
http://www.ncbi.nlm.nih.gov/pubmed/36986665?tool=bestpractice.com
Prescribing restrictions apply to the use of fluoroquinolones, and these restrictions may vary between countries. In general, fluoroquinolones should be restricted for use in serious, life-threatening bacterial infections only. Some regulatory agencies may also recommend that they must only be used in situations where other antibiotics, that are commonly recommended for the infection, are inappropriate (e.g., resistance, contraindications, treatment failure, and unavailability).
Consult your local guidelines and drug formulary for more information on suitability, contraindications, and precautions.
Children
Guidance from the World Society of Emergency Surgery supports nonoperative management as feasible, safe, and effective as initial treatment unless an appendicolith is present.[2]Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: A Review. JAMA. 2021 Dec 14;326(22):2299-311.
http://www.ncbi.nlm.nih.gov/pubmed/34905026?tool=bestpractice.com
[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
However, in the US the usual standard of care for the management of uncomplicated appendicitis in children continues to be operative.[50]Kumar SS, Collings AT, Lamm R, et al. SAGES guideline for the diagnosis and treatment of appendicitis. Surg Endosc. 2024 Jun;38(6):2974-94.
http://www.ncbi.nlm.nih.gov/pubmed/38740595?tool=bestpractice.com
Parenteral antimicrobials that are active against aerobic Gram-negative and anaerobic bacteria should be initiated as soon as the diagnosis of probable appendicitis has been established. Options include ceftriaxone plus metronidazole, piperacillin/tazobactam, or ciprofloxacin plus metronidazole, all as a single dose at the time of surgery.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Postoperative antibiotics are not indicated in children with uncomplicated acute appendicitis since there is no evidence they decrease the rate of surgical infection.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Appendicectomy should not be delayed for children with uncomplicated acute appendicitis needing surgery beyond 24 hours from admission.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Surgery performed within this time is not associated with increased risk of adverse outcomes such as perforation, complications, or operating time in children who receive timely administration of antibiotics and undergo appendectomy less than 24 hours after diagnosis.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
As for adults, surgery is recommended in children with appendicoliths since the failure rate of nonoperative management increases in these cases.[2]Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: A Review. JAMA. 2021 Dec 14;326(22):2299-311.
http://www.ncbi.nlm.nih.gov/pubmed/34905026?tool=bestpractice.com
[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
However, in children without an appendicolith and with low risk of perforation, an antibiotic-only approach can be considered. In this scenario, initial antibiotic therapy should be with a broad-spectrum antibiotic regimen such as ceftriaxone or cefotaxime plus metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Piperacillin/tazobactam is also an option.[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Ciprofloxacin plus metronidazole may be used if beta-lactams are contraindicated.[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
In patients at risk of infection by antimicrobial resistant organisms, antibiotic options include ertapenem, imipenem/cilastatin, or meropenem.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
After clinical improvement in 1 to 2 days, antibiotics can be swapped to an oral regimen to complete a total duration of 7 to 10 days. Oral options include amoxicillin/clavulanate, or ciprofloxacin plus metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Complicated presentation
Adults
Complications of acute appendicitis occur in 4% to 6% of adults and include gangrene with subsequent perforation or intra-abdominal abscess.[21]Brunicardi FC, Andersen DK, Billiar TR, et al, eds. The appendix. In: Schwartz's principles of surgery. 8th ed. New York, NY: McGraw-Hill; 2005:1119-37.
Initial management includes keeping the patient nothing by mouth and starting intravenous fluids.[101]Miller TE, Myles PS. Perioperative fluid therapy for major surgery. Anesthesiology. 2019 May;130(5):825-32.
https://pubs.asahq.org/anesthesiology/article/130/5/825/18881/Perioperative-Fluid-Therapy-for-Major-Surgery
http://www.ncbi.nlm.nih.gov/pubmed/30789364?tool=bestpractice.com
Give patients adequate analgesia.[12]Snyder MJ, Guthrie M, Cagle S. Acute appendicitis: efficient diagnosis and management. Am Fam Physician. 2018 Jul 1;98(1):25-33.
https://www.aafp.org/afp/2018/0701/p25.html
http://www.ncbi.nlm.nih.gov/pubmed/30215950?tool=bestpractice.com
[45]Manterola C, Vial M, Moraga J, et al. Analgesia in patients with acute abdominal pain. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD005660.
https://www.doi.org/10.1002/14651858.CD005660.pub3
http://www.ncbi.nlm.nih.gov/pubmed/21249672?tool=bestpractice.com
Patients who are in shock should be given a bolus of intravenous fluid to help maintain a stable pulse rate and BP.[105]National Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital. May 2017 [internet publication].
https://www.nice.org.uk/guidance/cg174
See Shock. Pregnant patients with acute appendicitis should be managed with obstetric support.[100]Weston P, Moroz P. Appendicitis in pregnancy: how to manage and whether to deliver. Obstet Gynaecol. 2015 Apr;17(2):105-10.
https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/tog.12188
Intravenous antibiotics (e.g., ceftriaxone, cefotaxime, cefepime, ceftazidime, ciprofloxacin, or levofloxacin plus metronidazole; or piperacillin/tazobactam) should be started immediately and continued until the patient becomes afebrile and the leukocytosis is corrected.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
For more severe infections, patients who are at risk of infection with antimicrobial resistant organisms, or who have healthcare associated infections, antibiotic options include ertapenem, imipenem/cilastatin, meropenem, or aztreonam plus vancomycin and metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Combination antibiotic regimens may also be used based on local sensitivities and protocols.[21]Brunicardi FC, Andersen DK, Billiar TR, et al, eds. The appendix. In: Schwartz's principles of surgery. 8th ed. New York, NY: McGraw-Hill; 2005:1119-37. See your local drug information source for guidance on antibiotic selection for pregnant patients.
In patients with acute peritonitis, appendectomy should be performed without delay.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Patients presenting with right lower quadrant abscess should be managed with intravenous antibiotics and drainage either by interventional radiology (computed tomography-guided drainage) or by operative drainage. If there is clinical improvement and the signs and symptoms are completely resolved, interval appendectomy may be unnecessary.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[106]Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect (Larchmt). 2008 Aug;9(4):481-8.
http://www.ncbi.nlm.nih.gov/pubmed/18687030?tool=bestpractice.com
[107]Deakin DE, Ahmed I. Interval appendicectomy after resolution of adult inflammatory appendix mass - is it necessary? Surgeon. 2007 Feb;5(1):45-50.
http://www.ncbi.nlm.nih.gov/pubmed/17313128?tool=bestpractice.com
[108]Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007 Nov;246(5):741-8.
http://www.ncbi.nlm.nih.gov/pubmed/17968164?tool=bestpractice.com
[109]Rushing A, Bugaev N, Jones C, et al. Management of acute appendicitis in adults: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2019 Jul;87(1):214-24.
https://www.east.org/education-resources/practice-management-guidelines/details/acute-appendicitis-in-adults-management-of
http://www.ncbi.nlm.nih.gov/pubmed/30908453?tool=bestpractice.com
Interval appendectomy is performed if the symptoms do not completely resolve and/or if symptoms recur.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[13]Gorter RR, Eker HH, Gorter-Stam MA, et al. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc. 2016 Nov;30(11):4668-90.
https://www.doi.org/10.1007/s00464-016-5245-7
http://www.ncbi.nlm.nih.gov/pubmed/27660247?tool=bestpractice.com
Interval appendicectomy is also recommended in all patients over 30 years old with complicated appendicitis initially treated nonoperatively; in addition, any patient ages ≥40 years with uncomplicated appendicitis who has conservative management without interval appendicectomy should undergo screening with colonoscopy and interval full-dose contrast-enhanced computed tomography (CT) scan.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[110]Hayes D, Reiter S, Hagen E, et al. Is interval appendectomy really needed? A closer look at neoplasm rates in adult patients undergoing interval appendectomy after complicated appendicitis. Surg Endosc. 2021 Jul;35(7):3855-60.
http://www.ncbi.nlm.nih.gov/pubmed/32676725?tool=bestpractice.com
Interval appendectomy can also be used to identify patients who have underlying appendiceal neoplasm; interval appendectomy may reduce the future risk of appendiceal neoplasm, particularly in the context of complicated appendicitis.[111]Mällinen J, Rautio T, Grönroos J, et al. Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-Year outcomes of the prei-appendicitis acuta randomized clinical trial. JAMA Surg. 2019 Mar 1;154(3):200-7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6439633
http://www.ncbi.nlm.nih.gov/pubmed/30484824?tool=bestpractice.com
[112]Darwazeh G, Cunningham SC, Kowdley GC. A systematic review of perforated appendicitis and phlegmon: interval appendectomy or wait-and-see? Am Surg. 2016 Jan;82(1):11-5.
http://www.ncbi.nlm.nih.gov/pubmed/26802841?tool=bestpractice.com
The risk of appendiceal neoplasm in patients treated with nonoperative management of complicated appendicitis is 11%, increasing to 16% in patients ages 50 years and older and 43% in patients ages over 80 years.[110]Hayes D, Reiter S, Hagen E, et al. Is interval appendectomy really needed? A closer look at neoplasm rates in adult patients undergoing interval appendectomy after complicated appendicitis. Surg Endosc. 2021 Jul;35(7):3855-60.
http://www.ncbi.nlm.nih.gov/pubmed/32676725?tool=bestpractice.com
[113]Peltrini R, Cantoni V, Green R, et al. Risk of appendiceal neoplasm after interval appendectomy for complicated appendicitis: a systematic review and meta-analysis. Surgeon. 2021 Dec;19(6):e549-58.
http://www.ncbi.nlm.nih.gov/pubmed/33640282?tool=bestpractice.com
[114]Skendelas JP, Alemany VS, Au V, et al. Appendiceal adenocarcinoma found by surgery for acute appendicitis is associated with older age. BMC Surg. 2021 May 2;21(1):228.
https://www.doi.org/10.1186/s12893-021-01224-0
http://www.ncbi.nlm.nih.gov/pubmed/33934697?tool=bestpractice.com
Short-term postoperative broad-spectrum antibiotics should be considered for patients who have undergone appendectomy for complicated appendicitis, especially if complete source control has not been achieved.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[50]Kumar SS, Collings AT, Lamm R, et al. SAGES guideline for the diagnosis and treatment of appendicitis. Surg Endosc. 2024 Jun;38(6):2974-94.
http://www.ncbi.nlm.nih.gov/pubmed/38740595?tool=bestpractice.com
Options for oral regimens include amoxicillin/clavulanate, or metronidazole plus levofloxacin or ciprofloxacin.[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
[115]Lipping E, Saar S, Reinsoo A, et al. Short postoperative intravenous versus oral antibacterial therapy in complicated acute appendicitis: a pilot noninferiority randomized trial. Ann Surg. 2024 Feb 1;279(2):191-5.
The optimal management for appendicitis with phlegmon or abscess remains subject to debate.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Latest evidence suggests that laparoscopic appendectomy is associated with fewer readmissions and fewer additional interventions than conservative management, provided advanced laparoscopic expertize is available.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[116]Ahmed A, Feroz SH, Dominic JL, et al. Is emergency appendicectomy better than elective appendicectomy for the treatment of appendiceal phlegmon?: a review. Cureus. 2020 Dec 12;12(12):e12045.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7802400
http://www.ncbi.nlm.nih.gov/pubmed/33447475?tool=bestpractice.com
Nonoperative management with antibiotics and, if available, percutaneous image-guided drainage is a reasonable alternative if the patient is stable and laparoscopic appendectomy is unavailable, although there is a lack of evidence for its use on a routine basis.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[50]Kumar SS, Collings AT, Lamm R, et al. SAGES guideline for the diagnosis and treatment of appendicitis. Surg Endosc. 2024 Jun;38(6):2974-94.
http://www.ncbi.nlm.nih.gov/pubmed/38740595?tool=bestpractice.com
Children
Complications of acute appendicitis occur in less than 19% of children and include gangrene with subsequent perforation or intra-abdominal abscess.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[116]Ahmed A, Feroz SH, Dominic JL, et al. Is emergency appendicectomy better than elective appendicectomy for the treatment of appendiceal phlegmon?: a review. Cureus. 2020 Dec 12;12(12):e12045.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7802400
http://www.ncbi.nlm.nih.gov/pubmed/33447475?tool=bestpractice.com
As with adults, initial management includes keeping the patient nothing by mouth and starting intravenous fluids and intravenous antibiotics. Early appendectomy within 8 hours should be performed in case of complicated appendicitis.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Laparoscopic appendectomy is preferred over open appendectomy in children where laparoscopic equipment and expertize are available.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[117]Kiblawi R, Zoeller C, Zanini A, et al. Laparoscopic versus open pediatric surgery: three decades of comparative studies. Eur J Pediatr Surg. 2022 Feb;32(1):9-25.
http://www.ncbi.nlm.nih.gov/pubmed/34933374?tool=bestpractice.com
[118]Neogi S, Banerjee A, Panda SS, et al. Laparoscopic versus open appendicectomy for complicated appendicitis in children: A systematic review and meta-analysis. J Pediatr Surg. 2022 Mar;57(3):394-405.
http://www.ncbi.nlm.nih.gov/pubmed/34332757?tool=bestpractice.com
Antibiotic options include ceftriaxone or cefotaxime plus metronidazole, or piperacillin/tazobactam. In patients with beta-lactam allergy or other contraindications to the preceding regimens, ciprofloxacin plus metronidazole can be used.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Postoperative antibiotics for less than 7 days seems to be safe and is not associated with an increased risk of complications.[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
These can be switched from intravenous to oral form after 48 hours in children with complicated appendicitis, if there is clinical improvement and white cell count (WCC) has normalized, with an overall length of therapy shorter than 7 days.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
Options for oral regimens include amoxicillin/clavulanate, or ciprofloxacin plus metronidazole.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
[102]Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017 Jan;18(1):1-76.
https://www.liebertpub.com/doi/10.1089/sur.2016.261
http://www.ncbi.nlm.nih.gov/pubmed/28085573?tool=bestpractice.com
As per management of adults with phlegmon or abscess, nonoperative management (antibiotics and, if available, percutaneous image-guided drainage) is a reasonable alternative if the patient is stable and laparoscopic appendectomy is unavailable.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
Nonoperative management has been associated with better results in terms of complication rate and readmission rate in children but evidence does not support its routine use.[119]Fugazzola P, Coccolini F, Tomasoni M, et al. Early appendectomy vs. conservative management in complicated acute appendicitis in children: a meta-analysis. J Pediatr Surg. 2019 Nov;54(11):2234-41.
http://www.ncbi.nlm.nih.gov/pubmed/30857730?tool=bestpractice.com
[120]Vaos G, Dimopoulou A, Gkioka E, et al. Immediate surgery or conservative treatment for complicated acute appendicitis in children? A meta-analysis. J Pediatr Surg. 2019 Jul;54(7):1365-71.
http://www.ncbi.nlm.nih.gov/pubmed/30115448?tool=bestpractice.com
Surgical options
There are two operative options for appendectomy: open and laparoscopic. Most procedures are now undertaken laparoscopically.
In adults, the choice of appendectomy generally depends upon the experience of the surgeon. Studies have shown laparoscopic appendectomy to have better cosmetic results, shorter length of hospital stay, reduced postoperative pain, and reduced risk of wound infection compared with open appendectomy.[121]Jaschinski T, Mosch CG, Eikermann M, et al. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018 Nov 28;(11):CD001546.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001546.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/30484855?tool=bestpractice.com
[122]Zhang G, Wu B. Meta-analysis of the clinical efficacy of laparoscopic appendectomy in the treatment of acute appendicitis. World J Emerg Surg. 2022 May 26;17(1):26.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9137214
http://www.ncbi.nlm.nih.gov/pubmed/35619101?tool=bestpractice.com
[  ]
For adults and adolescents with suspected appendicitis, how does laparoscopic appendectomy compare with conventional appendectomy?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2373/fullShow me the answer[Evidence B]4b1f7fa3-7ac9-4096-8d11-a428fd0c7cc0ccaBFor adults and adolescents with suspected appendicitis, how does laparoscopic appendectomy compare with conventional appendectomy? Laparoscopic appendectomy is recommended for uncomplicated appendicitis, as well as complicated and perforated appendicitis.[123]Wei HB, Huang JL, Zheng ZH, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010 Feb;24(2):266-9.
http://www.ncbi.nlm.nih.gov/pubmed/19517167?tool=bestpractice.com
[124]Yau KK, Siu WT, Tang CN, et al. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007 Jul;205(1):60-5.
http://www.ncbi.nlm.nih.gov/pubmed/17617333?tool=bestpractice.com
It is also considered the safest approach in obese patients.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[125]Woodham BL, Cox MR, Eslick GD. Evidence to support the use of laparoscopic over open appendicectomy for obese individuals: a meta-analysis. Surg Endosc. 2012 Sep;26(9):2566-70.
http://www.ncbi.nlm.nih.gov/pubmed/22437955?tool=bestpractice.com
]
For adults and adolescents with suspected appendicitis, how does laparoscopic appendectomy compare with conventional appendectomy?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2373/fullShow me the answer[Evidence B]4b1f7fa3-7ac9-4096-8d11-a428fd0c7cc0ccaBFor adults and adolescents with suspected appendicitis, how does laparoscopic appendectomy compare with conventional appendectomy? Laparoscopic appendectomy is recommended for uncomplicated appendicitis, as well as complicated and perforated appendicitis.[123]Wei HB, Huang JL, Zheng ZH, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010 Feb;24(2):266-9.
http://www.ncbi.nlm.nih.gov/pubmed/19517167?tool=bestpractice.com
[124]Yau KK, Siu WT, Tang CN, et al. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007 Jul;205(1):60-5.
http://www.ncbi.nlm.nih.gov/pubmed/17617333?tool=bestpractice.com
It is also considered the safest approach in obese patients.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[125]Woodham BL, Cox MR, Eslick GD. Evidence to support the use of laparoscopic over open appendicectomy for obese individuals: a meta-analysis. Surg Endosc. 2012 Sep;26(9):2566-70.
http://www.ncbi.nlm.nih.gov/pubmed/22437955?tool=bestpractice.com
In children, laparoscopic appendectomy decreases the incidence of overall postoperative complications, including wound infection and duration of total hospital stay.[118]Neogi S, Banerjee A, Panda SS, et al. Laparoscopic versus open appendicectomy for complicated appendicitis in children: A systematic review and meta-analysis. J Pediatr Surg. 2022 Mar;57(3):394-405.
http://www.ncbi.nlm.nih.gov/pubmed/34332757?tool=bestpractice.com
[121]Jaschinski T, Mosch CG, Eikermann M, et al. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018 Nov 28;(11):CD001546.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001546.pub4/full
http://www.ncbi.nlm.nih.gov/pubmed/30484855?tool=bestpractice.com
[126]Katkhouda N, Mason RJ, Towfigh S, et al. Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg. 2005 Sep;242(3):439-48; discussion 448-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1357752
http://www.ncbi.nlm.nih.gov/pubmed/16135930?tool=bestpractice.com
[127]Billingham MJ, Basterfield SJ. Pediatric surgical technique: laparoscopic or open approach? A systematic review and meta-analysis. Eur J Pediatr Surg. 2010 Mar;20(2):73-7.
http://www.ncbi.nlm.nih.gov/pubmed/19882502?tool=bestpractice.com
[128]Zhang S, Du T, Jiang X, et al. Laparoscopic appendectomy in children with perforated appendicitis: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2017 Aug;27(4):262-66.
http://www.ncbi.nlm.nih.gov/pubmed/28472016?tool=bestpractice.com
[129]Yu MC, Feng YJ, Wang W, et al. Is laparoscopic appendectomy feasible for complicated appendicitis ?A systematic review and meta-analysis. Int J Surg. 2017 Apr;40:187-97.
https://www.doi.org/10.1016/j.ijsu.2017.03.022
http://www.ncbi.nlm.nih.gov/pubmed/28302449?tool=bestpractice.com
In pregnant patients, laparoscopic appendectomy should be preferred to open appendectomy when surgery is indicated and where expertize of laparoscopy is available.[130]Liew AN, Lim KY, Quach D, et al. Laparoscopic versus open appendicectomy in pregnancy: experience from a single institution and meta-analysis. ANZ J Surg. 2022 May;92(5):1071-8.
http://www.ncbi.nlm.nih.gov/pubmed/35373462?tool=bestpractice.com
[131]Zeng Q, Aierken A, Gu SS, et al. Laparoscopic versus open appendectomy for appendicitis in pregnancy: systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 2021 May 3;31(5):637-44.
http://www.ncbi.nlm.nih.gov/pubmed/33935257?tool=bestpractice.com
It is safe in terms of risk of fetal loss and preterm delivery.[130]Liew AN, Lim KY, Quach D, et al. Laparoscopic versus open appendicectomy in pregnancy: experience from a single institution and meta-analysis. ANZ J Surg. 2022 May;92(5):1071-8.
http://www.ncbi.nlm.nih.gov/pubmed/35373462?tool=bestpractice.com
[131]Zeng Q, Aierken A, Gu SS, et al. Laparoscopic versus open appendectomy for appendicitis in pregnancy: systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 2021 May 3;31(5):637-44.
http://www.ncbi.nlm.nih.gov/pubmed/33935257?tool=bestpractice.com
Compared with open surgery during pregnancy, laparoscopic appendectomy is associated with shorter length of hospital stay and lower incidence of surgical site infection. Laparoscopy is technically safe and feasible during pregnancy.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[130]Liew AN, Lim KY, Quach D, et al. Laparoscopic versus open appendicectomy in pregnancy: experience from a single institution and meta-analysis. ANZ J Surg. 2022 May;92(5):1071-8.
http://www.ncbi.nlm.nih.gov/pubmed/35373462?tool=bestpractice.com
[131]Zeng Q, Aierken A, Gu SS, et al. Laparoscopic versus open appendectomy for appendicitis in pregnancy: systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 2021 May 3;31(5):637-44.
http://www.ncbi.nlm.nih.gov/pubmed/33935257?tool=bestpractice.com
[132]Lee SH, Lee JY, Choi YY, et al. Laparoscopic appendectomy versus open appendectomy for suspected appendicitis during pregnancy: a systematic review and updated meta-analysis. BMC Surg. 2019 Apr 25;19(1):41.
https://www.doi.org/10.1186/s12893-019-0505-9
http://www.ncbi.nlm.nih.gov/pubmed/31023289?tool=bestpractice.com
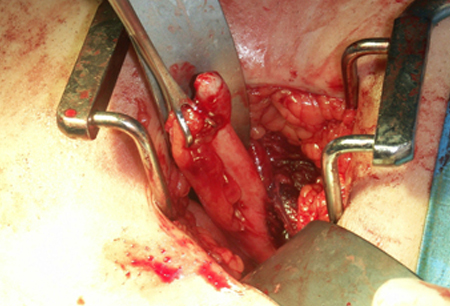
[Figure caption and citation for the preceding image starts]: Acute appendicitis - intraoperative specimen.Nasim Ahmed, MBBS, FACS; used with permission [Citation ends].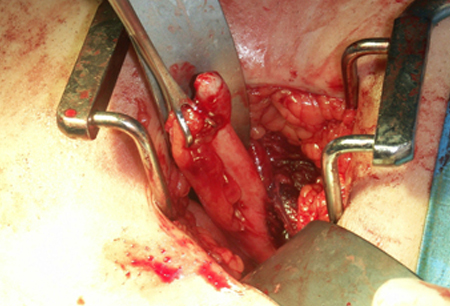
Antibiotic-only therapy
Antibiotics alone for the treatment of uncomplicated appendicitis can be successful in selected patients who wish to avoid surgery, and who accept the risk of up to 39% recurrence.[86]de Almeida Leite RM, Seo DJ, Gomez-Eslava B, et al. Nonoperative vs operative management of uncomplicated acute appendicitis: a systematic review and meta-analysis. JAMA Surg. 2022 Sep 1;157(9):828-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9330355
http://www.ncbi.nlm.nih.gov/pubmed/35895073?tool=bestpractice.com
[91]Herrod PJJ, Kwok AT, Lobo DN. Randomized clinical trials comparing antibiotic therapy with appendicectomy for uncomplicated acute appendicitis: meta-analysis. BJS Open. 2022 Jul 7;6(4):zrac100.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9379374
http://www.ncbi.nlm.nih.gov/pubmed/35971796?tool=bestpractice.com
In such cases, it is recommended that the diagnosis of uncomplicated appendicitis is confirmed by imaging, and that patient expectations are managed via a shared decision-making process.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[87]Salminen P, Tuominen R, Paajanen H, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018 Sep 25;320(12):1259-65.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6233612
http://www.ncbi.nlm.nih.gov/pubmed/30264120?tool=bestpractice.com
[88]Sakran JV, Mylonas KS, Gryparis A, et al. Operation versus antibiotics: the "appendicitis conundrum" continues - a meta-analysis. J Trauma Acute Care Surg. 2017 Jun;82(6):1129-37.
http://www.ncbi.nlm.nih.gov/pubmed/28338596?tool=bestpractice.com
[89]Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5504840
http://www.ncbi.nlm.nih.gov/pubmed/28702076?tool=bestpractice.com
In this scenario, broad-spectrum antibiotics are recommended. The recommended regimens are the same as for uncomplicated presentation (see above).
An antibiotic-only approach is not recommended in pregnant patients or if an appendicolith is present.[2]Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: A Review. JAMA. 2021 Dec 14;326(22):2299-311.
http://www.ncbi.nlm.nih.gov/pubmed/34905026?tool=bestpractice.com
[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
[103]CODA Collaborative., Flum DR, Davidson GH, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020 Nov 12;383(20):1907-19.
https://www.doi.org/10.1056/NEJMoa2014320
http://www.ncbi.nlm.nih.gov/pubmed/33017106?tool=bestpractice.com
Outpatient laparoscopic appendectomy
Some patients may be discharged safely after laparoscopic appendectomy without hospitalization.[134]de Wijkerslooth EML, Bakas JM, van Rosmalen J, et al. Same-day discharge after appendectomy for acute appendicitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2021 Jun;36(6):1297-309.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8119270
http://www.ncbi.nlm.nih.gov/pubmed/33575890?tool=bestpractice.com
This outpatient approach is suitable for patients with uncomplicated appendicitis, provided that an ambulatory pathway with well-defined ERAS (Enhanced Recovery After Surgery) protocols and patient information/consent are locally established.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
ERAS implementation after laparoscopic appendectomy carries similar rates of morbidity and readmissions compared with conventional care.[135]Trejo-Ávila ME, Romero-Loera S, Cárdenas-Lailson E, et al. Enhanced recovery after surgery protocol allows ambulatory laparoscopic appendectomy in uncomplicated acute appendicitis: a prospective, randomized trial. Surg Endosc. 2019 Feb;33(2):429-36.
http://www.ncbi.nlm.nih.gov/pubmed/29987566?tool=bestpractice.com
Its potential benefits include earlier recovery after surgery and lower hospital and social costs.[7]Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386163
http://www.ncbi.nlm.nih.gov/pubmed/32295644?tool=bestpractice.com
 ]
[Evidence B] Laparoscopic appendectomy is recommended for uncomplicated appendicitis, as well as complicated and perforated appendicitis.[123][124] It is also considered the safest approach in obese patients.[7][125]
]
[Evidence B] Laparoscopic appendectomy is recommended for uncomplicated appendicitis, as well as complicated and perforated appendicitis.[123][124] It is also considered the safest approach in obese patients.[7][125]