Complications
Is common, but rarely causes congestive heart failure.
Responds promptly to intravenous immune globulin.
Complete resolution with intravenous immune globulin.
Occurs in 25% of patients who are acutely ill before intravenous immune globulin treatment.
There are diffuse coronary artery ectasia, small aneurysms (internal luminal diameter <5 mm), and giant aneurysms (≥8 mm). Small aneurysms can resolve in up to 2 years. Giant coronary artery aneurysms (CAAs) are associated with significant morbidity and mortality. If the echocardiogram findings are abnormal at any stage in the course of illness, the patient should be referred to a pediatric cardiologist for a complete cardiac workup and follow-up care. The risk of CAAs is the highest in: children with KD who did not receive IVIG within 10 days of fever onset; patients who have persistent fever despite IVIG treatment; patients with laboratory findings suggesting persistent inflammation (increased erythrocyte sedimentation rate, C-reactive protein [CRP], or both); and young children (<6 months old) or older children (>8 years old) and male sex are also among the high risk. [Figure caption and citation for the preceding image starts]: Coronary artery ectasiaBMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1113 [Citation ends].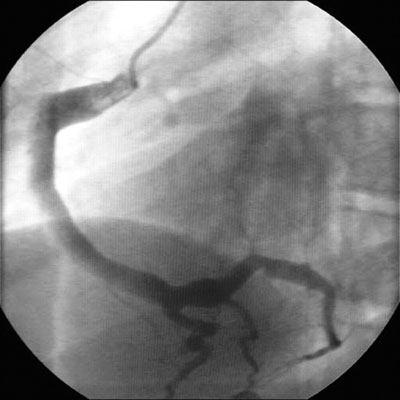
In IVIG-treated patients, the following are also associated with higher risk: higher counts of neutrophils, bands and platelets; anemia; and a fever that does not resolve within the first day of the IVIG treatment.[79][80]
Other treatment failure predictors after IVIG include: increase in CRP, lactate dehydrogenase, and bilirubin levels.[80][81] Some data suggest that sodium levels of <135 mEq/L at initial presentation may predict giant CAA development.[82]
Black ethnicity background may play a protective role for the development of coronary abnormalities.[83]
If CAAs are confirmed, an additional antiplatelet agent (e.g., clopidogrel) should be added and the patient should continue to be monitored by a cardiologist.
Patients with known giant aneurysms during the acute phase of KD are likely to have cardiovascular comorbidities as young adults. These patients should be followed up by a cardiologist. The number of patients with myocardial and vascular complications in adulthood, however, has decreased since the introduction of IVIG treatment.[84]
A study of patients from 1979-2014 in the US found that overall CAA regression rate was approximately 75%, with a low regression rate of 16% in patients with large/giant CAA and a high regression rate of 85% in those with small CAA at diagnosis. Notably, the overall regression rate was higher in the most recent 5-year period (90%). These rates are higher than those previously reported and may be related to better recognition of KD.[85]
Rarely merits valve replacement.
Usually mitral, occurs in only 1% of patients.
Responds promptly to intravenous immune globulin and high-dose aspirin. The American College of Rheumatology/Vasculitis Foundation recommend the use of nonsteroidal anti-inflammatory drugs in patients who are symptomatic following IVIG treatment, though this is not given in combination with aspirin.[37]
In the acute phase. Occurs in 10% to 30% of patients; responds promptly to intravenous immune globulin.
Hydrops (diagnosed by means of ultrasonography) occurs in less than 10% of patients. It usually resolves without surgical intervention.
Responds promptly to intravenous immune globulin.
Rare, but can occur as a manifestation of Kawasaki disease or as a consequence of intravenous immune globulin treatment. Complete spontaneous resolution.
Rare, but potentially fatal inflammatory reaction driven by excessive cytokine production, macrophage activation, and hemophagocytosis. Diagnosis should be considered in patients with suspected KD who have persistent fever, splenomegaly, high ferritin, low platelets, and high aspartate aminotransferase.[88]
Medical or surgical interventions as recommended by the cardiologist.
Treatment of thrombotic coronary occlusion is based upon recommendations for treatment of adults with acute coronary syndromes.
Thrombolytic therapy consists of use of streptokinase, urokinase, or alteplase (tissue plasminogen activator) in combination with aspirin and heparin (unfractionated or low molecular weight). Thrombosis can occur in giant aneurysms despite therapeutic levels of anticoagulation and antiplatelet therapy.[86] Children with ongoing significant stenotic coronary artery aneurysms may develop a network of collateral vessels, resulting in a greater tolerance of thrombotic occlusion in the main vessel. If immediate intervention is not required, there should be an urgent review of antithrombotic therapy and the overall management plan.[86]
Medical or surgical interventions as recommended by the cardiologist.
Acute myocardial infarction is an important cause of morbidity and mortality in Kawasaki disease, and patients with giant aneurysms are at the greatest risk. Risk of myocardial infarction or myocardial ischemia is highest in the first 2 years after diagnosis; patients with giant aneurysms after KD have a; 60% rate of cardiac events over 30 years, with the highest risk in those with bilateral giant coronary aneurysms.[87]
Diagnosis can be difficult in children and adults with previous Kawasaki disease, as they may present with atypical and nonspecific symptoms. This is particularly so for young children, who may present with poorly localized pain, restlessness, unusual pallor, breathlessness, or unexplained crying. Troponin and electrocardiogram may initially be normal, even with extensive ischemia. Urgent imaging is the only way to exclude thrombosis within aneurysms in children with chest pain or who are unwell. Unless the cause of illness is clearly noncardiac in origin (e.g., epilepsy, trauma, bacterial infection, acute abdomen, acute gastroenteritis), all patients should be seen in a specialized cardiac center for evaluation.[12]
All patients should have a clear management plan for antithrombotic treatment with tissue plasminogen activator or streptokinase.
In some settings, percutaneous coronary intervention is an option, depending on transport time to an interventional cardiology center, the patient's size if they are a child, and the technical challenges of instrumentation in vessels previously damaged by Kawasaki disease.[12]
Extremely rare and can be associated with hemopericardium. Most complications relate to healing with stenosis or persistence of giant coronary artery aneurysms.
Medical or surgical interventions as recommended by the cardiologist.
Rare, but can occur in the following arteries: femoral, subclavian, iliac, brachial, axillary, and others. Surgical intervention may be needed.
Vascular surgeon needs to be consulted.
Pediatric general surgeon needs to be consulted.
Use of this content is subject to our disclaimer