Approach
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Richtlijn acute rinosinusitisPublished by: Werkgroep Ontwikkeling Richtlijnen Eerste Lijn (Worel)Last published: 2023Guide de pratique clinique rhinosinusite aiguëPublished by: Groupe de travail Développement de recommandations de première ligneLast published: 2023Diagnosis is primarily based on the history and physical examination. There is usually no need for further investigations unless there are complications present. In most cases the diagnosis is made presumptively. Complications, although rare, are more common in children.
History
Key risk factors include allergic rhinitis or a recent history of viral upper respiratory tract infection. Asthma may be exacerbated by acute rhinosinusitis.
Important factors in differentiating viral from bacterial rhinosinusitis are the overall symptom duration and the symptom trajectory. Symptoms of viral infection tend to peak early and gradually resolve.[1][4][17] Thus symptoms present for less than 10 days indicate a viral infection, whereas symptoms present for more than 10 days, without an improvement, suggest a bacterial infection.[1][3] Symptoms that worsen after an initial improvement (so-called 'double sickening') suggest secondary bacterial infection following viral rhinosinusitis.[1]
Cough is a common symptom in acute viral and bacterial rhinosinusitis.[4] Cough may occur secondary to post-nasal drainage or asthma exacerbation. Other symptoms may include sore throat, hyposmia, purulent nasal discharge, and fever.
Physical examination
Examination should include a thorough head and neck examination, with particular attention paid to the presence of:
Facial tenderness to gentle palpation
Post-nasal pharyngeal secretions or exudate
Tender maxillary dentition
Middle ear effusion.
The nasal cavity should be examined for the presence of mucosal erythema or purulent discharge. Optimal examination is performed after topical decongestant spray.[18] Either an otoscope or a nasal speculum and head light may be used. However, because nasal examination may be difficult or the signs non-specific, nasal endoscopy is recommended in selected patients, including patients refractory to empirical antibiotic therapy or where there is concern for antibiotic resistance, or in immunocompromised patients.
Endoscopy can provide excellent visualisation of the nasal cavity and sinus drainage paths. There are two types of endoscope: rigid and flexible. A rigid nasal endoscope has superior resolution and only requires the use of one hand. This easily allows cultures of the nasal cavity or sinus to be obtained if necessary. A flexible nasal endoscope is more comfortable for patients, but requires both hands to use. There are flexible nasal endoscopes that have a channel for collecting cultures, but these tend to be larger and more uncomfortable and they are also more difficult to re-process. Generally, the flexible nasal endoscope is preferred in children as it is better tolerated; however, either type may be used in adults and children. Choice will depend on the practitioner's familiarity with the procedure, and most will be performed by an ear, nose, and throat specialist.
Peri-orbital or malar oedema, orbital proptosis, visual disturbances, abnormal extra-ocular movements, or abnormal neurological signs may indicate the presence of complications, and urgent otolaryngology consultation is required.[Figure caption and citation for the preceding image starts]: Right inferior turbinate and septum are visible prior to decongestant sprayFrom the collection of Melissa Pynnonen, MD [Citation ends].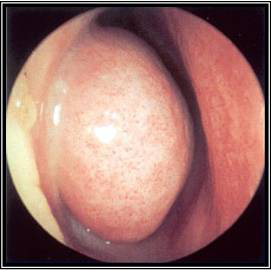 [Figure caption and citation for the preceding image starts]: Right middle turbinate and middle meatus are visible after decongestant sprayFrom the collection of Melissa Pynnonen, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Right middle turbinate and middle meatus are visible after decongestant sprayFrom the collection of Melissa Pynnonen, MD [Citation ends].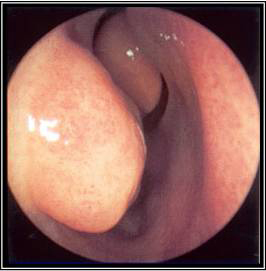 [Figure caption and citation for the preceding image starts]: Left middle meatus with severe oedema and purulent secretionsFrom the collection of Melissa Pynnonen, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Left middle meatus with severe oedema and purulent secretionsFrom the collection of Melissa Pynnonen, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Left middle meatus with healthy mucosa and non-purulent secretionsFrom the collection of Melissa Pynnonen, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Left middle meatus with healthy mucosa and non-purulent secretionsFrom the collection of Melissa Pynnonen, MD [Citation ends].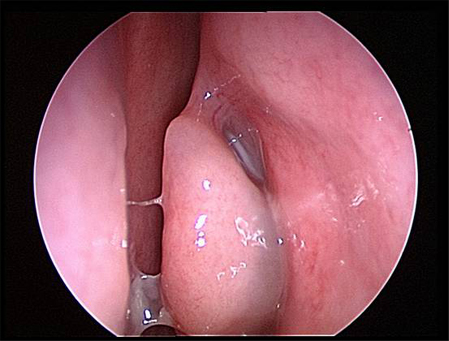 [Figure caption and citation for the preceding image starts]: Nasal endoscopy of the left nasal cavity showing a small polyp and pus in the middle meatusFrom the collection of Joseph K. Han [Citation ends].
[Figure caption and citation for the preceding image starts]: Nasal endoscopy of the left nasal cavity showing a small polyp and pus in the middle meatusFrom the collection of Joseph K. Han [Citation ends].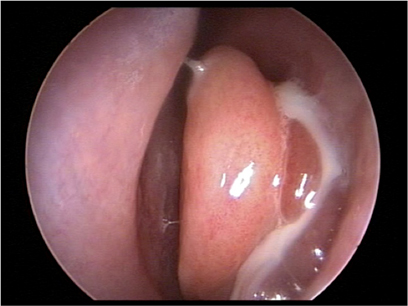
Investigations
Laboratory testing is of limited value in the diagnosis of acute rhinosinusitis.[19] However, culture can be an important aid in antibiotic selection if:
The infection has been refractory to empirical antibiotic therapy
There is a concern for antibiotic resistance
The patient is immunocompromised.
The Infectious Diseases Society of America (IDSA)/American Society for Microbiology (ASM) guidelines recommend that the ideal specimens for uncomplicated acute rhinosinusitis are aspirate obtained by antral puncture or a middle meatal swab specimen obtained with endoscopic guidance.[20] Endoscopic sinus culture is much less painful than sinus puncture. The two culture methods correlate well, especially when there is purulence within the middle meatus (i.e., within the sinus drainage path).[21][22] Cultures taken from the nasal cavity or the nasopharynx, such as with a swab and without endoscopic visualisation, are discouraged because they do not correlate with the causative pathogen.[20]
For complicated rhinosinusitis, aspirate obtained by antral puncture or tissue or aspirate obtained surgically can be used for bacterial or fungal culture.[20]
Skin or blood allergy testing (specific IgE) may be considered to rule out allergic rhinitis, particularly if there is no response to antibiotic therapy or for recurrent episodes.[1]
Imaging
Radiographic studies are not recommended for routine evaluation of acute rhinosinusitis because they have not been shown to change clinical outcomes.[23][24] They cannot differentiate viral from bacterial rhinosinusitis.[15][24] Imaging may expose patients to radiation and intravenous contrast unnecessarily.[23]
Radiographic studies are recommended in certain patients, including those with complications of rhinosinusitis, such as facial cellulitis, suspected orbital infection, or intracranial infection, and those with rapidly progressing disease or suspected acute invasive fungal rhinosinusitis.[24] Radiographic studies are also recommended in the evaluation of patients with suspected recurrent acute or chronic rhinosinusitis.[24] In this setting the study may be used to confirm the diagnosis of rhinosinusitis or rule out an alternative diagnosis.[1] For further details, see Chronic rhinosinusitis without nasal polyps.
Computed tomography (CT) scan
CT scan with contrast is the imaging study of choice for acute rhinosinusitis with suspected complications.[1][24]
Findings consistent with, but not diagnostic of, acute rhinosinusitis include sinus opacification, air-fluid level, or marked or severe mucosal thickening.[1][24]
CT without contrast may be appropriate if invasive fungal rhinosinusitis is suspected or for bony evaluation and surgical planning, but it is not as useful as a contrast CT for detecting orbital and intracranial complications.[24]
[Figure caption and citation for the preceding image starts]: Computed tomography scan with right ethmoid sinus opacification and adjacent orbital abscessFrom the collection of Melissa Pynnonen, MD [Citation ends].

Magnetic resonance imaging (MRI)
MRI with and without intravenous contrast may be useful if extra-sinus complications are suspected.[1][24]
MRI orbits, face, and neck without and with IV contrast can confirm paranasal sinus inflammation and identify orbital and adjacent intracranial complications.[24]
X-rays
X-rays of the sinus are not appropriate for the evaluation of rhinosinusitis with complications due to limitations in imaging of soft tissues. CT is preferred if imaging is required.[24]
Lateral neck x-rays can be helpful in children to evaluate the patient for adenoid hypertrophy in patients with nasal obstruction.[15] An alternative is flexible nasal endoscopy, which can confirm adenoiditis.
Use of this content is subject to our disclaimer