History and exam
Key diagnostic factors
common
history of mosquito bites
Mosquito bite exposure within 15 days of disease onset in an endemic area (either travel to or residence in) is the key determinant to acquire the disease. People with a higher degree of outdoor exposure (laborers or travelers) are at increased risk. Socioeconomic conditions can also predispose to higher risk, such as living in an area without mosquito nets or without air conditioning, or residing in a household with intradomiciliary or peridomiciliary conditions that favor the breeding of mosquitoes (water containers, accumulation of garbage).[25]
fever
arthralgias/arthritis
Peripheral arthralgia and/or arthritis has been reported in 90% of patients.[64]
Although monoarticular involvement has been described, the disease usually affects multiple joints and most commonly the distal joints, including wrists, ankles, and both hands and feet. The disease is usually symmetric. The affected joints might just be painful or may have prominent signs of inflammation, including swelling, warmth, and rubor. The joint involvement usually occurs in association with fever, but lasts longer (on average 1-3 weeks). Although arthralgias and myalgias can occur with other arboviral infections, the intensity and frequency of those symptoms is worse in chikungunya and may help in the differential diagnosis.[65]
In chronic cases, the disease can manifest as intermittent or persistent bouts of monoarthritis or polyarthritis. In some cases, the American College of Rheumatology criteria for rheumatoid arthritis are fulfilled by patients chronically affected by infection, including presence of erosive changes in the joints and positive rheumatoid factor. Occasionally, the disease may resemble a seronegative spondyloarthropathy with enthesitis (inflammation where tendons/ligaments insert into bone), and dorsolumbar pain.[4][49][50][51][52][Figure caption and citation for the preceding image starts]: Acute polyarthritis with sausage digits during acute phase, and after resolutionFrom the collection of Dr Fabrice Simon; used with permission [Citation ends].
rash and other dermatological manifestations
In about half of the cases, a maculopapular rash is described, usually associated with the onset of fever, but sometimes occurring after defervescence. The rash is of global distribution but most commonly affects the extremities, and is only occasionally pruritic.
Hyperpigmentation of the skin, predominantly on the face, and enhancement of the discoloration of pre-existing lesions is common.
Intertrigo, perigenital, and perianal well-demarcated ulcers, desquamation of the skin, especially of palms and soles, and oral aphthous ulcers are also frequent.
Vesiculobullous lesions, purpuric lesions, target-like lesions, and erythema nodosum are uncommon.
The morbiliform rash, hyperpigmentation, and intertriginous lesions may also manifest in the chronic phase of the infection.[49][50][Figure caption and citation for the preceding image starts]: Diffuse morbiliform rash during the acute phase of diseaseFrom the collection of Dr Fabrice Simon; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Diffuse hyperemia or erythroderma during the acute phase of the diseaseFrom the collection of Dr Fabrice Simon; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Diffuse hyperemia or erythroderma during the acute phase of the diseaseFrom the collection of Dr Fabrice Simon; used with permission [Citation ends].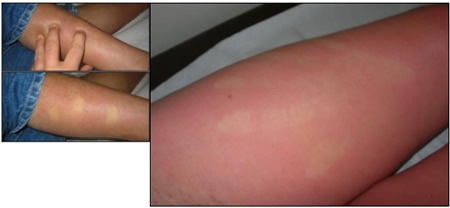
Other diagnostic factors
common
comorbid illness
Patients with chronic medical conditions such as diabetes mellitus or chronic organ failure tend to have worse outcomes. Lethal cases have been reported. This is likely related to impaired immunity.[50]
back pain
neuropathic-type pain
Some patients (18.9%) may present with neuropathic-type pain due to lesions in, or dysfunction of, the nervous system.[48]
headache
lymphadenopathy
ocular manifestations
The most common ocular symptoms are photophobia and retro-ocular pain. The most common sign is conjunctival inflammation during the febrile illness. Hypopyon and corneal precipitates from acute uveitis are occasionally seen. Posterior uveitis and optic neuritis are rare.[67]
uncommon
photophobia
sore throat
gastrointestinal manifestations
neurologic manifestations
Headache and abnormal mental status associated with meningitis or meningoencephalitis are uncommon. Acute flaccid paralysis, acute demyelinating encephalomyelitis, Guillain-Barre syndrome, and sensorineural hearing loss are very rare.[66]
hemorrhagic manifestations
Very rarely causes hemorrhagic manifestations. Gingivorrhagia, epistaxis, hematemesis, and melena were described in an outbreak, preceding the current epidemics.[68]
Risk factors
strong
Aedes mosquito bites
Several species of Aedes mosquitoes can transmit the virus; however, Aedesaegypti and Aedesalbopictus are the most common vectors. These mosquitoes can be identified by their striped appearance and their standing position with a straight body.
A aegypti was the main vector before 2005. Since then, A albopictus (also known as the Asian tiger mosquito) has become the most common vector. This is likely because of a single change in the envelope protein gene E1-A226V, which allowed the virus to adapt to A albopictus, a mosquito with a wider global distribution, including areas in Europe and the US.[24]
A aegypti is distributed in the southeast US and in a few spots in states bordering Mexico. This mosquito is commonly found indoors with larvae breeding in containers inside households. A albopictus also has a predominant distribution in the southeast US, but the range is more ample, extending to Illinois, New York, and Pennsylvania. This mosquito is found predominantly outdoors. Both A aegypti and A albopictus are aggressive biters that attack during the daytime with a peak at dusk.[25]
travel to/residence in endemic area
Although locally transmitted cases have been reported in the US and Europe, it is still expected that the bulk of cases in industrialized countries will be from returning travelers. A travel history to, or residence in, an endemic area within the 15 days prior to onset of infection should prompt suspicion. Housing and sanitary conditions outside developed countries may favor exposure to mosquito bites.[31][32]
outdoor exposure
The longer time spent outdoors, the higher the likelihood of being exposed to mosquito bites. In a study of more than 500 people in an endemic area, spending 8 or more hours outdoors increased the risk of both asymptomatic and symptomatic infection with chikungunya virus.[33]
environmental factors favoring breeding of mosquitoes
neonate with infected mother
Vertical transmission seems to occur predominantly in the third trimester and, particularly, close to delivery. The rate of vertical transmission was as high as 49% in pregnant females infected after week 38 during the Réunion Island outbreak. Infected neonates may have severe disease, predominantly encephalopathy; although most affected neonates have mild disease or no symptoms.[35]
weak
low educational level
Low educational level is a marker of poor socioeconomic condition. People with low educational levels are more likely to have jobs that require longer outdoor exposure. Their living conditions may also favor proliferation of mosquitoes in or near their households. They are also less likely to have mosquito nets or air conditioning.[33]
age >40 years
Some studies suggest that people older than 40 or 50 years of age may have higher risk of developing more severe disease or complications, presumably because of associated comorbidities.[36]
male sex
Studies suggest that men may have higher risk of infection, presumably because of the higher likelihood of outdoor exposure.[37]
blood transfusion
Viremic patients carry a risk for transmission if their blood is donated for transfusion. So far, this seems to be a theoretical risk and no cases have been reported yet.[26]
blood group O positive
A single study among 100 families showed that people with blood type O positive are more susceptible to infection with the virus. The reasons for this association are unclear.[38]
comorbid illnesses (risk of more severe disease)
Comorbid illnesses do not predispose people to infection; however, those affected tend to develop more severe clinical presentation.[39]
neonate (risk of more severe disease)
Being a neonate does not predispose to infection; however, those affected tend to develop a more severe clinical presentation.[35]
Use of this content is subject to our disclaimer