Case history
Case history #1
A 55-year-old woman presents with a left-leg deep vein thrombosis 2 days after being discharged from the hospital. She had been admitted with acute coronary syndrome and was treated with intravenous heparin for 6 days. Her platelet count has declined from 250 × 10⁹/L at the start of her treatment with heparin to 80 × 10⁹/L. Her physical exam is unremarkable except for left-leg edema and tenderness.
Case history #2
A 65-year-old woman is admitted to a rehabilitation floor 10 days after undergoing elective right total hip arthroplasty. She received low molecular weight heparin (LMWH) for thromboprophylaxis beginning on postoperative day 1, but intravenous heparin was subsequently started on postoperative day 9 for confirmed pulmonary embolism. Her platelet count was 175 × 10⁹/L on admission to the rehabilitation floor compared with 350 × 10⁹/L when intravenous heparin was initiated. Her physical exam is unremarkable except for normal postoperative changes. A venous Doppler ultrasound of her leg is negative for deep vein thrombosis.
Other presentations
HIT less commonly presents as adrenal hemorrhagic necrosis (secondary to adrenal vein thrombosis), necrotizing skin lesions at heparin injection sites, cerebral venous thrombosis, or as an acute systemic reaction 30 minutes following an intravenous bolus of unfractionated heparin or subcutaneous LMWH (e.g., fever, chills, tachycardia, hypertension, dyspnea, cardiopulmonary arrest).[6] Rarely, patients with HIT-provoked deep vein thrombosis will present with venous limb gangrene (as a consequence of inappropriate treatment with a vitamin K antagonist).[7][Figure caption and citation for the preceding image starts]: Venous limb gangrene of left foot in HIT: (A) dorsal aspect; (B) medial aspect; and (C) plantar aspectRozati H, Shah SP, Peng YY. Lower limb gangrene postcardiac surgery. BMJ Case Reports. 2013; doi:10.1136/bcr-2012-008362 [Citation ends].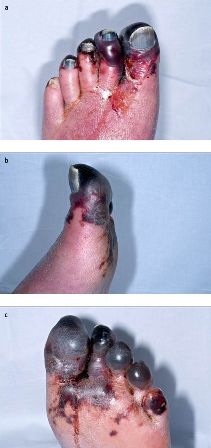
Use of this content is subject to our disclaimer