Approach
Many causes of vaginal bleeding can be diagnosed clinically with history and examination. Further investigation is often with pelvic ultrasound or colposcopy.
Exclude urethral or rectal bleeding as a source of bleeding.
History
Evaluation of vaginal bleeding should include a detailed history of the nature and extent of bleeding. This should include the frequency, volume, and duration of bleeding, and any precipitating factors. The history should be adapted to the patient’s age, because this determines the likely differential diagnoses.
Premenarchal patients
Enquire about the presence of pubic and axillary hair, breast development, and increased growth velocity. If present, these might indicate precocious puberty; puberty in girls <8 years is considered precocious.[53]
Elicit any history of trauma. The majority of injuries are straddle injuries, for example after a fall onto a bicycle crossbar, chair arm, or ladder rung.[54]
Enquire whether a foreign body could have been inserted into the vagina, although children may not divulge this information or may be too young to communicate it. Wads of toilet paper are the most common foreign body identified but pen tops, cotton tipped swabs, safety pins, and small toys have also been reported.[13]
Pruritus, discharge, pain, discomfort, and/or dysuria may indicate vulvovaginitis.[55] Although a common pediatric gynecologic problem, vulvovaginitis rarely causes bleeding, unless there is severe inflammation or excoriation.
The possibility of sexual abuse must be considered in any patient with prepubertal vaginal bleeding. Sexualized behavior, depressive symptoms, aggression, sleep disturbance, regression, and frequent or persistent genitourinary complaints may indicate sexual abuse, although they are nonspecific and the strength of association with child abuse is not quantified. Children may present with somatic complaints such as headaches or recurrent abdominal pain.[48][49] The child should be interviewed alone if possible and asked open ended questions in a neutral voice.[52]
Passage of tissue fragments or presence of a mass at the vaginal opening could indicate rhabdomyosarcoma.[13]
Patients of reproductive age
The initial part of the history should be directed towards establishing whether the patient could be pregnant. Check details of the last menstrual period, contraceptive use, and sexual activity. If the patient might be pregnant, this should be confirmed with a urine pregnancy test as soon as possible. Pregnancy alters the differential diagnosis and the focus of the assessment.
Initial questions should explore the details of the bleeding and any associated symptoms. Questions may include:
Duration of bleeding symptoms
Frequency of bleeding episodes
Volume of bleeding and duration of each episode
Relationship of bleeding to intercourse and menstruation
Associated symptoms may include:
Dyspareunia: may be present in cervical cancer or cervicitis
Pelvic pain: may be present in cervical cancer
Vaginal discharge: may indicate cervicitis, cervical cancer, vaginitis
Dysuria: may indicate sexually transmitted infection causing cervicitis
Lower back pain: can occur in invasive cervical cancer
Pruritus can occur in vaginitis
A medical, sexual, and drug history should be obtained.
The medical history should clarify:
Dates of previous smear tests and any abnormalities
Previous HPV infection (risk factor for cervical and vaginal cancer)
Immunosuppression (risk factor for cervical cancer)
Any history of cancer (possibility of vaginal metastases)
A brief sexual history is useful to establish the patient’s risk of a sexually transmitted infection (STI), which could cause cervicitis. This should include:[56]
Date of last sexual contact and number of partners in preceding 3 months
Sex of partners, anatomic sites of exposure, and condom use
Any suspected infection, infection risk, or symptoms in partners
Any previous STIs
Ask about contraceptive use and, among perimenopausal women, irregular menstrual bleeding and initiation of hormone replacement therapy:
Contraception: hormonal contraception can cause irregular vaginal bleeding and also increases the likelihood of cervical ectropion
Hormone replacement therapy: vaginal bleeding is common in the first 4 to 6 months of using estrogen and progesterone hormone replacement therapy.
Pregnant patients
In addition to considerations relating to women of reproductive age, the clinician should ask about:
the date of the last menstrual period and gestation of the pregnancy
whether the location of the pregnancy is known
any previous pregnancies, their outcomes, and any complications
presence of fetal movements (second and third trimester)
any trauma to the abdomen (including intimate partner violence)
whether the bleeding is associated with pain
any symptoms suggestive of hypovolemia or hemoperitoneum, e.g., dizziness or shoulder pain. Bleeding from the fallopian tube may irritate the diaphragm leading to referred shoulder pain.
Postmenopausal patients
Clarify the date of the last menstrual period. Menopause is diagnosed retrospectively when 12 months have elapsed since the woman’s last menstrual period. Irregular menstrual bleeding is common in the perimenopause and may occur in the first 4 to 6 months of hormone replacement therapy use.
It is appropriate to ask the same questions as for women of reproductive age (see above).
Risk of cancer is higher in this age group. The clinician should enquire about risk factors for gynecologic malignancy, including:
obesity, unopposed endogenous or exogenous estrogen exposure, tamoxifen use, history of endometrial intraepithelial hyperplasia, history of polycystic ovary syndrome (risk factors for endometrial cancer)
Any known BRCA gene mutations
Family history of breast or gynecologic cancer.
Physical exam
Examination should include inspecting the vulva, perineum, and anal area for nonvaginal causes of bleeding such as vulval lesions or anal fissures.
Vital signs should be checked if there is concern about hemodynamic instability, e.g., heavy bleeding or suspected ectopic pregnancy.
All women with abnormal vaginal bleeding should undergo appropriate components of the pelvic examination to identify benign or malignant disease.[57]
Possible findings on bimanual examination are:[58]
Cervical motion tenderness: may indicate ectopic pregnancy or cervicitis
Adnexal tenderness: may indicate ectopic pregnancy
Adnexal mass: may indicate ectopic pregnancy or ovarian cancer
Uterine mass in endometrial cancer
If pelvic examination suggests malignancy, examine the right upper quadrant and the lymph nodes in the groin and supraclavicular regions.[59] If placenta previa is suspected, do not perform digital vaginal examination until ultrasound has excluded this condition.[29][60]
Speculum exam may reveal structural cervical or vaginal lesions as the source of bleeding, such as cervical cancer, cervical polyps, or cervical ectropion.[Figure caption and citation for the preceding image starts]: Cervical erosionScience Photo Library; used with permission [Citation ends].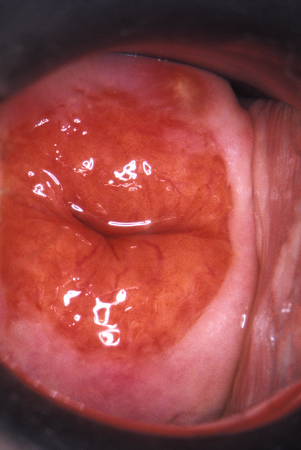 [Figure caption and citation for the preceding image starts]: Cervical polypScience Photo Library; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Cervical polypScience Photo Library; used with permission [Citation ends].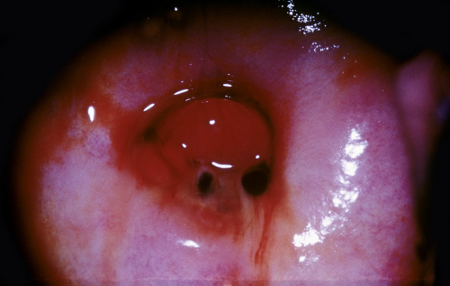
In patients with cervicitis, inflammatory exudate may be visible at the os. The cervix may bleed easily on contact. Punctate cervical hemorrhages ("strawberry cervix") are highly associated with T vaginalis infection.[61] The vagina is typically erythematous and tender.
Genital warts (condylomata acuminata) may be visible as verrucous fleshy papules. The papules may coalesce into plaques. Lesion size ranges from a few millimeters to several centimeters. The warts may be located anywhere in the anogenital or genital area, including on mucosal surfaces. The color can vary from whitish to flesh-colored, to hyperpigmented to erythematous.[24]
The vaginal mucosa appears thin and friable in atrophic vaginitis.[62] It may be erythematous or pale and shiny. Vulvar erythema or edema can accompany candidal vaginitis.
If a woman is in the second or third trimester of pregnancy, palpate the uterus per abdomen and attempt to auscultate the fetal heart. Uterine tenderness may occur in placental abruption, and the uterus may feel hard on palpation.[63]
Internal examination is rarely performed in prepubertal girls. It is usually appropriate to refer children to a pediatric gynecologist for examination. Many patients need to be sedated or anesthetized to enable an adequate physical exam.
Examination is normal or nonspecific in most children who have been sexually abused.[50][51] If sexual abuse is suspected, follow local protocols for reporting suspected sexual abuse. In many countries specific sexual assault centers have been developed, with specially trained staff and facilities.
Laboratory evaluation
Urine or serum human chorionic gonadotropin (hCG) should be performed if there is a possibility of pregnancy.
Complete blood count should be performed to detect anemia in pregnant women with heavy vaginal bleeding. Consideration should be given to the need for Rho(D) immune globulin prophylaxis. Maternal rhesus blood group should be checked, if not already known. The Kleihauer-Betke test determines the size and presence of feto-maternal hemorrhage.
Serum luteinizing hormone, follicle-stimulating hormone, estrogen, and androgen panel should be measured in cases of suspected precocious puberty.
Women with cervicitis or vaginitis should be offered testing for sexually transmitted infections.[15] This should include nucleic acid amplification tests for Chlamydia trachomatis and Neisseria gonorrhoeae, rapid tests for Trichomonas, wet-mount examination and Gram stain of cervical discharge, plasma Venereal Disease Research Laboratory (VDRL) or rapid plasma reagin (RPR) testing to screen for syphilis, and screening for HIV, hepatitis B, and hepatitis C. Vaginal pH testing is useful to distinguish between bacterial vaginosis (pH >4.5) and candidal vaginitis (pH ≤4.5).
Colposcopy
Colposcopic exam provides a magnified view of the cervix and the tissues of the vagina and vulva. Premalignant and malignant lesions with specific characteristics visible on colposcopy can therefore be detected in these areas (e.g., abnormal vascularity, white change with acetic acid, and exophytic lesions are key diagnostic criteria for cervical cancer).
Colposcopy permits the clinician to take biopsies for histologic examination. Women who present with persistent or recurrent episodes of postcoital bleeding should be referred to a gynecologist for colposcopy.
Imaging
Transvaginal and transabdominal pelvic ultrasound are the first-line investigations for most women who require imaging.[29][64][65] It is indicated for suspected miscarriage, ectopic pregnancy, placental abruption, placenta previa, ovarian cancer, endometrial cancer, and precocious puberty.
In women with postmenopausal bleeding, an endometrial thickness of 4 mm or less has a greater than 99% negative predictive value to exclude endometrial cancer.[66]
If cervical or ovarian cancer is suspected, CT pelvis and abdomen can assess for advanced disease.
MRI can assess the extent of myometrial invasion in patients with placenta previa and endometrial cancer.[35]
Biopsy
Endometrial biopsy is done to diagnose endometrial intraepithelial neoplasia and endometrial cancer.[67] The majority of postmenopausal women who present with vaginal bleeding will have an endometrial biopsy, particularly when ultrasound suggests thickened endometrium, risk factors for neoplasia are present, and/or bleeding is recurrent in absence of a history of hormonal therapy.
Cervical biopsy should be carried out if cervical cancer is suspected.
In ovarian cancer, biopsy elevates the risk of cancer cell spillage, so surgical extirpation of the affected ovary or paracentesis or thoracentesis of peritoneal/pleural fluid is usually necessary.[68]
Use of this content is subject to our disclaimer