Approach
The approach used for the diagnosis of a lipoma will depend on its location and characteristics. Superficial cutaneous lipomas can often be diagnosed on history and physical examination alone. There are many subtypes of lipomas, and they are still considered benign. With lesions in other locations, imaging tests and biopsy may be required. Careful consideration of the differential diagnoses is important, particularly the possibility of liposarcoma.
History
History-taking is guided by the anatomical location of the lesion. Questions should explore factors such as:
When the lump was first noticed
What brought the lump to the attention of the patient
The symptoms that are related to the lump
Changes that have occurred to the lump since it first appeared
Whether the lump ever disappears and what causes it to reappear
Whether the patient ever had any other lumps and what they were like
Whether there has been any loss of body weight
Whether the lump has been treated before and has recurred.
Some lesions may be noted only incidentally on imaging studies. In these circumstances, history-taking is adjusted to explore the most likely effects, based on anatomical location of the lesion.
The lipomatous tissue in Dercum's disease can be very severe, debilitating, and progressive. The diagnostic criteria for Dercum's disease are generalised overweight or obesity and chronic pain (>3 months) in the adipose tissue.[12]
If a patient fulfils the criteria and has isolated painful lipomas, the diagnosis is nodular Dercum's disease. Pain differentiates patients with Dercum's disease from patients with lipomatosis, who do not have extreme chronic pain. Dercum's disease is a syndrome consisting of four symptoms: multiple, painful fatty masses; generalised obesity; weakness and fatigue; psychiatric disturbances such as depression, confusion, and dementia. The pain can last for hours and be intermittent or constant, and may worsen with movement. It can be associated with congestive heart failure, myxoedema, paroxysmal flushing, hypertension, headaches, and epistaxis.
Physical examination
Physical examination of an accessible lesion should include all the classic elements: look, feel, measure, press, percuss, move, listen, trans-illuminate, and examine surrounding tissue.
Most superficial cutaneous lipomas on the extremities or trunk are <5 cm in size and present as painless, rounded, mobile masses, which have a characteristic soft, doughy feel.[Figure caption and citation for the preceding image starts]: Subcutaneous lipoma on the trunkFrom the collection of Dr Kimberly Moore Dalal and Dr Steven D. DeMartini; used with permission [Citation ends]. Angiolipomas, which tend to be multiple and occur in young adults, may be painful when palpated. The overlying skin appears normal.[5] The differential diagnosis of a subcutaneous lipoma includes:[16]
Angiolipomas, which tend to be multiple and occur in young adults, may be painful when palpated. The overlying skin appears normal.[5] The differential diagnosis of a subcutaneous lipoma includes:[16]
Epidermoid cyst: these are usually smooth, rounded, and subcutaneous and feel firm (rather than the soft, doughy feel of a lipoma); they usually have a central punctum through which a white exudate can be expressed
Abscess: these are typically tender and surrounded by erythema
Liposarcoma.
On an extremity, liposarcoma may present as a deep-seated, painless, enlarging mass. Liposarcomas grow either slowly over many years or rapidly over a short time scale, and can reach a very large size. The majority present at a size larger than 5 cm. Studies suggest that a size of 10 cm or larger is a strong discriminating feature for liposarcoma.[20] Definitive diagnosis is dependent on histological confirmation.[16]
For lesions that are detected in more unusual locations, the physical examination should be modified to assess the organs most likely to be affected.
Imaging
Imaging is considered for lesions which are clinically deep to the superficial fascia, feel more solid than subcutaneous fat, immobile, or increasing in size.
Initial imaging of superficial lesions, e.g., lesions on the extremities, head, or neck, is with ultrasound.[31][32] Ultrasound has a sensitivity of 87% and a specificity of 96% for diagnosis of lipoma.[33] Urgent investigation is recommended for an unexplained lump that is increasing in size, to evaluate for soft tissue sarcoma.[34]
Magnetic resonance imaging (MRI) is a more detailed modality of choice due to its ability to attenuate bone artifact and discern the relationship of the mass to fascial planes, vessels, bones and nerves.[35][36][Figure caption and citation for the preceding image starts]: Intramuscular lipoma, right thigh. MRI, axial, T1-weighted image. Lipomatous mass in the anterior aspect of the right thighFrom the collection of Dr Kimberly Moore Dalal and Dr Steven D. DeMartini; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Intramuscular lipoma, right thigh. MRI, coronal, T1-weighted image. Lipomatous mass in the anterior aspect of the right thighFrom the collection of Dr Kimberly Moore Dalal and Dr Steven D. DeMartini; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Intramuscular lipoma, right thigh. MRI, coronal, T1-weighted image. Lipomatous mass in the anterior aspect of the right thighFrom the collection of Dr Kimberly Moore Dalal and Dr Steven D. DeMartini; used with permission [Citation ends].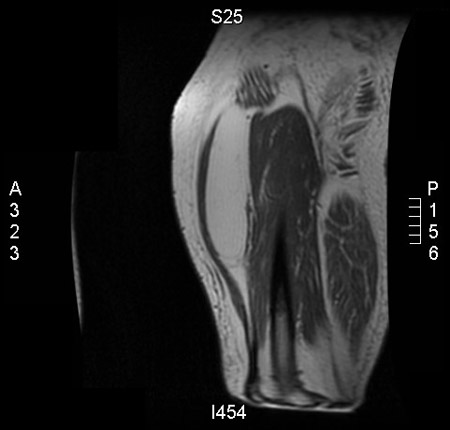
MRI is requested if the initial ultrasound is non-diagnostic.[31] Lesions that demonstrate septations or solid components, and are positioned deep to the superficial fascia or are infiltrating muscle, are likely to represent liposarcomas. In liposarcomas, septations or nodules generally demonstrate marked enhancement following administration of intravenous contrast (gadolinium).[20]
Conversely, lesions that appear homogeneous, with internal contents that are identical to subcutaneous fat on all MRI sequences, and that are located superficially, are likely to represent lipomas. Lipomas are typically non-enhancing or show only faint enhancement following administration of intravenous gadolinium.[20] However, lipomas may also contain muscle fibres, blood vessels, fibrous septa, and areas of necrosis or inflammation, which can make differentiation from well-differentiated liposarcomas difficult.[37]
If a lesion is on the trunk, particularly if it seems deep to the superficial fascia, computed tomography (CT) imaging is often preferred to MRI. CT with intravenous contrast may be ordered to evaluate deep tissue masses that are not amenable to ultrasound or radiographic evaluation.[31][Figure caption and citation for the preceding image starts]: Intramuscular lipoma of subscapularis muscle, CT scan. Right axillary soft-tissue fatty mass with well-circumscribed marginsFrom the collection of Dr Kimberly Moore Dalal and Dr Steven D. DeMartini; used with permission [Citation ends].
In patients with large gastrointestinal (GI) lipomas, a CT scan will demonstrate Hounsfield units identical to fat.[29] If a CT scan does not provide adequate information, an upper GI contrast study may provide additional functional information.[7][38]
Biopsy
Excisional biopsy is recommended for cutaneous or subcutaneous tumours smaller than 3 cm that are growing, are symptomatic (e.g., causing pain or pressure effects), or seem to have a solid component more firm than subcutaneous fat.[16]
In an adult, a soft-tissue mass should be considered for biopsy after imaging studies are completed if it shows any of the following characteristics, regardless of whether the lesion is on an extremity or the trunk:
Symptomatic
Enlarging
Larger than 3 cm in diameter
Recent onset and persisting beyond 4 weeks.
A core needle biopsy is the preferred biopsy method, and for superficial extremity or truncal lesions this can usually be performed under local anaesthetic, guided by direct palpation. Core needle biopsy can provide accurate diagnosis, and assessment of malignant potential and grade if examined by an experienced pathologist.[39] Should the tissue obtained by core biopsy be inadequate, a repeat core needle biopsy can be planned. If this is also non-diagnostic, an open, linearly placed incisional biopsy along the longitudinal axis of the limb and wide excision of the mass can be performed. A longitudinal incision is used so that the entire biopsy tract can be excised and the wound closed primarily should the lesion prove to be a liposarcoma. Fine needle aspiration is not helpful for the primary diagnosis of a mass as it provides only cells and does not provide information about overall tissue architecture.
Gastrointestinal lipomas that are encountered during upper endoscopy may be biopsied. Biopsy may not be required if the lipoma has a typical yellowish appearance on white light endoscopy and demonstrates the 'pillow sign' (the lipoma is easily deformed when pressed with closed biopsy forceps).[29]
Use of this content is subject to our disclaimer