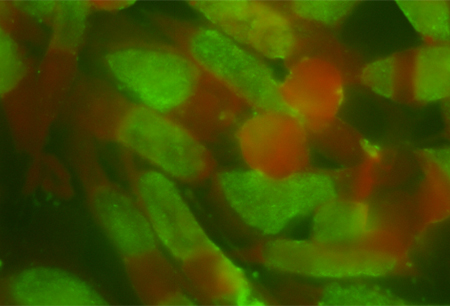
Infection is caused by Chlamydia psittaci, an obligate, intracellular, gram-negative bacterium.[1]Schlossberg D. Chlamydophila (chlamydia) psittaci (psittacosis). In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of infectious diseases, 6th ed. Philadelphia, PA: Churchill Livingston; 2005:2256-8. Contact with birds, for example among pet bird owners, people who work in zoos or pet shops, veterinarians, poultry and wildlife workers, and diagnostic laboratorians, appears to be the primary risk factor for infection.[13]National Association of State Public Health Veterinarians (NASPHV). Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (avian chlamydiosis). 2017 [internet publication].
http://www.nasphv.org/Documents/PsittacosisCompendium.pdf
Human infection can also result from indirect environmental exposure.[13]National Association of State Public Health Veterinarians (NASPHV). Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (avian chlamydiosis). 2017 [internet publication].
http://www.nasphv.org/Documents/PsittacosisCompendium.pdf
The association of C psittaci infection in humans exposed to birds and mammals has been known since the 1870s.[14]Harris RL, Williams TW Jr. "Contribution to the question of pneumotyphus": a discussion of the original article by J. Ritter in 1880. Rev Infect Dis. 1985 Jan-Feb;7(1):119-22.
http://www.ncbi.nlm.nih.gov/pubmed/3885364?tool=bestpractice.com
However, approximately 25% of affected patients deny exposure, which points to a lack of recognition of contact with an asymptomatic, but infected, bird or mammal.[13]National Association of State Public Health Veterinarians (NASPHV). Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (avian chlamydiosis). 2017 [internet publication].
http://www.nasphv.org/Documents/PsittacosisCompendium.pdf
Most infections are acquired from exposure to psittacine (parrot-type) birds, especially budgerigars and cockatiels. However, transmission has also been documented from nonpsittacine birds, most commonly pigeons and doves, as well as poultry, free-range birds, birds of prey, ducks, and shore birds.[13]National Association of State Public Health Veterinarians (NASPHV). Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (avian chlamydiosis). 2017 [internet publication].
http://www.nasphv.org/Documents/PsittacosisCompendium.pdf
[15]Hogerwerf L, Roof I, de Jong MJK, et al. Animal sources for zoonotic transmission of psittacosis: a systematic review. BMC Infect Dis. 2020 Mar 4;20(1):192.
https://www.doi.org/10.1186/s12879-020-4918-y
http://www.ncbi.nlm.nih.gov/pubmed/32131753?tool=bestpractice.com
Occupational exposure to commercially bred turkeys, other fowl, and mammals, or to infected tissue, can precipitate outbreaks of psittacosis.[6]Gaede W, Reckling KF, Dresenkamp B, et al. Chlamydia psittaci infections in humans during an outbreak of psittacosis from poultry in Germany. Zoonoses Public Health. 2008 May;55(4):184-8.
http://www.ncbi.nlm.nih.gov/pubmed/18387139?tool=bestpractice.com
Outbreaks have been observed on duck, turkey, and other poultry farms, among abattoir workers, and from exposure to feral pigeons.[1]Schlossberg D. Chlamydophila (chlamydia) psittaci (psittacosis). In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of infectious diseases, 6th ed. Philadelphia, PA: Churchill Livingston; 2005:2256-8.[5]Harkinezhad T, Geens T, Vanrompay D. Chlamydia psittaci infections in birds: a review with emphasis on zoonotic consequences. Vet Microbiol. 2009 Mar 16;135(1-2):68-77.
http://www.ncbi.nlm.nih.gov/pubmed/19054633?tool=bestpractice.com
[6]Gaede W, Reckling KF, Dresenkamp B, et al. Chlamydia psittaci infections in humans during an outbreak of psittacosis from poultry in Germany. Zoonoses Public Health. 2008 May;55(4):184-8.
http://www.ncbi.nlm.nih.gov/pubmed/18387139?tool=bestpractice.com
[16]Washington State Department of Health. Psittacosis: reporting and surveillance guideline. January 2018 [internet publication].
http://www.doh.wa.gov/Portals/1/Documents/5100/420-070-Guideline-Psittacosis.pdf
[17]Verminnen K, Duquenne B, De Keukeleire D, et al. Evaluation of a Chlamydophila psittaci infection diagnostic platform for zoonotic risk assessment. J Clin Microbiol. 2008 Jan;46(1):281-5.
http://jcm.asm.org/content/46/1/281.full
http://www.ncbi.nlm.nih.gov/pubmed/18003799?tool=bestpractice.com
[18]Telfer BL, Moberley SA, Hort KP, et al. Probable psittacosis outbreak linked to wild birds. Emerg Infect Dis. 2005 Mar;11(3):391-7.
http://wwwnc.cdc.gov/eid/article/11/3/04-0601_article
http://www.ncbi.nlm.nih.gov/pubmed/15757553?tool=bestpractice.com
[19]Queensland Department of Health, Australia. Animal contact guidelines - reducing the risk to human health 2014. August 2014 [internet publication].
https://www.health.qld.gov.au/publications/clinical-practice/guidelines-procedures/diseases-infection/governance/zoo-guidelines.pdf
[20]Magnino S, Haag-Wackernagel D, Geigenfeind I, et al. Chlamydial infections in feral pigeons in Europe: review of data and focus on public health implications. Vet Microbiol. 2009 Mar 16;135(1-2):54-67.
http://www.ncbi.nlm.nih.gov/pubmed/18977610?tool=bestpractice.com
[21]Laroucau K, de Barbeyrac B, Vorimore F, et al. Chlamydial infections in duck farms associated with human cases of psittacosis in France. Vet Microbiol. 2009 Mar 16;135(1-2):82-9.
http://www.ncbi.nlm.nih.gov/pubmed/18947944?tool=bestpractice.com
[22]Heddema ER, van Hannen EJ, Duim B, et al. Genotyping of Chlamydia psittaci in human samples. Emerg Infect Dis. 2006 Dec;12(12):1989-90.
http://wwwnc.cdc.gov/eid/article/12/12/05-1633_article
http://www.ncbi.nlm.nih.gov/pubmed/17326961?tool=bestpractice.com
There have also been reports of outbreaks associated with bird shows and in veterinary teaching hospitals.[23]Koene R, Hautvast J, Zuchner L, et al. Local cluster of psittacosis after bird show in the Netherlands, November 2007. Euro Surveill. 2007 Dec 13;12(12):E071213.1.
http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=3328
http://www.ncbi.nlm.nih.gov/pubmed/18082112?tool=bestpractice.com
[24]Heddema ER, van Hannen EJ, Duim B, et al. An outbreak of psittacosis due to Chlamydia psittaci genotype A in a veterinary teaching hospital. J Med Microbiol. 2006 Nov;55(Pt 11):1571-5.
https://www.microbiologyresearch.org/content/journal/jmm/10.1099/jmm.0.46692-0#tab2
http://www.ncbi.nlm.nih.gov/pubmed/17030918?tool=bestpractice.com
[25]Chan J, Doyle B, Branley J, et al. An outbreak of psittacosis at a veterinary school demonstrating a novel source of infection. One Health. 2017 Feb 24;3:29-33.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5454149
http://www.ncbi.nlm.nih.gov/pubmed/28616500?tool=bestpractice.com
Certain strains that infect poultry and psittacine birds tend to be more virulent.[1]Schlossberg D. Chlamydophila (chlamydia) psittaci (psittacosis). In: Mandell GL, Bennett JE, Dolin R, eds. Principles and practice of infectious diseases, 6th ed. Philadelphia, PA: Churchill Livingston; 2005:2256-8.[6]Gaede W, Reckling KF, Dresenkamp B, et al. Chlamydia psittaci infections in humans during an outbreak of psittacosis from poultry in Germany. Zoonoses Public Health. 2008 May;55(4):184-8.
http://www.ncbi.nlm.nih.gov/pubmed/18387139?tool=bestpractice.com
Human-to-human transmission is thought to be rare and can cause more severe disease.[5]Harkinezhad T, Geens T, Vanrompay D. Chlamydia psittaci infections in birds: a review with emphasis on zoonotic consequences. Vet Microbiol. 2009 Mar 16;135(1-2):68-77.
http://www.ncbi.nlm.nih.gov/pubmed/19054633?tool=bestpractice.com
[26]Ito I, Ishida T, Mishima M, et al. Familial cases of psittacosis: possible person-to-person transmission. Intern Med. 2002 Jul;41(7):580-3.
https://www.jstage.jst.go.jp/article/internalmedicine1992/41/7/41_7_580/_article
http://www.ncbi.nlm.nih.gov/pubmed/12132529?tool=bestpractice.com
[27]Wallensten A, Fredlund H, Runehagen A. Multiple human-to-human transmission from a severe case of psittacosis, Sweden, January-February 2013. Euro Surveill. 2014 Oct 23;19(42):20937.
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES2014.19.42.20937
http://www.ncbi.nlm.nih.gov/pubmed/25358043?tool=bestpractice.com