Investigations
1st investigations to order
serum thyroid-stimulating hormone (TSH)
serum total T4, total T3, free T3, free T4 index, and free T4
T3:T4 ratio
radioactive iodine uptake
Test
Always very low during the thyrotoxic phase. [Figure caption and citation for the preceding image starts]: I-123 radioactive iodine scan showing absence of thyroid uptake in thyroiditis and thyrotoxicosis; arrow indicates sternal notch markerFrom the personal collection of Dr Stephanie Lee [Citation ends].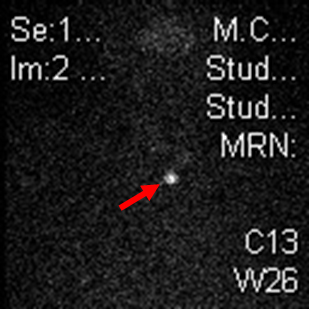
May be elevated during the recovery from hypothyroidism.[1][2]
Result
very low thyroidal uptake, typically <1% to 3% at 24 hours.
Serum ESR
Test
Non-specific but are likely to be elevated in most patients. The average rate in a study of patients with subacute thyroiditis was 53 mm/hour.[2]
Result
elevated (>40 mm/hour)
Serum CRP
Test
Significantly elevated (i.e., >10 mg/L) in 86% of patients with subacute thyroiditis, but not in patients with other thyroid conditions, such as Graves' disease, toxic nodular goitre, or amiodarone-induced thyrotoxicosis (type I and II).[20]
Thus serum CRP levels may help when, based on laboratory and imaging studies, the diagnosis of subacute thyroiditis is not clear.[21]
Result
elevated (>10 mg/L)
Serum thyroid antibodies (thyroid peroxidase antibodies [TPO Ab])
Test
Generally not useful to confirm or exclude the diagnosis. Usually normal in the patient at initial presentation of the thyrotoxic phase.
Result
normal or mildly elevated
Investigations to consider
fine needle aspiration biopsy
Test
These cytological features would be present in the area of thyroid pain in most patients.[29]
However, a biopsy is not routinely performed, as the diagnosis of subacute thyroiditis may be made based on the clinical presentation of thyroid pain, viral-like syndrome, biochemical thyrotoxicosis, and low radioiodine thyroid uptake. However, cytology can be useful to confirm a clinical diagnosis in the setting of high iodine intake, such as in an individual who recently received iodinated contrast for radiological scans, or in an individual who used an iodine-rich medication such as amiodarone.
Result
Multi-nucleated giant cells, with a background of degenerated follicular epithelium cells, rare epithelioid granulomas, and mixed inflammatory cells
full blood count
Test
Mild anaemia and elevation of white blood cell count are common.
Result
may show low level of haemoglobin or haematocrit; leukocyte count may be elevated
Emerging tests
ultrasonography of thyroid
Test
Approximately 78% to 90% of patients with painful subacute thyroiditis have ill-defined areas of hypoechoic echotexture on ultrasonography.[1][23][24][25][26]
Normal or decreased vascular flow can distinguish this condition from Graves' disease, which typically displays generalised increased vascular flow.[27]
However, the sensitivity and specificity of ultrasound appearance is not well-established, and ultrasound should not be used alone for the diagnosis of subacute thyroiditis. Ultrasound is not superior to a radioactive iodine uptake scan for the diagnosis of subacute thyroiditis because the appearance is not specific and can be similar to the sonographic appearance of chronic thyroiditis. New technology utilising real-time ultrasound elastography demonstrated that lesions of subacute thyroiditis had an elevated elasticity score compared with benign nodules of a multinodular goitre, but could not be distinguished from malignant nodules, which also had elevated elasticity scores.[28]
Result
focal heterogeneous hypoechogenicity with irregular margins in the area that is painful; decreased internal vascular flow with decreased or normal peripheral vascular flow by Doppler ultrasound
Use of this content is subject to our disclaimer