Approach
In any patient with thrombocytopenia, exclude pseudothrombocytopenia (a laboratory artifact attributable to the presence of EDTA-dependent antibody in the circulation) by one of the following:
Perform a fingerstick peripheral smear
Draw the blood into a heparin or citrated tube
Manually count on a sample diluted without anticoagulants.
Once true thrombocytopenia is confirmed, clinical history, examination, full blood count, and peripheral blood smear will narrow down the differential diagnosis.
History
Key symptoms: it is important to identify the time in which symptoms began, to establish whether thrombocytopenia is acute or chronic.
Easy bruising
Petechiae
Epistaxis
Gum bleeding
Gastrointestinal or genitourinary bleeding.
Associated symptoms are often non-specific but may be indicative of:
Malignancy:
Bone pain
Night sweats
Nausea
Anorexia
Fatigue/malaise
Weakness
Shortness of breath
Left upper quadrant discomfort (splenomegaly)
Excessive thirst, urination, and constipation (myeloma).
Infection:
Fever
Cough
Shortness of breath
Altered sense of smell or taste
Haemoptysis (tuberculosis)
Night sweats
Chills
Rigors
Rash
Pharyngitis (infectious mononucleosis)
Diarrhoea, vomiting, and nausea.
Inflammatory or autoimmune disorders:
Joint discomfort
Arthralgias
Morning stiffness (rheumatoid arthritis)
Malar rash (systemic lupus erythematosus [SLE])
Fatigue
Weight loss
Cough
Dyspnoea
History of miscarriage (antiphospholipid syndrome)
Diarrhoeal illness in child (haemolytic uraemic syndrome [HUS])
Confusion, seizures, and neurological changes (thrombotic thrombocytopenic purpura [TTP]).
Intravascular trauma:
Recent surgery or procedure
Confusion, dyspnoea, and cough (disseminated intravascular coagulation [DIC]).
Toxicity:
Excess alcohol.
Genetic disorders:
Atopy (Wiskott-Aldrich syndrome)
Hearing loss (May-Hegglin anomaly)
Familial thrombocytopenia and/or presence of myeloid neoplasms in an immediate family member.
Endocrine disorders:
Symptoms of hypothyroidism: for example, weight gain, constipation, fatigue.
Other:
Symptoms of anaemia: for example, fatigue, breathlessness, pallor
Abdominal distension (paroxysmal nocturnal haemoglobinuria), portal vein thrombosis/Budd-Chiari syndrome
Pruritus, early satiety, left upper quadrant pain, alcohol withdrawal (cirrhosis).
Additional history:
Old platelet counts to verify a history of low or normal levels
Infection with certain viruses, particularly HIV and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
History of rheumatological conditions
History of malignancy
A recent history of surgery or transfusion is important
Family history of bleeding or low platelet counts
Dietary (e.g., folic acid), B12 low in pernicious anaemia (although anaemia may be more important presenting problem)
Travel to endemic area (malaria)
Recent illnesses
Recent injections such as vaccinations
Intensive care unit admission
Alcohol or illicit drug misuse (cirrhosis).
Female patients:
Pregnancy status is important as patients are at risk for TTP, gestational thrombocytopenia (in which secreted placental factors lead to a decrease in platelet count), and haemolysis, elevated liver enzymes, low platelets (HELLP) syndrome.
Medication history:
Recent ingestion of new medications
Quinine exposure (e.g., tonic water ingestion, non-prescription pills for leg cramps)
Sulfur-containing medicines and antiepileptic medicines
Chemotherapeutic drugs, which may be used for treatment of neoplastic disorders, vasculitis, inflammatory bowel disease, and other rheumatological disorders
Exposure to heparin.
Physical examination
Key clinical findings pertinent to thrombocytopenia:
Petechiae or ecchymoses
Retinal haemorrhage, a possible sign of intracranial haemorrhage
Bleeding occurring at the back of the buccal mucosa, advancing to the front, is often a worrisome finding for impending intracranial bleeding in an individual with an extremely low platelet count.
Vital signs
Fever may indicate infection, leukaemia, lymphoma, DIC, TTP, SLE, sarcoidosis or aplastic anaemia
Hypotension and tachycardia can occur in DIC and sepsis
Hypertension is a feature of HELLP syndrome.
Other physical findings should be identified to narrow the diagnosis:
General examination
Lymphadenopathy
Pallor
Bleeding at sites of intravascular lines, dialysis catheters, extracorporeal oxygenation devices, chest tubes, mediastinal or pericardial tubes
White spots on tongue (oropharyngeal candidiasis may be seen in HIV/AIDS)
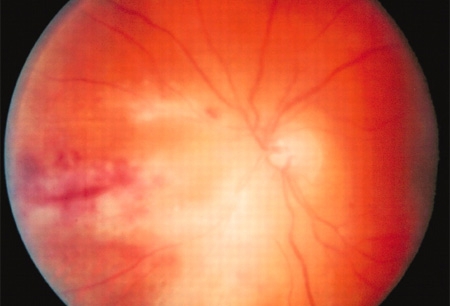
Retinal changes (cytomegalovirus infection)[Figure caption and citation for the preceding image starts]: Fundoscopy (left eye) showing area of CMV retinitis inferonasally involving the vascular arcades and the optic disc, associated with vasculitis, and flame haemorrhagesAdapted from BMJ Case Reports 2009 (10.1136/bcr.02.2009.1576) [Citation ends].
Jaundice (may occur in malaria, TTP, HELLP syndrome, and cirrhosis)
Signs of hypothyroidism: peripheral oedema, hair loss, bradycardia, hypothyroid facies, enlarged thyroid gland
Signs of chronic liver disease (spider telangiectasias on the chest, palmar erythema, pedal oedema).
Abdominal examination
Hepatosplenomegaly (may occur in leukaemia, lymphoma, bone marrow fibrosis, post-transfusion thrombocytopenia, malaria, Wiskott-Alrich syndrome, Gaucher's disease)
Ascites (cirrhosis).
Cardiovascular examination
Irregular pulse may occur in TTP.
Musculoskeletal examination
Joint deformity or swelling (SLE, rheumatoid arthritis)
Digital ischaemia and/or swollen extremities (antiphospholipid syndrome)
Bone pain (multiple myeloma)
Bone fractures (multiple myeloma).
Neurological examination
Weakness or leg numbness (multiple myeloma)
Confusion may occur in DIC and TTP
Seizures and focal neurological symptoms may also occur in TTP
Decreased vibratory sensation and dementia may indicate vitamin B12 deficiency.
Initial tests
The peripheral blood smear is an important next step in identifying the cause of thrombocytopenia.
Immune thrombocytopenia (ITP) is a diagnosis of exclusion, and the peripheral smear will show solely a low platelet count. The red cells should appear normal.[4]
Schistocytes and nucleated red blood cells along with thrombocytopenia on the smear indicate either TTP, HUS, or DIC. Schistocytes are also seen in sepsis.
Blasts on the peripheral smear raise the possibility of acute leukaemia. If the peripheral blood smear shows blasts, the patient must be promptly referred to a haematologist/oncologist or other appropriate specialist.
Rouleaux formation indicates multiple myeloma.
Leukoerythroblastic changes may be seen in metastatic malignancy and bone marrow fibrosis.
Atypical lymphocytes may be seen in mononucleosis.
Macrocytosis can indicate alcohol misuse, B12 deficiency, or folate deficiency.
Hypersegmented polymorphonuclear cells are a feature of B12 or folate deficiency.
Small platelets occur in Wiskott-Aldrich syndrome.
Large platelets occur in MYH9-related disorders, including May-Hegglin anomaly, and Bernard-Soulier syndrome. Döhle bodies in polymorphonuclear cells are also seen in MYH9-related disorders.
Platelet clumping will be visible in cases of pseudothrombocytopenia.
FBC with differential:
Identifies the extent of thrombocytopenia.
Identifies concomitant anaemia, leukocytopenia, or leukocytosis.
It is important to review any previous FBC results for history of low platelet count.
Pseudothrombocytopenia shows low counts with an EDTA tube. However, platelet count is normal using a citrate- or heparin-coated tube.
Targeted tests
The results of the peripheral smear together with the clinical findings should narrow down the differential diagnosis and guide further investigation.
Laboratory investigations
Serum creatinine may be elevated in TTP, HUS, SLE, sepsis, and multiple myeloma. BUN may be elevated and serum electrolytes deranged in sepsis.
Liver function tests (LFTs) (including bilirubin, alanine aminotransferase [ALT], aspartate aminotransferase [AST], and albumin) can distinguish between HELLP and gestational thrombocytopenia. Characteristic changes in cirrhosis include low serum albumin and elevated bilirubin. Malaria, dengue fever, and Epstein-Barr virus infection can cause elevated transaminases. LFTs may be deranged in sepsis. Indirect bilirubin is elevated if there is haemolysis.
Serum calcium: may be elevated in multiple myeloma and sarcoidosis.
Prothrombin time (PT), activated partial thromboplastin time (PTT), and fibrinogen can help to distinguish between DIC, post-transfusion thrombocytopenia, ITP, and TTP. PT and activated PTT are prolonged in cirrhosis. Coagulation studies may be abnormal in sepsis.
D-dimer is elevated in DIC and normal in TTP.
Serum reticulocyte count and lactate dehydrogenase (LDH) are elevated in haemolysis.
Uric acid is elevated in acute myelogenous leukaemia.
If multiple myeloma is suspected, serum and urine protein electrophoresis, serum calcium, serum free light chains, and serum beta-2-microglobulin should be measured.
If autoimmune or inflammatory conditions such as SLE, rheumatoid arthritis, antiphospholipid syndrome, and sarcoidosis are suspected, erythrocyte sedimentation rate, antinuclear antibodies, anti-double-stranded DNA antibodies, anti-Smith antibodies, rheumatoid factor, anti-cyclic citrullinated peptide antibodies, anticardiolipin antibodies, anti-beta2-glycoprotein I antibody, and lupus anticoagulant may help to differentiate the diagnosis.
Hashimoto's thyroiditis is confirmed with anti-microsomal antibodies. Thyroid function tests show elevated thyroid stimulating hormone and low T4.
If B12 or folate deficiency is suspected, low levels will confirm diagnosis.
If an infective process is suspected, then the following tests should be ordered:
Sepsis: blood cultures, arterial blood gas, serum lactate, C-reactive protein, cultures from the suspected site of infection
COVID-19: real-time reverse transcriptase polymerase chain reaction to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
Mononucleosis: heterophile antibody agglutination test, Epstein-Barr virus-specific antibodies
HIV: HIV antibody test plus CD4 count identifies the presence and progression of the HIV virus
Cytomegalovirus: serology
Sputum stain for acid-fast bacilli or nucleic acid amplification tests if there is suspicion of tuberculosis.
Urinalysis: indicated in cases of suspected malaria, SLE, gestational thrombocytopenia, and paroxysmal nocturnal haemoglobinuria.
Imaging tests
Computed tomography (CT) head is essential if there is suspicion for intracranial haemorrhage.
Skeletal survey, including x rays of the long bones, skull, and spine, is performed in all patients with suspected multiple myeloma. Whole-body low-dose CT may also be used for this purpose.[36]
A CT of the abdomen helps identify pathology such as cirrhosis, splenomegaly, metastases, or lymphoma.
Chest x ray may show signs of miliary tuberculosis, lung cancer, or sarcoidosis.[Figure caption and citation for the preceding image starts]: Bilateral hilar adenopathy, associated with sarcoidosisFrom the collection of Muthiah P. Muthiah, MD, FCCP [Citation ends].

Specialised tests
Bone marrow aspiration and/or biopsy is performed if other studies are inconclusive. Bone marrow aspiration and/or biopsy may be used in the diagnosis of leukaemia, multiple myeloma, bone marrow fibrosis, ITP, TTP, HIV, and aplastic anaemia. Bone marrow biopsy is usually only performed for suspected ITP if the clinical presentation is atypical or the patient does not respond to ITP therapy.
Cytogenetic analysis of bone marrow yields prognostic information in leukaemia and multiple myeloma.
Lymph node biopsy is indicated for suspected lymphoma.
Antigen assays for heparin-induced thrombocytopenia (HIT) antibodies are used to diagnose HIT.
If a genetic disorder is suspected, specific tests including single gene sequencing, next generation sequencing, skin fibroblast culture, and platelet flow cytometry may be required.[37]
Use of this content is subject to our disclaimer