Aetiology
Viruses account for approximately 70% to 87% of episodes of acute gastroenteritis in children, with Rotavirus and Norovirus being the two most common identifiable causes.[7][8] Prior to routine rotavirus vaccination, rotavirus was the most common cause of gastroenteritis in the paediatric age group. Currently, norovirus is the most common cause of viral gastroenteritis.[9]
Other viral pathogens include caliciviruses, astroviruses, and adenoviruses.[10] Other viruses such as coronaviruses, parvoviruses, and picobirnaviruses have also been linked to human gastroenteritis.
1. Rotaviruses
Worldwide, approximately 30% to 72% of young children hospitalised with diarrhoea have been reported as infected with Rotavirus.[11] At the community level, rotavirus infection accounts for approximately 4% to 24% of gastroenteritis cases.[12] In outbreaks of gastroenteritis in children attending daycare centres, rotavirus accounts for 20% to 40% of cases.[11] Rotavirus gastroenteritis is most common and severe in children 6-24 months of age. Infections during the first few months of life are often mild or asymptomatic, possibly owing to maternal antibodies.[13]
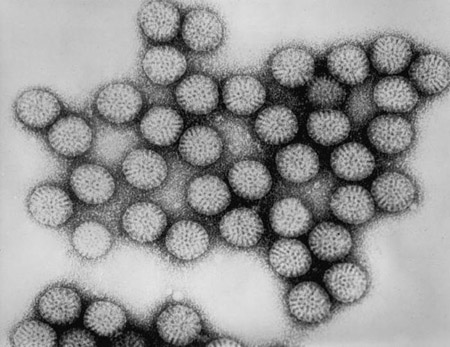
Rotavirus is a non-enveloped double-stranded RNA virus of the Reoviridae family. The virus is so named because of its characteristic appearance on electron microscopy as a hubbed wheel with spokes. The outer viral capsid is composed of 2 structural proteins, VP4 and VP7; the inner capsid is composed of VP6; and the core is composed of VP1, VP2, and VP3. VP6 is the major group-specific antigen. Rotaviruses can be classified into 7 groups (A to G) on the basis of VP6 differences. Group A is the most common rotavirus causing human illness.[14] Serotype specificity is determined by VP4 and VP7, according to their reactivity with neutralising antibodies. Rotaviruses are generally species-specific, but cross-species transmission may occur.[15] Rotavirus is ubiquitous and almost all children are infected by 3 years of age.[14][Figure caption and citation for the preceding image starts]: Transmission electron micrograph of intact rotavirus particles, double-shelled. Distinctive rim of radiating capsomeresCDC/Dr Erskine Palmer; used with permission [Citation ends].
2. Caliciviruses
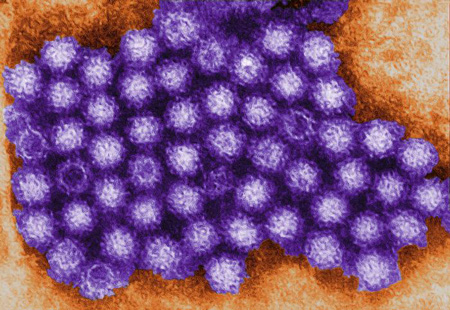
Caliciviruses are non-enveloped, positive-sense, single-stranded RNA viruses of the Caliciviridae family. They are so-called because of the characteristic cup-shaped depressions over the surface of the virion. Caliciviruses are divided into 4 genera: Norovirus (previously known as Norwalk virus), Sapovirus, Vesivirus, and Lagovirus. Only Norovirus and Sapovirus cause gastroenteritis in humans; they are called human caliciviruses. Human caliciviruses can cause large outbreaks of gastroenteritis in all age groups through contaminated food or water.[16][Figure caption and citation for the preceding image starts]: This transmission electron micrograph reveals some of the ultrastructural morphology displayed by norovirus virions, or virus particlesCDC/Charles D. Humphrey; used with permission [Citation ends].
3. Astroviruses
Astroviruses are non-enveloped, positive-sense, single-stranded RNA viruses of the Astroviridae family. They are so-named because of their characteristic star-like appearance on electron microscopy. Astroviral gastroenteritis has been associated with outbreaks of mild gastroenteritis in daycare centres, schools, and paediatric wards, as well as in nursing homes.[17] Astroviral gastroenteritis mainly affects children under 1 year old.[18][19]
4. Adenoviruses
Pathophysiology
Of all the viruses that may cause gastroenteritis in children, Rotavirus is the best studied. Rotavirus preferentially infects enterocytes in the mature small intestine after it has been activated by cleavage of VP4 by trypsin-like proteases.[22] Infection is initiated in the proximal end of the intestine and spreads distally but is generally confined to the intestinal mucosa. Multiplication of the rotavirus particles in mature enterocytes leads to destruction of these cells.[23] Villous tips receive the most extensive damage, with sparing of the crypts. Viable crypt cells undergo rapid division.
Mechanisms of excessive secretion
Loss of villous tips and the filling of crypts with rapidly multiplying cells results in a marked decrease in the surface area of the gut lumen.
Villous cell dysfunction during infection leads to an imbalance between absorption and secretion, resulting in a net secretion (villous cells are largely absorptive and crypt cells are secretory).
Increased enterocyte turnover results in immature enterocytes that have impaired absorptive capacity.[24]
The virus destroys disaccharidases in the small intestine.
Rotavirus enterotoxin (NSP4) may cause release of calcium from the endoplasmic reticulum, with resultant increased secretion from the villous cells.[23][25]
Stimulation of the enteric nervous system by NSP4 and villous ischaemia may further aggravate the diarrhoea.[23]
Substantial fluid and electrolyte loss may result in dehydration, electrolyte imbalance, and metabolic acidosis. If uncorrected, this may lead to circulatory collapse, shock, end-organ hypoperfusion, and tissue damage.
Use of this content is subject to our disclaimer