Aetiology
Common causes of upper extremity mononeuropathy can be broadly divided into compression neuropathies and idiopathic neuropathies. Less common, but important, causes are malignancy and vasculitis.
Compression neuropathies
Carpal tunnel syndrome
This is the most common mononeuropathy of the upper extremity.[2][4] It results from compression of the median nerve in the carpal tunnel. Most cases appear to be idiopathic. It is more common in women.[2][4] Incidence increases during pregnancy, particularly the third trimester.[4][5] Other risk factors include jobs or activities involving repetitive wrist flexion, extension, or both.[6][7] The incidence seems to be higher in manual labourers.[7] However, despite popularly held opinion, no definite relationship has been shown between typing/computer use and carpal tunnel syndrome.[4] Occasionally patients have a ganglion cyst or lipoma at the wrist compressing the median nerve, mimicking carpal tunnel syndrome.[Figure caption and citation for the preceding image starts]: Severe bilateral carpal tunnel syndrome resulting in atrophy of abductor pollicis brevisFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].

Ulnar neuropathy at the elbow
This is the second most common compression neuropathy of the upper extremity.[2] It most commonly results from chronic mechanical compression of the ulnar nerve at the ulnar groove or cubital tunnel (cubital tunnel syndrome). Case reports and the clinical impression of electromyographers is that risk factors include chronic minor trauma caused by leaning on the elbow, prolonged periods of elbow flexion, and/or repetitive flexion/extension of the elbow. Elbow deformities, elbow fractures, and surgery under general anaesthetic are also considered risk factors for the development of ulnar neuropathy at the elbow.[8] Other less common causes of ulnar neuropathy at the elbow include a ganglion cyst or lipoma compressing the ulnar nerve. In patients from endemic regions, leprosy is a frequent cause of ulnar neuropathy at the elbow.[9][Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on dorsum of handFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
 [Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on palmFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].
[Figure caption and citation for the preceding image starts]: Approximate distribution of ulnar sensory nerve on palmFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].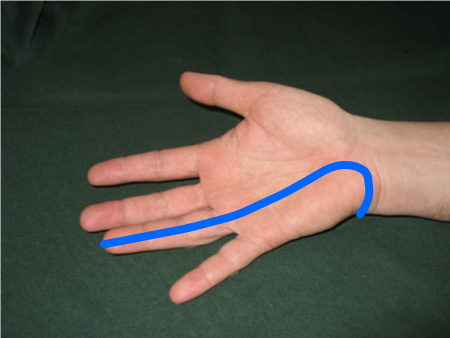
Ulnar neuropathy at the wrist/palm
This is a very rare cause of ulnar compression neuropathy. It is occasionally seen in cyclists, presumably due to pressure from the handlebars on the base of the wrist.[10] Ganglion cysts or other structural lesions in the palm are another cause of distal ulnar neuropathies.[Figure caption and citation for the preceding image starts]: Severe ulnar neuropathy; note atrophy of first dorsal interosseus and inability to extend proximal interphalangeal (PIP) joints of 4th and 5th digitsFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].

Radial neuropathy
This is the third most common upper extremity mononeuropathy seen by family physicians.[1] Trauma with associated fracture of the humerus is by far the most common cause of radial neuropathy.[2][3] The next most frequent cause is compression over the spiral groove (Saturday night palsy).[2] As its name suggests, this most commonly occurs after a deep sleep (usually associated with drug or alcohol intoxication), during which persistent pressure has been applied to the medial aspect of the arm, generally because the arm is positioned over the back of a chair or other hard surface.
Not all patients are intoxicated. Radial neuropathies have also been reported as a result of sleeping with the arm outstretched while another person rests their head on the arm (honeymooner's palsy).[2][Figure caption and citation for the preceding image starts]: Approximate distribution of radial sensory nerveFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].

Cervical radiculopathy
Although technically not a mononeuropathy, cervical radiculopathy needs to be considered in the differential diagnosis of patients presenting with symptoms of upper extremity pain, paraesthesiae, numbness, and/or weakness. Patients typically present with a complaint of pain radiating from the neck down into the arm or hand. This symptom is often exacerbated by neck movement. Frequently, the pain is associated with paraesthesiae in the distribution of the affected nerve (C5 = lateral elbow, C6 = thumb, C7 = middle finger, C8 = fifth digit, T1 = medial elbow). When more severe compression occurs, patients will experience persistent paraesthesiae, numbness, and/or weakness in the distribution of the affected nerve root. The most common nerve roots involved are C6 and C7.
The most frequent finding on examination is loss or depression of the affected reflex (C6 = biceps and/or brachioradialis reflex, C7 = triceps reflex). Sensory loss does not usually affect the entire dermatome, and weakness can be subtle (due to muscle innervations by multiple nerve roots). C5 radiculopathy can result in biceps and deltoid weakness, C6 in wrist extensor weakness, C7 in triceps weakness, and C8T1 in intrinsic muscle weakness.
The most common cause is compression from a cervical disc herniation or from chronic spondylotic changes (e.g., osteophytes). Less common causes are trauma, malignancy, or infection.
Neurogenic thoracic outlet syndrome
This is an extremely rare cause of hand numbness and weakness. It primarily affects young or middle-aged women. It is insidious in onset.[11] Weakness and atrophy of the small muscles of the hand, particularly abductor pollicis brevis and first dorsal interosseus, is the most common presenting symptom and sign. Pain and sensory symptoms are not prominent. Occasionally, patients complain of an aching in the medial arm and/or of numbness or paraesthesiae in the medial hand (4th and 5th digits) and forearm.
Neurogenic thoracic outlet syndrome is caused by compression of the lower trunk of the brachial plexus, associated with an elongated transverse process of the C7 vertebra. In many cases, a fibrous band extends from the elongated transverse process to the first thoracic rib, and this band is believed to cause the compressive symptoms. The diagnosis is made by demonstrating the presence of an elongated transverse process (cervical rib) at C7 in a patient with a lower trunk brachial plexus lesion on nerve conduction studies.[Figure caption and citation for the preceding image starts]: Marked atrophy of both the thenar eminence and the first dorsal interosseus is seen in thoracic outlet syndrome; it should be noted that this is an extremely rare diagnosisFrom the collection of Hannah R. Briemberg, MD, FRCPC [Citation ends].

Idiopathic neuropathies
Posterior interosseus syndrome
This is a rare syndrome affecting the distal branch of the radial nerve (posterior interosseus nerve).[3] Patients present with mild weakness of wrist extension and more severe weakness of finger and thumb extension. It is a pure motor nerve so there is no associated sensory loss. Some patients complain of associated pain in the region of the radial head but this is not universal. Posterior interosseus neuropathy may result from trauma to the radial head and occasionally from ganglia or other mass lesions in this region. Most other cases are felt to be idiopathic. Some have argued that these cases are due to compression of the nerve by fibrous tissue at the arcade of Frohse. This is controversial, as the arguments put forward to support this theory are not specific for compression neuropathies. The natural history in many cases is similar to that of idiopathic brachial neuritis, and many neurologists believe that isolated posterior interosseus neuropathy is a variant of brachial neuritis.
Anterior interosseus syndrome
This is another rare syndrome affecting a distal branch of the median nerve.[12] The anterior interosseus nerve innervates flexor pollicis longus, flexor digitorum profundus to digits 2 and 3, and pronator quadratus. Usually the lesion is incomplete, and the primary weakness occurs in flexor pollicis longus. Patients lose the ability to flex the distal phalanx of the thumb and complain of a weak pinch. A weak pinch is also a primary complaint in ulnar neuropathies.
Most cases are idiopathic and felt to be a variant of brachial neuritis. Occasional cases result from trauma to the forearm. Compressive lesions are another cause. Compressive lesions should be considered when the weakness is progressive.
Brachial neuritis
This goes by several names including brachial amyotrophy, Parsonage-Turner syndrome, and idiopathic acute brachial plexopathy. The cause is unknown. Patients present with the acute onset of severe unprovoked shoulder pain, typically centred in the region of the scapula and radiating from there into the neck and shoulder.[13] The pain typically lasts from 3 to 14 days, although it may be longer or shorter. Several days after the onset of the pain, the patient develops marked weakness and atrophy in the shoulder region. Complaints of sensory loss or paraesthesia are extremely unusual and generally suggest another diagnosis (compressive lesion, cervical radiculopathy).
Although any nerve in the upper extremity may be affected, the most common presentation is with new-onset scapular winging, and weakness and atrophy of the shoulder muscles (deltoid, supraspinatus, and infraspinatus). Distal nerves may also be involved, however, particularly the anterior interosseus nerve with subsequent loss of the ability to flex the distal phalanx of the thumb. Occasionally the phrenic nerve is involved. In general, this is asymptomatic, although it may be identified by an elevated haemidiaphragm on chest x-ray. Brachial neuritis can generally be differentiated from compressive brachial plexopathies by the acute presentation followed by a plateau and then subsequent improvement in most cases.
Amyotrophic lateral sclerosis (ALS)
This is a neurodegenerative disease affecting both upper and lower motor neurons. The most common early clinical features are unilateral distal muscle weakness and atrophy in upper or lower limb muscles.[14] The weakness is painless and insidious in onset. Sensation is not affected. Typically at the time of presentation there is already significant muscle atrophy. Other clues on history and physical examination that help to differentiate ALS from the more common mononeuropathies of the upper extremity include a history of exertional muscle cramps, fasciculations, hyperreflexia in the affected limb, and weakness that cannot be localised to an individual nerve distribution (i.e., weakness of all median, ulnar, and radial innervated hand muscles) without sensory findings.
Malignant, inflammatory, or infectious causes
Although comparatively rare, the most worrying causes of mononeuropathy in the upper extremity are:
Vasculitis
Malignancy (primarily associated with lesions of the brachial plexus).
Other rare causes are:
Infection: leprosy, cytomegalovirus, HIV, Lyme disease
Sarcoidosis
Amyloidosis
Multifocal chronic inflammatory demyelinating polyneuropathy
Hereditary neuropathy with liability to pressure palsies
Post-irradiation brachial plexopathy.
Use of this content is subject to our disclaimer