Investigations
1st investigations to order
upper gastrointestinal contrast series
Test
Diagnostic standard test for malrotation, and should be performed with AP and lateral projections if there is any history of bilious vomiting without previous abdominal surgery.
Normal pattern of rotation: the transition of duodenum to jejunum (ligament of Treitz) lying left of the left vertebral pedicles in AP view. The position of this transition should also be at the level of the pylorus or superior to this.[Figure caption and citation for the preceding image starts]: Malrotation with volvulus without obstruction as seen on upper GI contrastFrom the collection of Dr S.D. St Peter [Citation ends].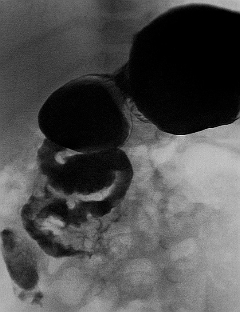
Normal anatomy on this examination rules out malrotation, midgut volvulus, and obstruction of the upper small intestine.
Delayed images in 1 or 2 hours can depict or rule out obstruction of the distal small bowel.
Result
right-sided duodenum (malrotation); duodenum courses inferior or medial to normal (malrotation); bird-beak cut-off of duodenum (volvulus); corkscrew of duodenum (volvulus); a web in the duodenum (duodenal atresia)
CT abdomen (with oral and intravenous [IV] contrast)
Test
Should be ordered when the presentation is abdominal pain without witnessed vomiting, and the concern for malrotation is low. If midgut volvulus is being considered, then CT scan should not be performed before an upper gastrointestinal (GI) series.[10]
Performed using oral and IV contrast to delineate intestinal pathologies.
Coronal reconstructions are particularly useful in following the course of the duodenum to assure the transition from duodenum to jejunum lies left of the left side of the spine and is appropriately high enough.
Additional information that can be obtained from the scan, which is not offered by the upper GI contrast series, is immediate assessment of caecal position/colonic rotation and 3-dimensional evaluation of the entire extra-intestinal space.
Result
no oral contrast beyond duodenum (volvulus); no contrast in the distal superior mesenteric artery (volvulus with ischaemia); twirling of the superior mesenteric artery and vein (volvulus); transposition of superior mesenteric artery and vein (malrotation); a transition point in bowel calibre, right-sided duodenum; duodenum courses anterior or to right of superior mesenteric artery
abdominal plain x-rays
Test
Usually ordered in the emergency department for patients presenting with abdominal complaints, but is rarely helpful in changing management or preventing other tests.
In the newborn nursery, a patient with bilious vomiting should be studied first with emergency plain films, as they provide a better yield for demonstrating other congenital aetiologies for symptoms.
Stomach and proximal duodenum distended with gas and some distal gas is the most consistent but non-specific sign of volvulus on plain films.[9]
The build-up of air in the stomach and proximal duodenum during volvulus may give the double-bubble appearance that is otherwise pathognomonic for duodenal atresia, but if any air is present distally, malrotation with volvulus is suggested and an emergency upper gastrointestinal (GI) series should be performed.
If the amount of distended loops of bowel is large, suggesting more of a distal bowel obstruction, but a midgut volvulus cannot be ruled out, a carefully combined upper and lower GI series may need to be performed in co-ordination with the paediatric radiologist.
Result
distended stomach and proximal duodenum with paucity of bowel gas seen distally (volvulus or duodenal web); normal x-ray (malrotation without volvulus or volvulus without complete obstruction)
FBC
Test
In cases of malrotation without volvulus, WBC count is normal. It is also typically normal for several hours in cases of patients with volvulus.
If the volvulus exists for a period of time, WBC count may be elevated. If the presentation is delayed the loss of plasma in the intravascular space leads to haemoconcentration.
Result
elevated WBC count; polycythaemia
Investigations to consider
ultrasound
Test
Can be done quickly without contrast or radiation, but if midgut volvulus is a concern, it may be clinically misguided to order an ultrasound.
An ultrasound is more commonly ordered to assess for intussusception if malrotation or midgut volvulus is not the primary consideration. However, when it is ordered to rule out intussusception, or in circumstances where the upper gastrointestinal series is not conclusive, images of the mesenteric vessels may be useful, demonstrating a reversed SMA-SMV relationship or even a "whirlpool" pattern of volvulus.
Result
no flow beyond the proximal superior mesenteric artery ([SMA] volvulus with ischaemia); twirling of the superior mesenteric artery and vein ([SMV] volvulus)
lower gastrointestinal (GI) contrast series
Test
May be ordered in the work-up of newborn patients with stooling difficulty or distal intestinal obstruction.
Malrotation may be recognised by abnormal position of the caecum (present in 85%).[10]
If there is any concern of GI obstruction, the abnormal caecal position should prompt contrast being placed from above.
Rarely, lower GI series may augment the investigation for malrotation if the upper GI series is inconclusive.[10]
Result
abnormal position of the caecum
ABG
Test
When bowel perfusion is compromised from twisting of the mesenteric vessels, lactic acidosis ensues dropping the serum pH with increased anion gap.
Acidosis is non-specific and non-diagnostic. If the diagnosis of volvulus is confirmed with radiological studies, blood gas analysis is important to know the physiological status of the patient and to guide resuscitation.
Result
metabolic acidosis with respiratory alkalosis resulting in profound decrease in partial pressure of carbon dioxide
Use of this content is subject to our disclaimer