History and exam
Key diagnostic factors
common
presence of risk factors
bruxism activities: teeth grinding/clenching, jaw bracing/thrusting
Can occur during sleep or wakefulness. Classic bruxism involves teeth grinding/clenching, but bruxism can also involve masticatory muscle activity without tooth contact.[16]
Bed partners may complain about grinding noises or tapping sounds during sleep. Can give rise to relationship problems and reduced quality of life.
oral parafunctions
Habits such as biting activities (chewing gum, tooth-tapping, nail-biting, object-biting, e.g., pencils), and movements involving soft-tissues (cheek-, lip-, or tongue-biting, grimacing, tongue pushing against teeth, licking lips, tongue protrusion) may be present.[54]
Association of oral parafunctions with bruxism has been reported, especially in children and adolescents, and may suggest an anxious personality that is also associated with awake bruxism.[55][56]
tooth wear
Tooth wear is considered the typical bruxism sign, but is not a reliable diagnostic factor because of the high prevalence of tooth wear in populations of non-bruxing people.[5][Figure caption and citation for the preceding image starts]: Tooth enamel chippings, cracks, and fractures of natural teeth together with attrition, abfraction, and abrasion due to ceramicsFrom the collection of Dr Alessandro Bracci [Citation ends].
Often present as wear facets on canines and incisors in people with bruxism. Findings suggestive of bruxism include tooth wear affecting at least one sextant of the dentition, with enamel reduction to dentine and some loss of crown height.[5]
jaw muscle and/or temporomandibular joint (TMJ) pain
Bruxism can be associated with pain, fatigue, stiffness, and other symptoms in the jaw-closing muscles (masseter and temporalis). If present in patients with sleep bruxism, the pain is often worst upon awakening.[59] Investigations based on self-reported or clinical bruxism diagnosis showed a positive association with TMJ pain, but studies based on more quantitative and specific methods to diagnose bruxism showed much lower association with temporomandibular disorders symptoms in general.[6]
jaw muscle tenderness
Bruxism may sensitise the jaw muscles, making palpation and normal function such as biting or wide jaw opening uncomfortable.[59]
uncommon
jaw muscle hypertrophy
Repeated activation of jaw muscles can lead to a functional hypertrophy, most noticeably of the masseter muscle.[54] Palpation of the increase in jaw muscle volume with maximal voluntary contraction can give an indication of possible hypertrophy.
Other diagnostic factors
common
headache
Bruxism may be associated with temporal headaches. Literature on the topic is scarce and mainly based on observations in children.[60]
tooth soreness and/or hypersensitivity
If the attrition reaches the dentine, the tooth pulp may become more sensitive to cold air or liquids.[54] However, this phenomenon can also be caused by other dental pathologies (e.g., caries).[Figure caption and citation for the preceding image starts]: Bruxism-related attrition reaching the dentine may result in tooth soreness and hypersensitivityFrom the collection of Dr Alessandro Bracci [Citation ends].
People with bruxism may also experience tooth soreness, especially in the morning after prolonged sleep-time clenching.
uncommon
history of temporomandibular disorder (TMD)
dental restorations and/or implant failure
Range in severity from detachment of aesthetic fillings with poor retention, to fractures of composites or ceramics.[54] Chipping of restorations and de-cementation of crowns and bridges may also be observed. For dental implants, bruxism is unlikely to be a risk factor for biological complications (e.g., implant survival, bone loss, gingival attachment loss), but may be a risk factor for mechanical complications (e.g., screw loosening, fractures of restorations).[67][68]
[Figure caption and citation for the preceding image starts]: An example of a fracture of dental implant componentsFrom the collection of Dr Alessandro Bracci; used with permission [Citation ends].
periodontal problems
tooth chippings, cracks, and fractures
Signs of tooth enamel chipping, teeth fractures, or cracks of natural teeth may indicate the presence of bruxism activities. In particular, tooth enamel chippings may be clinically relevant when occurring on multiple teeth.[Figure caption and citation for the preceding image starts]: Tooth enamel chippingsFrom the collection of Dr Alessandro Bracci [Citation ends].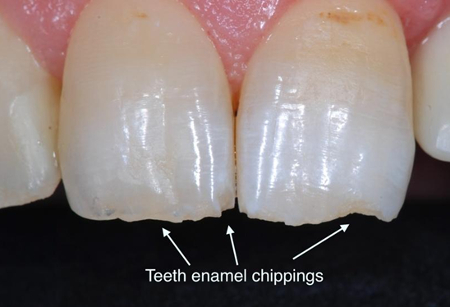 [Figure caption and citation for the preceding image starts]: Tooth fractureFrom the collection of Prof Daniele Manfredini [Citation ends].
[Figure caption and citation for the preceding image starts]: Tooth fractureFrom the collection of Prof Daniele Manfredini [Citation ends].
oral mucosal changes
Bruxism and related oral parafunctions can lead to linea alba, indentations and/or traumatic lesions on the tongue or cheek, or unusual keratinisation of the lip.[54][Figure caption and citation for the preceding image starts]: Linea alba (white line) is a hyperkeratosis of the oral mucosa in the cheeks, representing a dental impression on the inside surface of the cheekFrom the collection of Prof Daniele Manfredini [Citation ends].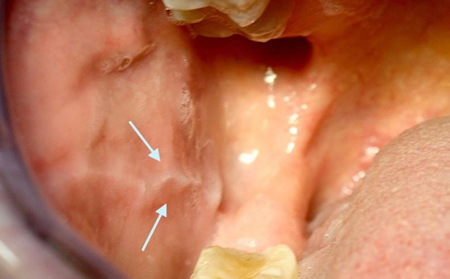 [Figure caption and citation for the preceding image starts]: Tongue scallopingFrom the collection of Dr Alessandro Bracci [Citation ends].
[Figure caption and citation for the preceding image starts]: Tongue scallopingFrom the collection of Dr Alessandro Bracci [Citation ends].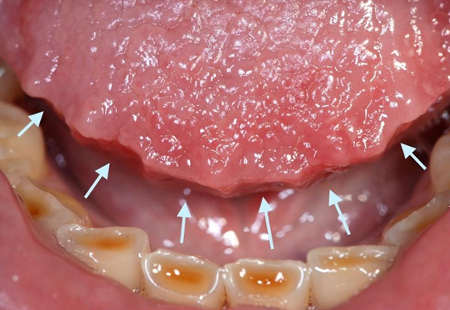
Risk factors
strong
smoking, caffeine, alcohol consumption
All of these factors exacerbate sleep bruxism (SB), although the specific mechanisms are unclear.[34][35]
Smoking as a risk factor suggests that nicotinic receptors are involved, possibly through an effect on the cholinergic system and impact on vigilance and brain-arousal networks. There is also the hypothesis that smoking habits are linked to stress and personality traits which may be the true risk factor for bruxism.
One systematic review found that smoking showed a moderate association with SB.[35] A higher association was noted in current smokers (Odds ratio [OR] 2.8, 95% confidence interval [CI] 2.2 to 3.5), and a weaker association in patients smoking ≤20 cigarettes per day (OR 1.3, 95% CI 1.1 to 1.5). A moderate association was reported for alcohol intake (OR 1.9, 95% CI 1.2 to 2.8). In comparison, caffeine was noted to have a weaker association with SB (OR 1.4, 95% CI 1.2 to 1.8).
stress sensitivity and anxious personality traits
A literature review concluded that awake bruxism is associated with psychosocial factors and psychopathology such as stress and anxiety.[21] A possible explanation of this correlation is that individuals with certain psychological profiles may try to release emotional tension by engaging in bruxism activities.
snoring, obstructive sleep apnoea, and other sleep disorders
Obstructive sleep apnoea (OSA) and snoring have been indicated as risk factors for sleep bruxism (SB).[36][37] One systematic review found that SB was moderately associated with snoring (Odds ratio [OR] 2.6, 95% CI 1.5 to 4.4) and OSA (OR 1.8, 95% CI 1.2 to 2.6).[35]
Apnoeic events may be part of a cascade of events that result in a bruxism-like jaw movement in an attempt to put the mandible forward and restore upper airway patency, even if evidence is lacking about the actual prevalence of this kind of relationship within the full spectrum of individuals with SB and apnoea.[38]
Other sleep disorders may be associated with SB as part of complex central nervous system phenomena occurring during sleep.[39]
medication and illicit drug use
weak
genetic predisposition
Twin studies and analyses of familial distribution indicate a genetic determinant in sleep bruxism.[43] Bruxism may sometimes persist from childhood into adulthood.[44] However, because bruxism is a complex motor behaviour, it is unlikely to be explained by a single gene expression, and genetic-environmental interaction is likely involved.[27]
Use of this content is subject to our disclaimer