Approach
Acute conjunctivitis clinically presents with a red eye and discharge without significant pain, light sensitivity, or visual loss. It is often difficult to clinically differentiate allergic, viral, and bacterial conjunctivitis, because there is often a significant overlap in the presenting symptoms.
Once the conjunctivitis is thought to be infectious, the rapid adenovirus immunoassay should be considered to identify the possibility of adenoviral conjunctivitis, which is the most common cause of acute conjunctivitis.[49]
Allergic conjunctivitis
All forms of allergic conjunctivitis are bilateral. The condition is usually associated with a watery or ropy mucoid discharge, and itching must be present as the primary complaint to make the diagnosis.[8] Mild-to-moderate disease typically has a swollen conjunctiva (chemosis) with a mild papillary conjunctival reaction with scant mucoid discharge. More severe cases have large ('giant') papillae on the palpebral conjunctiva, limbal follicles, and a shield (sterile) corneal ulcer. Allergic conjunctivitis is most commonly seasonal or perennial and often associated with patients with a history of atopic dermatitis, hay fever, and/or asthma.[8]
Atopic conjunctivitis is a type of allergic conjunctivitis that usually occurs in adults and is associated with atopic dermatitis of the eyelids. Vernal conjunctivitis typically affects young males; prevalence is greatest in hot, dry climates.[13][43][44] Vernal conjunctivitis is aggressive and may be associated with shield corneal ulcers. Atopic and vernal conjunctivitis are both associated with a higher incidence of keratoconus - a progressive thinning of the cornea.[1][13] Atopic and vernal conjunctivitis are both rare compared with seasonal and perennial conjunctivitis, with the seasonal and perennial forms representing 98% of patients with ocular allergy.[8]
Seasonal/perennial allergic conjunctivitis is an acute disorder with a recurrent course, whereas atopic and vernal conjunctivitis are chronic diseases with acute exacerbations.[1][8]
Bacterial conjunctivitis, acute (non-gonococcal)
Acute bacterial conjunctivitis can be bilateral or unilateral. Unilateral symptoms and signs are more common in bacterial than viral infection.[18][19][20][42] Patients usually complain of a red eye associated with burning or foreign body sensation. Itching is uncommon. Acute bacterial conjunctivitis is associated with a papillary conjunctival reaction, eyelid matting, and purulent discharge. There is no pre-auricular lymphadenopathy, as there is with hyperacute bacterial conjunctivitis. Bacterial conjunctivitis may be associated with concurrent bacterial otitis media, sinusitis, or pharyngitis.[1] The most common bacterial pathogens in infective conjunctivitis include Pneumococcus, Staphylococcus aureus, Moraxella catarrhalis, and Haemophilus influenzae.[18][19][20][Figure caption and citation for the preceding image starts]: Bacterial conjunctivitisFrom the collection of Mr Hugh Harris; used with permission [Citation ends].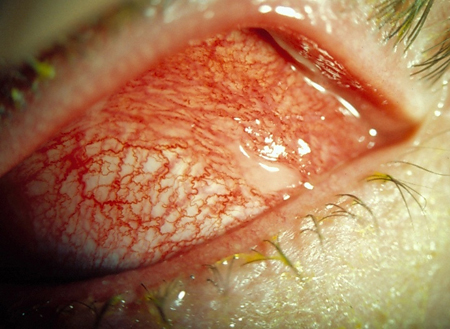
Bacterial conjunctivitis, hyperacute (gonococcal)
Hyperacute bacterial conjunctivitis is likely to be caused by Neisseria gonorrhoeae. This is associated with copious, purulent discharge, eyelid swelling, and chemosis (swelling of the conjunctiva) that develops over 12 to 24 hours. There may also be peripheral corneal ulcers, which may lead to corneal perforation. Typically, the patient is a sexually active young adult; pre-auricular lymphadenopathy may be present. A Gram stain for diplococci is the key differentiating feature. If a child has this condition, then sexual abuse should be ruled out.[1][Figure caption and citation for the preceding image starts]: Gonococcal conjunctivitisCDC Image Library/Joe Miller; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Gonococcal conjunctivitis: resulted in partial blindnessCDC Image Library; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Gonococcal conjunctivitis: resulted in partial blindnessCDC Image Library; used with permission [Citation ends].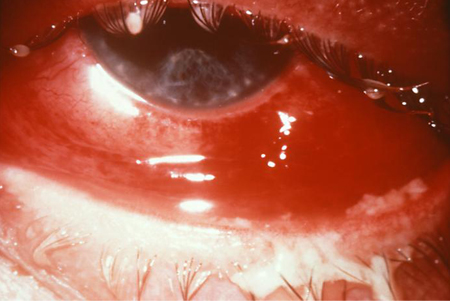
Bacterial conjunctivitis, chlamydial
Chlamydial conjunctivitis is sexually transmitted and typically found in sexually active young adults. If a child has this condition, then sexual abuse should be ruled out.[1]
Patients usually have stringy or mucous discharge, conjunctival follicles, and corneal pannus and may have corneal infiltrates. Pre-auricular lymphadenopathy is commonly present. This form often develops into chronic conjunctivitis. Approximately 70% of patients with confirmed ocular chlamydia also have urogenital chlamydia disease and should be referred for a work-up. Consider co-infection with gonorrhoea.[1]
Chlamydial conjunctivitis that occurs in developed countries is also known as 'inclusion conjunctivitis'. It is caused by Chlamydia trachomatis serotypes D to K and is transmitted sexually. Chlamydial conjunctivitis caused by C trachomatis serotypes A, B, and C is known as trachoma and is mainly limited to areas without adequate access to clean water and sanitation.[1] See Trachoma.
Viral conjunctivitis
Viral conjunctivitis is most commonly caused by an adenovirus.[24][50] Adenoviral conjunctivitis usually starts abruptly in one eye and spreads to the other several days later. It is frequently associated with exposure to an infected person or recent upper respiratory tract symptoms. Patients complain of a red eye with itching, burning, or a foreign body sensation that is associated with a watery to mucous discharge and pre-auricular lymphadenopathy. Corneal subepithelial infiltrates may be present. Herpes conjunctivitis (herpes simplex virus or varicella zoster virus) is usually unilateral and presents with eyelid vesicles, but it may present in an indistinguishable manner from adenovirus. Molluscum contagiosum is another viral cause, presenting mainly in older children and young adults; an immunocompromised state may be a risk factor for molluscum contagiosum.[1][Figure caption and citation for the preceding image starts]: Viral conjunctivitisFrom the collection of Robert Sambursky, MD; used with permission [Citation ends].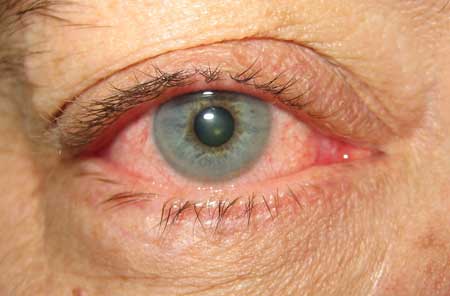
Laboratory evaluation
If infectious conjunctivitis is suspected, the rapid adenovirus immunoassay should be considered to identify adenoviral conjunctivitis (the most common cause of acute conjunctivitis).[51][52][53] Sensitivity is between 85% and 93%, and specificity is between 94% and 99%.[49][54] The positive predictive and negative predictive values for this test are 82.4% and 96.3%, respectively.[54] As patients with adenovirus require more time away from work or school, correct and efficient diagnosis (made possible with the rapid adenovirus immunoassay) can limit the use of unnecessary antibiotics and reduce the spread of disease.
Other laboratory tests include polymerase chain reaction (PCR) and cell culture, but most patients are not routinely sent for these studies, because of the length of time required to obtain a result.[55][56] The use of these tests should be considered for chronic forms of infectious conjunctivitis to confirm the pathogen.
Cell culture is the most accurate and reliable test, but it may take up to 3 weeks for a result of a virus. PCR is used mostly for investigational purposes.[57]
Conjunctival cultures and smears for cytology and special stains (e.g., Gram, Giemsa) should be performed in all neonates with suspected infectious conjunctivitis.[1]
Hyperacute conjunctivitis necessitates a Gram stain to identify gram-negative diplococci and cell culture (chocolate agar) to rule out N gonorrhoeae.[22] Suspected chlamydial conjunctivitis may be confirmed with laboratory testing, such as PCR or cell culture.[1][58]
Allergy skin testing and measuring tear immunoglobulin E levels may be useful in more severe allergic conjunctivitis. Allergy skin testing may identify specific allergens to target with immunosuppression, while tear immunoglobulin E levels may help to diagnose allergic conjunctivitis and assess its severity.[1]
Non-infectious conjunctivitis
Non-infectious conjunctivitis can usually be diagnosed based on the patient's history. Direct chemical exposure to the eye can indicate toxic/chemical conjunctivitis. In cases of suspected chemical splash injury, ocular pH should be tested and eye irrigation continued until pH is 7. Conjunctivitis can be caused from contact lens use or mechanical irritation from the eyelid. Floppy eyelid syndrome, which is associated with obesity and sleep apnoea, may lead to chronic upper lid inversion and mechanical trauma when sleeping. The use of certain topical and systemic medications, such as topical glaucoma medications, antibiotics, antivirals, oral antihistamine, or anticholinergic drugs may irritate the eye and lead to conjunctivitis.[1]
Neoplastic conjunctivitis is caused by a sebaceous gland carcinoma; secondary radiotherapy may also induce a chronic conjunctivitis. It may also be caused by ocular surface squamous neoplasia and melanoma. With a sebaceous gland carcinoma, there may be a hard, nodular, non-mobile mass on the tarsal plate. With ocular surface squamous neoplasia and melanoma, there may be a history of ultraviolet light exposure. With ocular surface squamous neoplasia, there may be a history of human papillomavirus (HPV) infection.[1]
Consultant referral
The following may indicate a more serious condition, and referral to an eye consultant should be considered: history of trauma, rheumatoid disease, contact lens use, significant pain, visual loss, light sensitivity, irregular or fixed pupil, afferent pupillary defect, severe purulent discharge, conjunctival scarring, lack of response to treatment, recurrent episodes, history of herpes simplex virus (HSV) conjunctivitis, history of immunocompromise or corneal involvement (e.g white spot on the cornea).[1][54]
The American Academy of Ophthalmology supports the prompt and appropriate referral of individuals to an ophthalmologist when they present with visual impairment, including that due to inflammation of the lids or conjunctiva, with or without discharge.[59]
Use of this content is subject to our disclaimer