Aetiology
Obstetric causes can be divided into those in early and late pregnancy. Conditions that span the entire gestation period have been categorised according to their anatomical system. For simplicity, only conditions that more commonly occur ante-partum (before labour commences), rather than intra- or postpartum, have been included.
Early pregnancy
Ectopic pregnancy
Usually diagnosed in the first trimester, most commonly affecting the fallopian tube[4]
Strongly associated with conditions that damage the fallopian tube, such as pelvic inflammatory disease (PID), previous ectopic pregnancy, and previous tubal surgery
Also associated with current IUD users and women whose pregnancy is the result of assisted reproductive technologies.
Miscarriage
Usually occurs before the 12th week, with approximately 50% of all cases of early pregnancy loss due to fetal chromosomal abnormalities[5][6][7][8]
Other causes include multiple pregnancy, uterine pathology (e.g., fibroids), cytotoxic drugs, radiation, and systemic conditions (e.g., anti-phospholipid syndrome).
Ovarian hyper-stimulation syndrome (OHSS)
At least 2% of pregnancies in industrialised countries are consequent to advanced fertility treatment such as in vitro fertilisation
The most life-threatening iatrogenic complication, occurring in 2% of women undergoing gonadotrophin stimulation
Risk highest in young women with polycystic ovary syndrome or low BMI
Severe form (0.2%) characterised by enlarged ovaries, ascites, increased blood viscosity, and renal or hepatic dysfunction.[9]
Late pregnancy
Pre-term labour
May be triggered by nephrolithiasis, urinary tract infections (UTIs) (particularly pyelonephritis), haemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome, placental abruption (implicated in up to 10% of premature deliveries), chorioamnionitis, and appendicitis[10]
Acute cystitis may irritate the uterine segment and trigger uterine contractions
More likely to occur with non-operative management of cholecystitis compared with those undergoing cholecystectomy.[11]
Chorioamnionitis
Complicates 1% to 5% of full-term pregnancies and is seen in about 25% of pre-term deliveries[12]
Associated organisms include Ureaplasma urealyticum, Mycoplasma hominis, Gardnerella vaginalis, Peptostreptococcus, and Bacteroides species
Risk increased following chorionic villus sampling (CVS) and amniocentesis.
Uterine rupture
High risk in patients who have had previous uterine surgery (e.g., myomectomy).[13]
Placental abruption
Risk factors include maternal age ≥35 years, multi-parity, cigarette smoking, cocaine and other drug use, multiple gestation, chronic hypertension, mild and severe pre-eclampsia, premature rupture of membranes, oligohydramnios, and chorioamnionitis.[14]
Haemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome
Characterised by haemolytic anaemia, elevated liver enzymes, and thrombocytopenia
Given its progressive nature, can be considered a variant of pre-eclampsia.[15]
Acute fatty liver of pregnancy
Rare but life-threatening condition characterised by micro-vesicular fatty infiltration of the liver
Most commonly occurs in the third trimester.
Gynaecological
Adnexal masses
Encountered in 8.8% of pregnant women and mostly resolve by the second trimester[16][17]
Pelvic masses should be considered cancerous until proved otherwise
Persistent masses (that have not resolved by the second trimester) are at risk of malignancy and have an occurrence of 2% to 3% during pregnancy[18]
Adnexal masses causing abdominal pain (torsion, haemorrhage, and rupture) more likely to present in the first trimester
About 20% of adnexal torsions occur during pregnancy, are common in the right adnexa, and predominantly affect teenagers and young women. Torsions are often associated with an increased weight of the adnexa due to the presence of masses that are usually >5 cm
Ovarian cyst rupture is rare and may occur in conjunction with torsion
Massive haemorrhage into an ovarian cyst (particularly a malignant cyst) occurs infrequently and causes pain similar to that of torsion
Haemorrhage may also result in a corpus luteum cyst. At the time of formation of the corpus luteum, there is always a little bleeding into the follicle that has discharged its ovum. If the bleeding is excessive, the corpus luteum becomes distended with blood. Cysts vary in size from 2.5 to 10 cm.
Fibroids
Occur in approximately 20% to 30% of women of reproductive age
Most growth happens in early pregnancy
Cause pain in pregnancy mainly because of red degeneration (necrobiosis), which occurs in 5% to 10% of pregnancies between 12 and 20 weeks' gestation[19]
Pain may also result from torsion of a pedunculated fibroid or from fibroid impaction.
Urological
Urological conditions in pregnancy present a major diagnostic challenge, as the urinary tract undergoes profound anatomical and physiological changes that predispose pregnant women to an increased risk for symptomatic UTIs and kidney stone formation. The ureters become dilated as early as the first trimester and remain distended until after delivery. This is mainly due to compression exerted by the growing uterus on the collecting system above the level of the linea terminalis. This leads to vascular congestion of the upper urinary tract, with consequent urinary stasis. These changes can facilitate aggregation of crystals in the urine and increase the risk of ascending infection. The following conditions may subsequently occur:
UTIs
Most frequently Escherichia coli (80% to 90% of UTIs during pregnancy)
Other gram-negative rods isolated: Proteus mirabilis, Klebsiella pneumonia
Incidence increases with low socio-economic status, increasing age, sexual activity, and diabetes mellitus.
Acute pyelonephritis
Most common during the second half of pregnancy, as a result of increased ureteral obstruction and urinary stasis[20]
Usually uni-lateral and more common in the right kidney
E coli is the predominant organism.
Nephrolithiasis
Usually occurs during the second and third trimesters
Three times more likely in multi-parous women
Ureteric stones more common than kidney stones.[21]
Hydronephrosis
Common physiological condition in pregnancy; disappears rapidly after birth[22]
Most commonly (90%) occurs after the 20th week of gestation, being more pronounced in primigravidae
Dilatation only seen above the linea terminalis and is more frequently right sided
Compression of the ureters by the uterus (causing hydronephrosis) can result in acute attacks of pain triggered by ureteral obstruction.
Gastrointestinal
A number of common gastrointestinal (GI) conditions can complicate pregnancy and present with abdominal pain. In turn, pregnancy can make the diagnosis of these conditions difficult due to the physiological changes occurring to the body during this time.
Appendicitis
Acute appendicitis occurs approximately at a rate of 1:1250 to 1:1500[23]
No single symptom, sign, or laboratory finding is diagnostic for acute appendicitis[24]
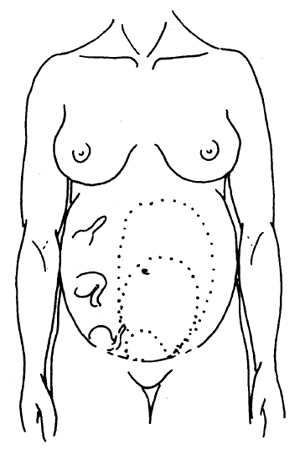
Diagnosis complicated by anatomical changes in the location of the appendix as pregnancy progresses[25]
Clinical judgement vital in deciding whether surgical management is needed.[Figure caption and citation for the preceding image starts]: The site of the appendix changes as pregnancy advancesChamberlain G. ABC of antenatal care: abdominal pain in pregnancy. BMJ. 1991;302:390-1394. Used with permission [Citation ends].
Cholecystitis
Caused by cholelithiasis in >90% of cases in pregnancy[26]
Cholelithiasis risk is increased by progesterone-induced smooth muscle relaxation of the gallbladder (which promotes stasis of the bile) and elevated levels of oestrogens (which increase the lithogenicity of bile).
Pancreatitis
Cholelithiasis and hypertriglyceridaemia may be common causes in pregnancy.[27][28][29]
Tends to occur late in the third trimester, possibly due to increased intra-abdominal pressure on the biliary ducts.[30]
Intestinal obstruction
Incidence increasing with increased frequency of intra-abdominal surgery, pelvic surgery, and PID
Most commonly caused by simple obstruction, mainly as a result of adhesions (60% to 70% of cases) or volvulus (25%)[2]
Rarely caused by intussusception, hernias, and neoplasms.
Traumatic
Traumatic causes of abdominal pain should not be overlooked in pregnant women. Abdominal pain following blunt trauma affects 6% to 7% of pregnancies, 0.3% of which require admission.[31] The most common causes are road traffic accidents, accidental falls, and physical abuse. Splenic rupture may be due to domestic violence.[32]
Musculoskeletal
Although uncommon, a rectus sheath haematoma can be the cause of abdominal pain in pregnancy. Trauma, obesity, straining, coughing, previous abdominal surgery, vascular pathologies, disorders of coagulation, endometriosis of the rectus sheath, Cushing's syndrome, and anticoagulation therapy may contribute to the occurrence of this condition.[33]
Use of this content is subject to our disclaimer