The management of familial adenomatous polyposis (FAP) is guided by colonoscopic surveillance and the presence of adenomas.
Prophylactic proctocolectomy is the main means for preventing colorectal cancer in FAP.
Surveillance colonoscopy
Patients with a family history of FAP/attenuated FAP (AFAP) who are adenomatous polyposis coli (APC)-positive should undergo surveillance colonoscopy to identify and/or monitor colonic adenomas.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[24]Hyer W, Cohen S, Attard T, et al. Management of familial adenomatous polyposis in children and adolescents: Position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):428-41.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Familial_Adenomatous_Polyposis_in.30.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585891?tool=bestpractice.com
[30]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034349
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
[38]Issaka RB, Chan AT, Gupta S. AGA clinical practice update on risk stratification for colorectal cancer screening and post-polypectomy surveillance: expert review. Gastroenterology. 2023 Nov;165(5):1280-91.
https://www.gastrojournal.org/article/S0016-5085(23)04771-6/fulltext?referrer=https%3A%2F%2Fpubmed.ncbi.nlm.nih.gov%2F
http://www.ncbi.nlm.nih.gov/pubmed/37737817?tool=bestpractice.com
For patients with FAP, the National Comprehensive Cancer Network (NCCN) advises that colonoscopy should be offered starting from ages 10 to 15 years. Other guidance, including from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition, recommend that this surveillance can begin slightly later, from age 12 years onwards.[24]Hyer W, Cohen S, Attard T, et al. Management of familial adenomatous polyposis in children and adolescents: Position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):428-41.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Familial_Adenomatous_Polyposis_in.30.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585891?tool=bestpractice.com
[30]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034349
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
For patients with AFAP, colonoscopic surveillance should begin in the late teens, and generally no later than 20 years age.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
Frequency of colonic surveillance is individualised depending on colonic phenotype and is typically undertaken between every 1 and 3 years.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[24]Hyer W, Cohen S, Attard T, et al. Management of familial adenomatous polyposis in children and adolescents: Position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):428-41.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Familial_Adenomatous_Polyposis_in.30.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585891?tool=bestpractice.com
[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
The presence of alarm symptoms such as anaemia, rectal bleeding, increased bowel movements, and mucous discharge should prompt urgent colonoscopy for any patient, regardless of age or colonic phenotype.[24]Hyer W, Cohen S, Attard T, et al. Management of familial adenomatous polyposis in children and adolescents: Position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):428-41.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Familial_Adenomatous_Polyposis_in.30.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585891?tool=bestpractice.com
[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
There is no single consensus for the absolute or relative indications for surgery. In patients with FAP, surgery is generally recommended following detection of colonic adenomas, but timing must be individualised and depends on the distribution, size, and histology of colorectal polyps.[24]Hyer W, Cohen S, Attard T, et al. Management of familial adenomatous polyposis in children and adolescents: Position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr. 2019 Mar;68(3):428-41.
https://journals.lww.com/jpgn/Fulltext/2019/03000/Management_of_Familial_Adenomatous_Polyposis_in.30.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30585891?tool=bestpractice.com
[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
In cases of AFAP, surgery is largely guided by adenoma burden than adenoma presence.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
The American College of Gastroenterologists advise absolute indications for immediate colorectal surgery in patients with FAP, or attenuated FAP, include:[29]Syngal S, Brand RE, Church JM, et al.; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
Documented or suspected colorectal cancer
Significant symptoms related to colonic neoplasia (e.g., gastrointestinal bleeding)
These indications are also supported by the British Association of Gastroenterology and the Association of Coloproctology of Great Britain and Ireland.[30]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034349
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
Relative indications for surgery include:[29]Syngal S, Brand RE, Church JM, et al.; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
Presence of multiple adenomas >6 mm
Significant increase in adenoma number
Presence of adenoma with high-grade dysplasia
Inability to adequately survey the colon due to multiple diminutive polyps
The European Hereditary Tumor Group (EHTG) and European Society of Coloproctology (ESCP) recommend, for patients with FAP, indications for immediate colorectal surgery include:[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
Certain or suspected cancer
Severe symptoms from polyposis
Severe disease (>1000 polyps identified at colonoscopy)
Unfavourable histological features (e.g., villous adenoma)
Indications for planned surgery include:[37]Zaffaroni G, Mannucci A, Koskenvuo L, et al. Updated European guidelines for clinical management of familial adenomatous polyposis (FAP), MUTYH-associated polyposis (MAP), gastric adenocarcinoma, proximal polyposis of the stomach (GAPPS) and other rare adenomatous polyposis syndromes: a joint EHTG-ESCP revision. Br J Surg. 2024 May 3;111(5):znae070.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11081080
http://www.ncbi.nlm.nih.gov/pubmed/38722804?tool=bestpractice.com
Polyp >10 mm in diameter
Favourable histology features
Substantial increase in polyp number between examinations
Sparse disease (100-1000 polyps)
Surgery for FAP
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred surgery for most patients with FAP because it prevents rectal cancers.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
However, some patients may require (or choose) total abdominal colectomy with ileorectal anastomosis (IRA), or total proctocolectomy with permanent end ileostomy.
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA)
This procedure is offered to patients with classical FAP, patients with attenuated FAP with numerous polyps resulting in carpeting of the rectum, those with curable rectal cancer complicating the polyposis, and those who have previously undergone IRA and now have an unstable rectum in terms of polyp number, size, or histology. The procedure is usually not offered to patients with incurable cancer, those with an intra-abdominal desmoid that may interfere with the completion of surgery, those with anatomical, physiological, or pathological contraindications to an IPAA, or where there is concern regarding the ability of patients to participate in close endoscopic surveillance following surgery.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
The advantages of total proctocolectomy with IPAA are that the risk of developing rectal cancer is negligible and a permanent stoma is not needed. The disadvantages are that it is a complex operation, a temporary stoma is usually needed, and there is a small risk of bladder or sexual dysfunction, and anal sphincter injury. Bowel function, although usually reasonable, is also somewhat unpredictable. The ileal pouch requires surveillance, and the area of the IPAA should still be examined due to the fact that residual anal transitional zone mucosa may remain.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Mucosectomy to maximise removal of rectal mucosa may be considered in IPAA.[39]Chambers WM, McC Mortensen NJ. Should ileal pouch-anal anastomosis include mucosectomy? Colorectal Dis. 2007;9:384-392.
http://www.ncbi.nlm.nih.gov/pubmed/17504334?tool=bestpractice.com
Hand-sewn or stapled IPAA techniques may be used. Hand-sewn IPAA involves the removal of all colorectal mucosa, and is therefore associated with decreased risk for polyps occurring post-operatively in the anal transitional zone, compared with stapled anastomosis. It may be the preferred technique for IPAA for selected patients with FAP.[40]Bjork JA, Akerbrant HI, Iselius LE, et al. Risk factors for rectal cancer morbidity and mortality in patients with familial adenomatous polyposis after colectomy and ileorectal anastomosis. Dis Colon Rectum. 2000;43:1719-1725.
http://www.ncbi.nlm.nih.gov/pubmed/11156457?tool=bestpractice.com
This would include patients with polyps in the transitional zone that may be difficult to clear without mucosectomy. Retrospective data from a large, prospective, institutional genetic registry of patients with FAP showed that although stapled IPAA has a higher incidence of anal transitional zone polyps requiring treatment, compared with hand-sewn IPAA, the incidence of anal transitional zone adenocarcinoma was similar between the two groups.[41]Ozdemir Y, Kalady MF, Aytac E, et al. Anal transitional zone neoplasia in patients with familial adenomatous polyposis after restorative proctocolectomy and IPAA: incidence, management, and oncologic and functional outcomes. Dis Colon Rectum. 2013;56:808-814.
http://www.ncbi.nlm.nih.gov/pubmed/23739186?tool=bestpractice.com
The stapled anastomosis is associated with better long-term bowel function than a hand-sewn anastomosis. It is therefore the preferred technique for the surgical management of patients with FAP in some centres.[41]Ozdemir Y, Kalady MF, Aytac E, et al. Anal transitional zone neoplasia in patients with familial adenomatous polyposis after restorative proctocolectomy and IPAA: incidence, management, and oncologic and functional outcomes. Dis Colon Rectum. 2013;56:808-814.
http://www.ncbi.nlm.nih.gov/pubmed/23739186?tool=bestpractice.com
There is evidence that laparoscopic IPAA is a feasible and safe procedure, although large, good-quality trials examining differences between laparoscopic and open approaches in terms of postoperative complications, cosmesis, quality of life, and costs are needed.[42]Xie YQ, Yuan X. Meta analysis of surgical treatment of 231 cases of familial adenomatous polyposis in China. Chin J Cancer Prev Treat. 2008;15:537-540.[43]Ahmed AU, Keus F, Heikens JT, et al. Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Cochrane Database Syst Rev. 2009;(1):CD006267.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006267.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/19160273?tool=bestpractice.com
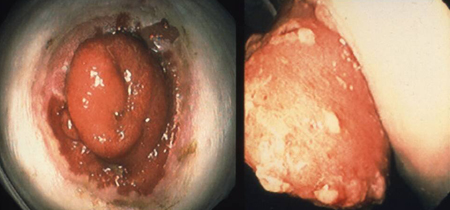
[Figure caption and citation for the preceding image starts]: Brooke ileostomy in familial adenomatous polyposis: adenoma riskFrom the personal collection of Lisa A. Boardman, MD; used with permission [Citation ends].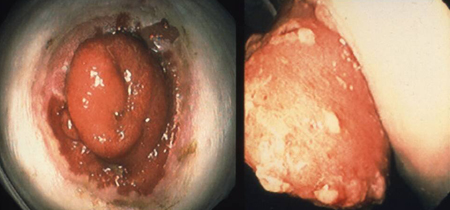
Female patients should be counselled that the IPAA is associated with an increase in infertility.[44]Rajaratnam SG, Eglinton TW, Hider P, et al. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011;26:1365-1374.
http://www.ncbi.nlm.nih.gov/pubmed/21766164?tool=bestpractice.com
For patients who have undergone IPPA, an annual pouchoscopy is necessary for pouch polyp surveillance.[45]Tudyka VN, Clark SK. Surgical treatment in familial adenomatous polyposis. Ann Gastroenterol. 2012;25(3):201-6.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3959379
http://www.ncbi.nlm.nih.gov/pubmed/24714154?tool=bestpractice.com
Total abdominal colectomy with IRA
This is an option for patients with FAP with few or no rectal adenomas.[12]Yang J, Gurudu SR, Koptiuch C, et al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in familial adenomatous polyposis syndromes. Gastrointest Endosc. 2020 May;91(5):963-82.e2.
https://linkinghub.elsevier.com/retrieve/pii/S0016-5107(20)30054-7
http://www.ncbi.nlm.nih.gov/pubmed/32169282?tool=bestpractice.com
[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
Because nearly one quarter of patients with FAP treated with IRA develop rectal cancer in the retained rectal mucosa without follow up, patients who have undergone this procedure require annual proctoscopy.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
In one study, 13% of patients with FAP treated with IRA developed rectal cancer a median of 10 years after surgery.[46]Jenner DC, Levitt S. Rectal cancer following colectomy and ileorectal anastomosis for familial adenomatous polyposis. Aust N Z J Surg. 1998;68:136-138.
http://www.ncbi.nlm.nih.gov/pubmed/9494007?tool=bestpractice.com
The risk of cancer development in the rectal stump rises considerably after age 50 years. If the rectum becomes unstable, a proctectomy with either an IPAA or end ileostomy is recommended.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
The benefits of IPAA versus IRA should be thoroughly discussed with the patient.[44]Rajaratnam SG, Eglinton TW, Hider P, et al. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011;26:1365-1374.
http://www.ncbi.nlm.nih.gov/pubmed/21766164?tool=bestpractice.com
[47]De Cosse JJ, Bulow S, Neale K, et al. Rectal cancer risk in patients treated for familial adenomatous polyposis. Br J Surg. 1992;79:1372-1375.
http://www.ncbi.nlm.nih.gov/pubmed/1336702?tool=bestpractice.com
[48]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2019 Sep;51(9):877-895.
https://www.doi.org/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
Patients who have IRA have better continence and bowel function following surgery, compared with patients having IPAA.[49]Günther K, Braunrieder G, Bittorf BR, et al. Patients with familial adenomatous polyposis experience better bowel function and quality of life after ileorectal anastomosis than after ileoanal pouch. Colorectal Dis. 2003 Jan;5(1):38-44.
http://www.ncbi.nlm.nih.gov/pubmed/12780925?tool=bestpractice.com
Women of childbearing age may choose IRA until after childbearing, when they can convert to IPAA.
IRA conversion to IPAA
In some instances, IRA can be converted to IPAA. This was the case in 8% of patients in a retrospective review of patients with FAP. Aside from an increased risk of wound infection in 9% of those converted to IPAA compared with <1% with IPAA as the first operation, no other significant complications were associated with IPAA following an IRA.[50]Parc Y, Piquard A, Dozois RR, et al. Long-term outcome of familial adenomatous polyposis patients after restorative proctocolectomy. Ann Surg. 2004 Mar;239(3):378-82.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1356236
http://www.ncbi.nlm.nih.gov/pubmed/15075655?tool=bestpractice.com
Proctocolectomy with end ileostomy
This is rarely indicated as a prophylactic procedure because alternative approaches are available that do not involve a permanent stoma. A proctocolectomy with end ileostomy removes all risk for rectal cancer, but is associated with a risk of bladder or sexual dysfunction. It may be offered to patients with a low, locally advanced rectal cancer, patients who cannot have an ileal pouch due to a desmoid tumour, patients with a poorly functioning ileal pouch, patients who have a contraindication to an IPAA (e.g., concomitant Crohn disease, poor sphincter function), and patients in whom there is a concern for participation in close endoscopic surveillance after surgery. Proctocolectomy with continent ileostomy is offered to patients who are motivated to avoid end ileostomy because they are either not suitable for proctocolectomy with IPAA (e.g., patients who have had previous pelvic surgery or who have shortening of the mesentery) or they have a poorly functioning IPAA. This is a complex operation with a significant risk for reoperation.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Management of desmoid tumours
Intra-abdominal desmoid tumours are one of the leading causes of death in patients with FAP.[51]DE Marchis ML, Tonelli F, Quaresmini D, et al. Desmoid tumors in familial adenomatous polyposis. Anticancer Res. 2017 Jul;37(7):3357-3366.
https://www.doi.org/10.21873/anticanres.11702
http://www.ncbi.nlm.nih.gov/pubmed/28668823?tool=bestpractice.com
Desmoid tumours have unpredictable behaviour with poorly understood biology, resulting in a lack of standardised medical and surgical therapies. Management of desmoids is difficult and they often recur in spite of treatment. Patients with FAP and desmoid tumours should be referred to centres specialising in management of desmoid tumours.
Pharmacological therapy is usually the preferred initial approach.[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
Surgery can stimulate intra-abdominal desmoid tumour growth in patients with FAP and is only typically offered to symptomatic patients who do not respond to initial medical therapy.[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
Intra-abdominal desmoid staging systems have been developed to help predict associated mortality. Five-year survival of patients with stage I, II, III, and IV intra-abdominal desmoid tumours was 95%, 100%, 89%, and 76%, respectively (P <0.001). Severe pain, opioid dependence, tumour size larger than 10 cm, and need for total parenteral nutrition were shown to further define survival within stages. The 5-year survival rate of a stage IV patient with all of the above-mentioned risk factors was only 53%.[52]Quintini C, Ward G, Shatnawei A, et al. Mortality of intra-abdominal desmoid tumors in patients with familial adenomatous polyposis: a single center review of 154 patients. Ann Surg. 2012;255:511-516.
http://www.ncbi.nlm.nih.gov/pubmed/22323009?tool=bestpractice.com
Available treatments include cyclo-oxygenase (COX)-2 inhibitors (e.g., celecoxib) or combined COX-1 and COX-2 inhibitors (e.g., sulindac), anti-oestrogens (e.g., tamoxifen), chemotherapy and radiotherapy, and surgery. Imatinib has been associated with both partial response and growth stabilisation, even in desmoids that do not have apparent mutations in the KIT tyrosine kinase oncogene.[53]Duffaud F, Le Cesne A. Imatinib in the treatment of solid tumors. Targ Oncol. 2009;4:45-56.
http://www.ncbi.nlm.nih.gov/pubmed/19343301?tool=bestpractice.com
There are no controlled trials comparing these various modalities of treatment. Complicating our understanding of the impact of these treatments is the phenomenon of spontaneous regression of desmoids, which may occur in up to 10% of cases.[54]Clark SK, Phillips RK. Desmoids in familial adenomatous polyposis. Br J Surg. 1996;83:1494-1504.
http://www.ncbi.nlm.nih.gov/pubmed/9014661?tool=bestpractice.com
[55]Knudsen AL, Bulow S. Desmoid tumour in familial adenomatous polyposis: a review of literature. Fam Cancer. 2001;1:111-119.
http://www.ncbi.nlm.nih.gov/pubmed/14574007?tool=bestpractice.com
Management of duodenal polyps
In more than 90% of patients with FAP, duodenal adenomatous polyposis develops. Upper gastrointestinal tract surveillance with endoscopy is an important aspect of management, as duodenal cancer may develop in up to 10% of patients.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
The Spigelman criteria are used to assess the severity of polyps:[36]Spigelman AD, Williams CB, Talbot IC, et al. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet. 1989 Sep 30;2(8666):783-5.
http://www.ncbi.nlm.nih.gov/pubmed/2571019?tool=bestpractice.com
Duodenal/periampullary polyp number (1-4 = 1 point; 5-20 = 2 points; >20 = 3 points)
Size (1-4 mm = 1 point; 5-10 mm = 2 points; >10 mm = 3 points)
Histology (tubular = 1 point; tubulovillous = 2 points; villous = 3 points)
Degree of dysplasia (low grade = 1 point; high grade = 3 points).
A score of 0 points is classified as stage 0 disease, 1 to 4 points is classified as stage 1 disease, 5 to 6 points is classified as stage 2 disease, 7 to 8 points is classified as stage 3 disease, and 9 to 12 points is classified as stage 4 disease.
At-risk patients found to have colorectal adenomas, as well as known APC gene carriers, should have forward- and side-viewing oesophagogastroduodenoscopies at least every 5 years.
The American Society of Colon and Rectal Surgeons and the National Comprehensive Cancer Network recommend that screening for duodenal adenomas begin at aged 20-25 years, although this may be offered to younger patients if there is a family history of duodenal cancer or significant duodenal polyp burden.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
[30]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034349
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
The American College of Gastroenterologists and the European Society of Medical Oncology advise a later starting age of 25-30 years.[29]Syngal S, Brand RE, Church JM, et al.; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[30]Monahan KJ, Bradshaw N, Dolwani S, et al. Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut. 2020 Mar;69(3):411-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034349
http://www.ncbi.nlm.nih.gov/pubmed/31780574?tool=bestpractice.com
[56]Stjepanovic N, Moreira L, Carneiro F, et al. Hereditary gastrointestinal cancers: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019 Oct 1;30(10):1558-71.
https://www.sciencedirect.com/science/article/pii/S0923753419609774
http://www.ncbi.nlm.nih.gov/pubmed/31378807?tool=bestpractice.com
Endoscopy should be repeated every 4-5 years until polyps are found.[29]Syngal S, Brand RE, Church JM, et al.; American College of Gastroenterology. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62.
http://www.ncbi.nlm.nih.gov/pubmed/25645574?tool=bestpractice.com
[56]Stjepanovic N, Moreira L, Carneiro F, et al. Hereditary gastrointestinal cancers: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019 Oct 1;30(10):1558-71.
https://www.sciencedirect.com/science/article/pii/S0923753419609774
http://www.ncbi.nlm.nih.gov/pubmed/31378807?tool=bestpractice.com
Once polyps develop, the Spigelman criteria can be used to determine the appropriate surveillance intervals:[36]Spigelman AD, Williams CB, Talbot IC, et al. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet. 1989 Sep 30;2(8666):783-5.
http://www.ncbi.nlm.nih.gov/pubmed/2571019?tool=bestpractice.com
Stage 0: 3-5 years
Stage 1: 2-3 years
Stage 2: 1-2 years
Stage 3: 6-12 months
Stage 4: surveillance should occur every 3-6 months along with surgical consultation for consideration of duodenectomy.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Patients with advanced polyposis should be referred to expert centres to be managed by endoscopists with expertise in FAP.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Endoscopic treatment is used for downstaging, with the aim of delaying the development of stage 4 disease. Endoscopic therapies for duodenal adenomas include polypectomy, endoscopic mucosal resection, and ablation.[12]Yang J, Gurudu SR, Koptiuch C, et al. American Society for Gastrointestinal Endoscopy guideline on the role of endoscopy in familial adenomatous polyposis syndromes. Gastrointest Endosc. 2020 May;91(5):963-82.e2.
https://linkinghub.elsevier.com/retrieve/pii/S0016-5107(20)30054-7
http://www.ncbi.nlm.nih.gov/pubmed/32169282?tool=bestpractice.com
There is insufficient evidence for the benefit of chemoprevention in the management of duodenal polyps. Patients should be referred to expert centres for consideration of enrolment in a clinical trial if they are interested in chemoprevention. There are currently no approved drugs for the prevention or regression of duodenal adenomas.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Management of attenuated FAP
Frequent colonoscopic adenoma clearance may be suitable for patients with a low polyp burden.[40]Bjork JA, Akerbrant HI, Iselius LE, et al. Risk factors for rectal cancer morbidity and mortality in patients with familial adenomatous polyposis after colectomy and ileorectal anastomosis. Dis Colon Rectum. 2000;43:1719-1725.
http://www.ncbi.nlm.nih.gov/pubmed/11156457?tool=bestpractice.com
[48]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2019 Sep;51(9):877-895.
https://www.doi.org/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
[57]Nugent KP, Phillips RK. Rectal cancer risk in older patients with familial adenomatous polyposis and an ileorectal anastomosis: a cause for concern. Br J Surg. 1992;79:1204-1206.
http://www.ncbi.nlm.nih.gov/pubmed/1334761?tool=bestpractice.com
[58]Parc YR, Olschwang S, Desaint B, et al. Familial adenomatous polyposis: prevalence of adenomas in the ileal pouch after restorative proctocolectomy. Ann Surg. 2001 Mar;233(3):360-4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421251
http://www.ncbi.nlm.nih.gov/pubmed/11224623?tool=bestpractice.com
[59]van Duijvendijk P, Vasen HF, Bertario L, et al. Cumulative risk of developing polyps or malignancy at the ileal pouch-anal anastomosis in patients with familial adenomatous polyposis. J Gastrointest Surg. 1999;3:325-330.
http://www.ncbi.nlm.nih.gov/pubmed/10481126?tool=bestpractice.com
This is generally defined as having >20 adenomas (all <1 cm in diameter) with no advanced histology.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Where adenoma burden cannot be managed endoscopically, surgery should be offered. This is typically when polyp burden is >20 (at any individual examination), polyps have been previously ablated, some polyps are >1 cm in size, or advanced histology is noted in any polyp.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
Choice of surgery in attenuated FAP is individualised based on the age of the patient, their previous surgical history, location of polyps, and patient preferences.[48]van Leerdam ME, Roos VH, van Hooft JE, et al. Endoscopic management of polyposis syndromes: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2019 Sep;51(9):877-895.
https://www.doi.org/10.1055/a-0965-0605
http://www.ncbi.nlm.nih.gov/pubmed/31342472?tool=bestpractice.com
In most cases, rectal adenomas are few, therefore colectomy with an IRA and continuous, lifelong surveillance of the rectum is the management of choice.
Chemoprevention
Chemoprevention may be considered as an adjunct in the management of retained rectum or ileal pouch in select patients with FAP/AFAP following prophylactic surgery.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[28]Poylin VY, Shaffer VO, Felder SI, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the management of inherited adenomatous polyposis syndromes. Dis Colon Rectum. 2024 Feb 1;67(2):213-27.
https://journals.lww.com/dcrjournal/fulltext/2024/02000/the_american_society_of_colon_and_rectal_surgeons.6.aspx
http://www.ncbi.nlm.nih.gov/pubmed/37682806?tool=bestpractice.com
Available data suggest that sulindac is the most potent drug for polyp regression; however, it is not yet known whether decreases in polyp burden reduces colorectal cancer risk.[9]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal, endometrial, and gastric [internet publication].
https://www.nccn.org/guidelines/category_2
[60]Cruz-Correa M, Hylind LM, Romans KE, et al. Long-term treatment with sulindac in familial adenomatous polyposis: a prospective cohort study. Gastroenterology. 2002 Mar;122(3):641-5.
https://www.doi.org/10.1053/gast.2002.31890
http://www.ncbi.nlm.nih.gov/pubmed/11874996?tool=bestpractice.com
Patients should be referred to expert centres for consideration of enrolment in a clinical trial if they are interested in chemoprevention. There are currently no approved drugs for this indication.