Differentials
Common
Idiopathic ulcerative proctitis
History
diarrhoea with small, frequent stools and mucus, although constipation may develop due to rectal fibrosis; bleeding usually associated with discomfort, tenesmus, or diarrhoea; urgency; nocturnal diarrhoea; occasionally faecal incontinence[21]
Exam
no differentiating examination findings
1st investigation
- sigmoidoscopy:
continuous inflammation with or without ulceration from rectum proximally
More
Crohn's proctitis
History
similar symptoms to ulcerative proctitis (e.g., rectal bleeding, urgency, diarrhoea); involvement of other parts of the colon or small bowel can cause abdominal pain and fevers; diagnosis of disease may already be known
Exam
perianal disease may cause fistulae, abscesses, or fissures; right lower quadrant pain if associated with ileitis[19]
1st investigation
- colonoscopy:
patchy areas of inflammation and/or ulceration, although rectum is usually spared in Crohn's disease
More
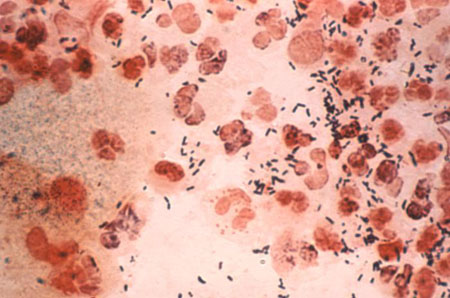
Sexually transmitted proctitis
History
anal-receptive sex with or without immunosuppression (e.g., HIV), rectal discharge, severe anal pain, malaise
Exam
systemic fever, lymphadenopathy (lymphogranuloma venereum caused by Chlamydia trachomatis), anal discharge
1st investigation
- rectal swab for microscopy, Gram stain, and culture, nucleic acid amplification tests (NAAT):
Neisseria gonorrhoeae, Chlamydia trachomatis, Herpes simplex, Treponema pallidum
More
Other investigations
- sigmoidoscopy:
patchy inflammation and/or ulceration, may look like ulcerative colitis
- syphilis serology (rapid plasma reagin, Venereal Disease Research Laboratory, fluorescent treponemal antibody-absorption tests):
positive
- biopsy:
Treponema pallidum, Chlamydia trachomatis, Herpes simplex, cytomegalovirus
More - HIV test:
may be positive
- lymphogranuloma venereum (LGV) genotyping:
may be positive
More
Uncommon
Coeliac disease
History
reported primarily in children; presents with diarrhoea or steatorrhoea, fatigue, abdominal pain, weight loss; diagnosis of disease may already be known[9]
Exam
pallor, easy bruising, aphthous stomatitis
1st investigation
Other investigations
- rectal biopsy:
crypt distortion with forked glands, crypt atrophy, and general crypt epithelial polymorphs
More - small bowel biopsy:
villous atrophy, increased intra-epithelial lymphocytes
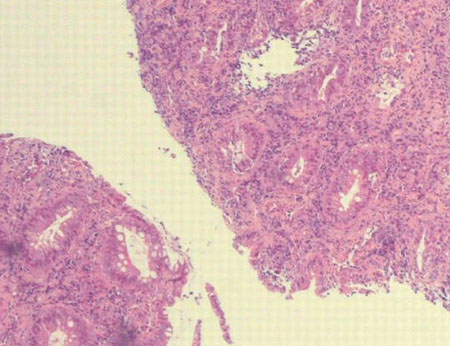
Radiation proctitis
History
rectal bleeding after radiotherapy; acute proctitis occurs within 3 months of therapy and usually ceases once treatment is complete; late proctitis occurs at least 3 months after completion of therapy, with recurrent bleeding as main feature; chronic phase can develop in 5% to 15% of cases[4]
Exam
no differentiating examination findings
1st investigation
- sigmoidoscopy:
diffuse inflammation
More
Other investigations
- rectal biopsy:
acute findings: cryptitis, loss of goblet cells, eosinophilia, stromal inflammation; late findings: subintimal fibrosis, telangiectasia of capillaries and post-capillary venules, endothelial degeneration, platelet thrombi formation[25]
Ischaemic proctitis
History
older patient with recent hypotensive episodes; in one case series, all patients were >55 years of age with a ruptured abdominal aortic aneurysm or other cause of hypotension; may also occur with systemic lupus erythematosus and after anaphylaxis[6]
Exam
can present with massive rectal haemorrhage, as well as sepsis and peritonism due to infarction of the rectal wall; hypotension; most cases of ischaemic injury to the colon are proximal to the rectum
1st investigation
- sigmoidoscopy:
sharp proximal demarcation of inflammation due to the arterial distribution
Other investigations
- biopsy:
necrosis and gangrenous changes in most instances due to the severity of the ischaemia[6]
- abdominal CT with intravenous contrast:
thickening of rectal wall with fat stranding
Proctitis related to non-steroidal anti-inflammatory drug use, caustic agent
History
Non-steroidal anti-inflammatory drug (NSAID) use, either oral or rectal; insertion of caustic agent per rectum (>16 agents have been implicated; most common are cleaning solutions and acids)
Exam
no differentiating examination findings
1st investigation
- sigmoidoscopy:
rectal NSAIDs: well-demarcated area of inflammation and/or ulceration within reach of NSAID suppository; oral NSAIDs: inflammation uncommon in rectal area, but may cause discrete ulcers
Other investigations
- biopsy:
acute inflammatory infiltrate of polymorphonuclear lymphocytes into the lamina propria
More
Diversion colitis
History
prior surgery leading to diversion of faecal flow from rectum; onset within 9 to 12 months of surgery; rectal bleeding, rectal discharge, tenesmus most common symptoms
Exam
presence of colostomy or ileostomy
1st investigation
- sigmoidoscopy:
continuous erythema and petechiae from the rectum spreading proximally[11]
Other investigations
- biopsy:
crypt abscesses, follicular hyperplasia, lamina propria infiltration with plasma cells; relative preservation of mucosal architecture
Mpox
History
a characteristic rash that typically progresses in sequential stages (from macules, to papules, vesicles, and pustules); anorectal symptoms have been reported (e.g., severe/intense anorectal pain, tenesmus, rectal bleeding, or purulent or bloody stools, pruritus, dyschezia, burning and swelling) in recent outbreaks, and may occur in the absence of a rash; fever may be a symptom of the prodromal period (usually preceding the appearance of the rash), but may present after the rash or not at all; other common symptoms may include myalgia, fatigue, asthenia, malaise, headache, sore throat, back ache, cough, nausea/vomiting, oral/oropharyngeal ulcers; there may be a history of recent travel to/living in endemic country or country with outbreak, or contact with suspected, probable, or confirmed case within the previous 21 days before symptom onset
Exam
rash or skin lesion(s) are usually the first sign of infection; physical examination may reveal a rash or lesion(s), and possibly lymphadenopathy; rash generally starts on the face and body and spreads centrifugally to the palms and soles (it may be preceded by a rash affecting the oropharynx and tongue in the 24 hours prior that often passes unnoticed); lesions simultaneously progress through four stages - macular, papular, vesicular, and pustular - with each stage lasting 1-2 days, before scabbing over and resolving; lesions are typically 5-10 mm in diameter, may be discrete or confluent, and may be few in number or several thousand; vesicles are well-circumscribed and located deep in the dermis; the rash may appear as a single lesion in the genital or perioral areas without a prodromal phase; perianal/rectal lesions and proctitis may be present; lymphadenopathy typically occurs with onset of fever preceding the rash or, rarely, with rash onset, may be submandibular and cervical, axillary, or inguinal, and occur on both sides of the body or just one side; inguinal lymphadenopathy has been commonly reported
1st investigation
- FBC:
may show leukocytosis, lymphocytosis, thrombocytopenia
- urea and electrolytes:
may show low urea or other derangements
- LFTs:
may show elevated transaminases, hypoalbuminaemia
- polymerase chain reaction:
positive for monkeypox or orthopoxvirus virus DNA
More - STI tests:
variable (depends on the infection present)
More
Use of this content is subject to our disclaimer