Approach
Clubbing is a bulbous uniform swelling of the soft tissue of the terminal phalanx of a digit, with subsequent loss of the normal angle between the nail and the nail bed. It is usually bilateral, although unilateral clubbing does exist.[30] It is a sign, rather than a condition. Once clubbing is identified, history and examination should focus on identification of the underlying cause.
History
A detailed history is necessary to exclude organic causes of clubbing.[29][30]
Symptoms associated with pulmonary aetiology
The presence of shortness of breath, chest pain, and cough (acute or chronic) on history-taking usually indicates an underlying pulmonary aetiology. A cough may be a symptom of hypersensitivity pneumonitis, congenital heart disease, thymus cancer, or Hodgkin's lymphoma. Production of purulent sputum is particularly suggestive of lung abscess, empyema, or bronchiectasis. Haemoptysis may indicate underlying lung cancer, pulmonary tuberculosis (TB), pulmonary artery sarcoma, interstitial pulmonary fibrosis, bronchiectasis, lung abscess, or myelofibrosis. Smoking is considered a risk factor for lung cancer, asbestosis, and interstitial pulmonary fibrosis.[40] Asbestos exposure is suggestive of asbestosis, lung cancer, or pleural mesothelioma. A known TB contact, travel to an endemic area, and/or a history of immunosuppression (particularly HIV infection) should arouse suspicion of cavitating pulmonary TB. A history of mineral or vegetable oil ingestion (e.g., laxative use) in a patient with respiratory symptoms supports a diagnosis of lipoid pneumonia.[41][42]
Symptoms associated with cardiac aetiology
Faltering growth in children, shortness of breath, diaphoresis, irritability, and recurrent lung infections, with or without cyanosis, strongly suggest a cardiac aetiology.
Adults who survive congenital heart disease may have symptoms of heart failure (dyspnoea, peripheral oedema, and fatigue) or differential cyanosis (pink upper extremities and cyanotic lower extremities, as can occur in coarctation of the aorta).
Symptoms that may help to narrow the differential diagnosis
Abdominal pain may occur in cystic fibrosis, ulcerative colitis, Crohn's disease, tropical sprue, or coeliac disease. Ulcerative oesophagitis can present with epigastric pain. In addition, diarrhoea may be a symptom of both cystic fibrosis and coeliac disease.
Fever often suggests an underlying infectious aetiology such as pulmonary TB, infective endocarditis, empyema, or lung abscess. Other conditions presenting with fever include pulmonary artery sarcoma, hypersensitivity pneumonitis, Hodgkin's lymphoma, disseminated chronic myeloid leukaemia, atrial myxoma, Crohn's disease, and tropical sprue. When considering tropical sprue as an underlying cause, a history of travel to endemic areas should be established.
Loss of weight is a fairly non-specific symptom and may occur with pulmonary TB, ulcerative colitis, Crohn's disease, tropical sprue, malignancy, metastatic disease, interstitial pulmonary fibrosis, chronic hypersensitivity pneumonitis, and achalasia.
Generalised weakness is associated with most conditions, particularly TB, lung cancer, congenital heart disease, inflammatory bowel disease, liver cirrhosis, cystic fibrosis, interstitial pulmonary fibrosis, and primary biliary cholangitis. Jaundice suggests underlying liver cirrhosis.
Night sweats are a common presenting symptom of pulmonary TB and Hodgkin's lymphoma. Patients with infective endocarditis may also complain of night sweats.
Paraesthesias may occur in association with lung metastases due to associated hypercalcaemia, paraproteinaemia, or vasculitis. Arthralgia is a feature of pachydermoperiostosis, sarcoidosis, and infective endocarditis.[31]
Nausea and vomiting are symptoms of early pregnancy and of ulcerative oesophagitis. A history of dysphagia should arouse suspicion of an oesophageal condition such as achalasia or leiomyoma of the oesophagus.
In thymus cancer almost one third of patients are asymptomatic. Chest pain, myasthenia gravis, cough, and dyspnoea may occur with equal frequency. Fatigue is common in thymoma, as are weakness and weight loss.[43]
Patients with thyroid acropachy usually have a history of thyrotoxicosis (Graves' disease, but it may also be present in Hashimoto's thyroiditis) and complain of related symptoms including heat intolerance, sweating, weight loss, palpitations, scalp hair loss, or irritability.
Physical examination
On clinical examination, in profile, the normal distal digit shows an angle made by the junction of the proximal nail fold and nail plate (Lovibond's angle) typically ≤160°. With clubbing this angle flattens, and then rises as the severity of the clubbing increases. If the angle is >180°, definitive clubbing exists. An angle between 160° and 180° possibly reflects early stages of clubbing or a pseudo-clubbing phenomenon.[Figure caption and citation for the preceding image starts]: Clubbing of nails showing loss of the classic Lovibond's angle (normally ≤160° in a normal distal digit, but >180° with definitive clubbing)From the collection of Dr Murlidhar Rajagopalan [Citation ends].
The Schamroth window test can be used to identify or confirm clubbing. If two opposing fingers are held back to back against each other, a diamond-shaped space should normally appear between the nail beds and the nails of the two fingers. In clubbing, this space (or window) is missing.[Figure caption and citation for the preceding image starts]: Schamroth window test demonstrating a diamond-shaped window when fingers are not clubbedCreated by BMJ Knowledge Centre [Citation ends].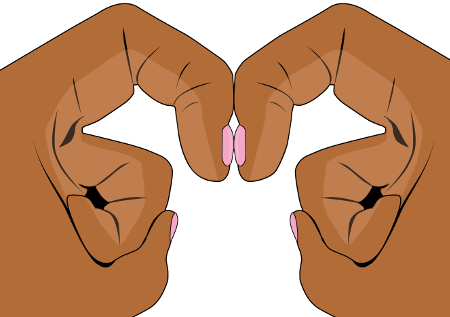 [Figure caption and citation for the preceding image starts]: Schamroth window test demonstrating lack of window with clubbed fingersCreated by BMJ Knowledge Centre [Citation ends].
[Figure caption and citation for the preceding image starts]: Schamroth window test demonstrating lack of window with clubbed fingersCreated by BMJ Knowledge Centre [Citation ends].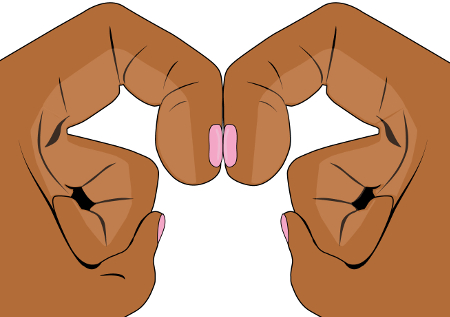 [Figure caption and citation for the preceding image starts]: Finger clubbingFrom the collection of Dr Murlidhar Rajagopalan [Citation ends].
[Figure caption and citation for the preceding image starts]: Finger clubbingFrom the collection of Dr Murlidhar Rajagopalan [Citation ends].
Examination for other clinical signs of the skin and nails
The following signs should be sought:[31][44]
Thickened palms and soles suggestive of palmoplantar keratoderma
Cutis verticis gyrata (thickened skin of the scalp manifesting as folds and furrows), associated with various conditions such as acromegaly and pachydermoperiostosis
Coarse skin indicative of acromegaly or pachydermoperiostosis
Acne, which may be associated with pachydermoperiostosis
Skin changes of liver disease including jaundice, spider naevi, and skin excoriations
Pallor suggesting anaemia (present in disseminated myeloid leukaemia, Crohn's disease, ulcerative colitis, coeliac disease, tropical sprue, and infective endocarditis)
Swellings that could indicate an aneurysm, such as axillary artery aneurysm and brachial arteriovenous malformations
Rashes, which may indicate a compromised immune state, such as underlying malignancy
Erythema nodosum, which may be a feature of sarcoidosis, Crohn's disease, and ulcerative colitis
Unilateral clubbing, which may indicate an axillary artery aneurysm or brachial arteriovenous malformation.
[Figure caption and citation for the preceding image starts]: Pachydermoperiostosis: furrowed and thickened foreheadFrom the collection of Dr Murlidhar Rajagopalan [Citation ends]. [Figure caption and citation for the preceding image starts]: Pachydermoperiostosis: finger clubbingFrom the collection of Dr Murlidhar Rajagopalan [Citation ends].
[Figure caption and citation for the preceding image starts]: Pachydermoperiostosis: finger clubbingFrom the collection of Dr Murlidhar Rajagopalan [Citation ends].
Examination of other systems
A complete physical examination of the lungs should be undertaken, looking for signs suggestive of fluid collection in the pleura (pleural effusion, empyema), consolidation, or collapse (pneumonia, TB). Pulmonary malignancies, including metastatic lesions, may also present with signs suggestive of fluid collection, consolidation, and/or collapse. Areas of hyper-resonance on the lung fields and evidence of cavitation (TB) or fibrosis (suggestive of interstitial pulmonary fibrosis, chronic hypersensitivity pneumonitis, or cystic fibrosis) should also be excluded.
A thorough cardiovascular examination should be performed to evaluate for signs suggestive of a right-to-left shunt (cyanosis together with a cardiac murmur indicates cyanotic congenital heart disease), infective endocarditis (cardiac murmur, Janeway's lesions, Osler's nodes, splinter haemorrhages, Roth's spots), and an atrial myxoma (systolic murmur, loud first heart sound, opening snap, embolic manifestations).
Hepatomegaly may be present on abdominal examination, indicating an underlying malignancy or the early stages of primary biliary cholangitis. Splenomegaly is almost always present in myelofibrosis. The presence of splenomegaly and ascites suggests advanced liver disease. Epigastric tenderness may be due to ulcerative oesophagitis. Ulcerative colitis, Crohn's disease, tropical sprue, coeliac disease, and cystic fibrosis can all present with varying degrees of abdominal pain.
Thyroid gland examination should focus on the presence of enlargement, nodules, and tenderness. This helps to exclude endocrine conditions associated with clubbing, such as thyroid acropachy.
Tender, swollen joints may suggest pachydermoperiostosis or secondary hypertrophic osteoarthropathy.[31][35] In addition to joint pain, patients with severe secondary hyperparathyroidism experience bone tenderness.[Figure caption and citation for the preceding image starts]: Pachydermoperiostosis: wrist joint swellingFrom the collection of Dr Murlidhar Rajagopalan [Citation ends].
Baseline investigations
Consider the following investigations when digital clubbing is identified.
Full blood count (FBC) with peripheral smear and erythrocyte sedimentation rate: useful when an underlying infectious or inflammatory cause, or malignancy is suspected. An FBC will show anaemia in myelofibrosis, and a peripheral blood smear will show teardrop-shaped red blood cells (RBCs) and the presence of metamyelocytes, myelocytes, promyelocytes, myeloblasts, and nucleated RBCs in the circulation.
Complete metabolic panel: necessary when evaluating for chronic illness (e.g., cystic fibrosis, sarcoidosis, and liver disease). Liver function tests are requested if a hepatobiliary cause is suspected, and thyroid function tests (serum free T3/total T3, serum free T4, and thyroid-stimulating hormone levels) are indicated if thyroid disease is suspected.
Chest x-ray: to search for an underlying pulmonary condition.
Blood cultures: when a possible infectious aetiology is suspected (e.g., lung abscess, infective endocarditis).
Urinalysis: may demonstrate active sediment (indicating septic emboli) in cases of infective endocarditis.
Specific investigations
Further investigation is guided by the above results coupled with findings on physical examination and a suggestive history.
Investigations for suspected respiratory cause
Sputum microscopy and culture, as well as cytology, should be requested where there is an underlying pulmonary cause associated with clubbing. If history or clinical examination suggests pulmonary TB, three sputum samples should be collected for acid-fast bacilli smear and culture, and nucleic acid amplification tests should be performed on at least one respiratory specimen.[45]
Spirometry helps to assess lung function and often supports various pulmonary diagnoses, particularly interstitial lung disease. Bronchoalveolar lavage is useful in confirming the diagnosis of lipoid pneumonia or hypersensitivity pneumonitis, and may be indicated in difficult-to-prove cases of TB. A diagnostic thoracentesis may be necessary when empyema or pleural mesothelioma is suspected.[46]
A chest computed tomography (CT) scan may be required to clarify or localise chest x-ray findings, especially where a pulmonary malignancy is the concern. It can detect metastases and helps to diagnose lymphoreticular malignancies such as Hodgkin's lymphoma. High-resolution chest CT (HRCT) is the test of choice when interstitial lung disease is suspected.[15]
A magnetic resonance imaging scan is useful to localise lesions. It may be combined with angiography to visualise the vascularity of the lesion or the relationship of the lesion to blood vessels.
A positron emission tomography scan is a useful investigation, especially when combined with CT scan for accurate definition of lesions. It is particularly helpful in detecting lymphomas of the chest or body.
Once the site of the lesion has been identified, a confirmatory tissue diagnosis is desirable. This may be achieved via bronchoscopy, aspiration techniques, tumour resection, or simple biopsy through endoscopy, all depending on lesion location.
When cystic fibrosis is suspected a sweat test is performed. Gene analysis may be indicated if the sweat test is inconclusive.
Investigations for suspected cardiac cause
When a structural heart defect is suspected, trans-thoracic echocardiogram is usually the first test performed. Trans-oesophageal echocardiogram is considered a more sensitive assay to detect structural defects and vegetations in infective endocarditis.[47] Cardiac catheterisation is a specialised investigation, done to confirm an echocardiogram finding or, rarely, to sample an intracardiac mass. It is also a useful tool to measure pressure changes in the heart accurately. Intravascular ultrasonography is useful for preoperative diagnosis of a pulmonary artery sarcoma. A final diagnosis is confirmed with histopathology following surgery.
When an arteriovenous malformation is present, Doppler ultrasonography detects the flow across a shunt and the direction of flow of blood in a vessel. This is considered especially helpful in delineating the origins of an aneurysm. Angiography or magnetic resonance angiography is useful, particularly when planning treatment of an arteriovenous anomaly.
Investigations for suspected hepatic or gastrointestinal cause
The size and texture of the liver is easily assessed with ultrasonography and, therefore, this is usually one of the initial tests ordered when evaluating liver disease, including cirrhosis.
Barium studies may be necessary when the underlying diagnosis is thought to be due to inflammatory bowel disease or an oesophageal abnormality. Colonoscopy is indicated when signs and symptoms suggest inflammatory bowel disease. This technique also allows tissue sampling for histopathology, which further confirms the diagnosis.
A prolonged prothrombin time is often associated with coeliac disease or liver cirrhosis. Coeliac disease may also result in iron deficiency; thus, iron studies should be sent. Serum folate and B12 analysis is necessary when tropical sprue is suspected, as malabsorption may reduce levels.
A 72-hour faecal fat collection to assess for steatorrhoea may assist in the diagnosis of tropical sprue (although a 24-hour sample is more commonly obtained).
Investigations for suspected endocrine cause
When acromegaly is suspected, growth hormone levels, coupled with measurement of insulin growth factor 1, confirms the diagnosis. Levels of serum parathyroid hormone, calcium, and vitamin D are indicated when the possibility of secondary hyperparathyroidism is a concern.
If thyroid cancer is suspected, thyroid ultrasonography helps determine the structure and nature of the thyroid mass. A fine needle aspiration biopsy of the suspicious lesion may be performed under ultrasound guidance for accurate tissue sampling. Cytology results confirm the diagnosis.
Investigations for suspected haematological cause
Cytogenetic testing (e.g., fluorescent in situ hybridisation) may be indicated in cases of disseminated chronic myeloid leukaemia. Determining lactate dehydrogenase level and immunohistochemical studies may be necessary when evaluating for Hodgkin's lymphoma.
Other potential investigations
Plain film radiographs of the hands and other joints may be helpful in confirming a diagnosis of secondary hypertrophic osteoarthropathy or pachydermoperiostosis.[31]
Skin biopsy is rarely necessary. However, in some conditions it may help to establish a diagnosis, including sarcoidosis, thyroid acropachy, and pachydermoperiostosis.[31]
Use of this content is subject to our disclaimer