Approach
Pruritus is a subjective sensation; therefore, the diagnosis is based solely on the patient's symptoms. However, a thorough history and complete physical examination are central to the evaluation of pruritus. During clinical evaluation, it is important to identify a possible cause or disease responsible for itching, as well as determining the intensity and timeframe of the pruritus.
In every patient with chronic pruritus it is essential to determine whether the itchy skin looks normal or not. For lesional skin, primary eruption must be differentiated from secondary scratch lesions. If primary skin lesions are present, the diagnosis is made based on clinical presentation, skin biopsy, and additional examinations, if necessary.
Patients with healthy-looking skin, or only with scratch lesions, require basic sets of laboratory examinations including blood morphology, erythrocyte sedimentation rate, iron level, kidney and liver function tests, serum glucose, hormones (namely thyroid-stimulating hormone), and, if necessary, skin biopsy (to exclude subclinical dermatoses or skin conditions camouflaged by secondary scratch lesions).
A detailed history must also be collected regarding the concomitant symptoms, co-existent diseases, and medical problems, as well as drugs taken by patients.[39]
Any abnormalities found in the above tests should direct further diagnostic procedures to confirm the cause of pruritus. If all these tests, as well as medical history, are within the normal range or negative, psychogenic pruritus should be suspected and psychological or psychiatric consultation may be warranted.
History
Disease history typically reveals the onset of pruritus, its intensity, and sleep disturbances related to it. Concomitant systemic diseases that could provoke itching should be considered in the patient's medical history and associated current symptoms. The physician should also take a thorough medication history and consult the pharmacological literature on adverse effects to establish the likelihood of drug-induced pruritus as a cause for the patient's itch.
Physical examination
Dermatological pruritus is diagnosed in patients with primary skin lesions that can be linked with itch sensation.
Other pruritus types (systemic, neurological, psychogenic) are often not associated with a visible skin problem, but many patients may have secondary scratch lesions. Special attention should be directed to identifying signs of secondary scratch lesions (e.g., excoriations, erosions, or nodular prurigo-like lesions) that aid differentiation from a primary skin eruption.[40]
In post-burn pruritus, additional tissue damage from scratching may be noted.[31]
During routine examination of patients with pruritus, the severity of this symptom is usually assessed by a visual analogue scale (VAS), the numerical rating scale (NRS), or by one of various itch questionnaires.[41] VAS and NRS are very simple and quick methods of measuring itching intensity; the patient marks the severity of the most intense pruritus within the last few days on a linear scale from 0 (no itch) to 10 (worst imaginable itch).[42][43][44][45]
Some conditions causing pruritus can be diagnosed on clinical findings alone and include skin xerosis, insect bites, diabetic peripheral neuropathy, postherpetic itch, depression, schizophrenia, somatoform disorder, and drug-induced pruritus.[Figure caption and citation for the preceding image starts]: Atopic dermatitis: erythema, excoriations, and lichenification in popliteal areaFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Lichenification due to chronic rubbing in a patient with atopic dermatitisFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Lichenification due to chronic rubbing in a patient with atopic dermatitisFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Prurigo nodularis: a disease with extensive scratch lesionsFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Prurigo nodularis: a disease with extensive scratch lesionsFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Prurigo nodularis: note sparing of upper part of back, which is difficult to access for scratchingFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Prurigo nodularis: note sparing of upper part of back, which is difficult to access for scratchingFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Prurigo nodularis: secondary scratch lesionsFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Prurigo nodularis: secondary scratch lesionsFrom the collection of Adam Reich MD, PhD [Citation ends].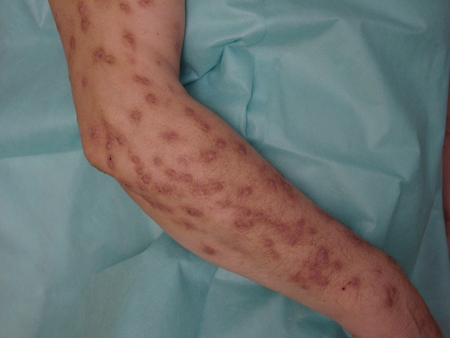
Investigations in dermatological causes
If a condition cannot be diagnosed based on the clinical findings alone, further investigation is warranted.
In suspected allergic dermatological conditions, such as atopic dermatitis or urticaria, the following investigations are indicated:
Total serum IgE level
Allergen-specific IgE levels
Prick tests with specific allergens (aeroallergens, food allergens, medications)
Skin biopsy.
In urticaria, additional tests may include physical tests (exposure to pressure, cold, heat, ultraviolet light, physical activity, water), exposure to drugs (e.g., acetylsalicylic acid), stool microscopy (for parasites) and antinuclear antibodies (ANAs), and intradermal injection of autologous serum (autologous serum skin test).[3][46][47]
Hymenoptera allergy radioallergosorbent (RAST) testing is performed to confirm an allergy to insect bites.
Microscopy of skin scrapings should be done to confirm scabies, and to exclude parasitic skin infestations in persistent delusional disorders. Dermoscopy may show scabies burrows and mites with characteristic 'jet-plane' appearance or may show eggs.
A skin biopsy should be performed to confirm suspected cases of lichen planus, dermatitis herpetiformis, and bullous pemphigoid. It is only done in patients with psoriasis if in doubt of the diagnosis. Direct immunofluorescence of the skin biopsy will further assist in the diagnosis of dermatitis herpetiformis and bullous pemphigoid, with further supportive tests performed depending on the most likely diagnosis.
Stool microscopy should be performed in suspected systemic parasitic infection. In these cases a blood smear and serological tests will further help to confirm the parasite involved.
Serological testing for hepatitis B or C antibodies may be performed if lichen planus is diagnosed, as some studies have demonstrated an association between lichen planus and viral hepatitis.[Figure caption and citation for the preceding image starts]: Atopic dermatitis: white dermographismFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Atopic dermatitis: erythema, excoriations, and lichenification in popliteal areaFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Atopic dermatitis: erythema, excoriations, and lichenification in popliteal areaFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Lichenification due to chronic rubbing in a patient with atopic dermatitisFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Lichenification due to chronic rubbing in a patient with atopic dermatitisFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Acute urticaria: typical whealsFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Acute urticaria: typical whealsFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Urticaria: whealsFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Urticaria: whealsFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: ScabiesFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: ScabiesFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Scabies: typical lesions within interphalangeal areasFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Scabies: typical lesions within interphalangeal areasFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Lichen planus: lacy network traversing the buccal mucosaFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Lichen planus: lacy network traversing the buccal mucosaFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Lichen planus: flat, violaceous papules with visible Köbner phenomenon (arrow)From the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Lichen planus: flat, violaceous papules with visible Köbner phenomenon (arrow)From the collection of Adam Reich MD, PhD [Citation ends].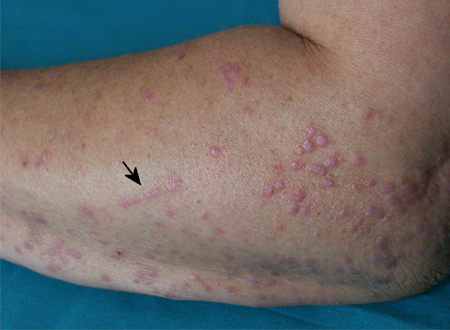 [Figure caption and citation for the preceding image starts]: Dermatitis herpetiformis: typical lesions on extensor surface of forearmFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Dermatitis herpetiformis: typical lesions on extensor surface of forearmFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Dermatitis herpetiformis: highly pruritic vesicles, small blisters, and erosions on extensor surfaces of extremitiesFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Dermatitis herpetiformis: highly pruritic vesicles, small blisters, and erosions on extensor surfaces of extremitiesFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Bullous pemphigoid: tense blisters and erosions on erythematous backgroundFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Bullous pemphigoid: tense blisters and erosions on erythematous backgroundFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Plaque type psoriasisFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Plaque type psoriasisFrom the collection of Adam Reich MD, PhD [Citation ends]. [Figure caption and citation for the preceding image starts]: Psoriasis: symmetrical plaques on the back covered with thick scalesFrom the collection of Adam Reich MD, PhD [Citation ends].
[Figure caption and citation for the preceding image starts]: Psoriasis: symmetrical plaques on the back covered with thick scalesFrom the collection of Adam Reich MD, PhD [Citation ends].
Investigations in systemic causes
In cases of systemic causes of pruritus, investigations appropriate to the condition are indicated. Examples include the following:[2]
Liver function tests in cholestatic pruritus
Renal function, and total serum calcium and serum phosphorus levels, in chronic renal failure
Thyroid function tests in thyroid disease
Iron studies in iron deficiency anaemia
Blood morphology in iron deficiency anaemia, polycythaemia vera, and paraneoplastic pruritus
Viral load, serological tests, and CD4 count in suspected HIV infection.
Sonography of the abdomen and peripheral lymph nodes is performed in evaluation of Hodgkin's lymphoma and polycythaemia vera. Imaging in evaluation of paraneoplastic pruritus depends on the suspected malignancy and may include sonography, x-ray examination, CT, MRI, or scintigraphy.
Biopsy may be indicated in further evaluating haematological pathologies and malignancies. Lymph node biopsy is used to confirm diagnosis in Hodgkin's lymphoma and paraneoplastic pruritus. Bone marrow aspirate aids diagnosis of polycythaemia vera and haematological malignancies.
Diabetic peripheral neuropathy is usually a clinical diagnosis but can be confirmed using nerve conduction tests, electromyogram, and quantitative sensory testing.
Investigations in neurological causes
Neurological pruritus is frequently localised to areas innervated by particular nerves. Although pruritus can be the only symptom of neurological damage, in many cases patients present with other neurological symptoms. Frequently they may have other feeling disturbances in the area of pruritus.
All suspected neurological causes require imaging. MRI is used for initial diagnosis of multiple sclerosis and brain tumour. Non-contrast CT is the first-line imaging tool in patients with acute stroke.
X-ray of the vertebral column is the initial test to diagnose brachioradial pruritus (cervical spine) and notalgia paraesthetica (thoracic spine). MRI in both conditions also helps to confirm the diagnosis.[48][49]
Cerebrospinal fluid analysis is performed in evaluation of multiple sclerosis.
Use of this content is subject to our disclaimer