Approach
Although history and examination are key to identifying an RPA, imaging or the spontaneous or surgical drainage of the abscess confirms the diagnosis.[8]
History
A careful history is important, as other serious conditions are part of the differential diagnoses. RPAs are most commonly the sequelae of an upper respiratory tract infection (e.g., pharyngitis, tonsillitis, sinusitis, dental infections). They occur more commonly in children; therefore, a history of foreign body ingestion should be noted.
In children, presentation may be vague and depends on the stage of disease, but characteristic symptoms include spiking fever, neck pain (especially on movement) or torticollis, and dysphagia. Other common symptoms include irritability, malaise, mild photophobia, and odynophagia (painful swallowing). Odynophagia causes drooling, poor oral intake, and anorexia. Less common symptoms include trismus (lockjaw), dysphonia (hoarseness), stridor, or sleep apnoea. The child may also be seen to pull at their ears or throat, which indicates pain.[3]
In adults, the presentation may be more specific with drooling and dysphagia, but is usually more insidious in onset. It is important to enquire about comorbidities such as diabetes mellitus and optimise glycaemic control if present. Up to one third of patients with a deep neck abscess have diabetes mellitus.[4]
Airway compromise usually presents with symptoms of dyspnoea, distress, and fatigue. Patients with a more complicated clinical course are more likely than those with a smooth clinical course to present with airway obstruction or multiple abscesses.[19]
Physical examination
An attempt should be made to examine the oral cavity and neck to look for tonsillar swelling, oropharyngeal swelling, and lymphadenopathy. Other important observations may be made such as drooling, dyspnoea, torticollis, and neck swelling/mass. In children the examination may be limited depending on the age and co-operation of the child (and parents).
Airway compromise usually presents as tachypnoea, cyanosis, tracheal tug, or intercostal recession. High respiratory rate and oxygen saturations aid diagnosis of a compromised airway. In cases where there is a concern of airway compromise in the form of partial airway obstruction, stridor, or stertor, oropharyngeal examination may be best performed in a controlled setting (i.e., in the operating theatre where an emergency surgical airway can be established if required).[20]
Laboratory investigations
A full blood count with differential should be ordered initially to confirm neutrophilia. The erythrocyte sedimentation rate can be measured to establish the degree of inflammatory disease in the absence of a significant neutrophilia. Blood cultures are not usually taken, unless sepsis is suspected. In unusual presentations consider testing for Epstein-Barr virus, cytomegalovirus, and toxoplasmosis titers in addition to C-reactive protein.[20]
Imaging
Radiological investigations are required to confirm diagnosis. The selected investigation depends on the degree of suspicion and access to the different imaging modalities, as well as the severity of the case. Nonetheless, a CT scan is the definitive investigation and will demonstrate a ring-enhancing lesion in the retropharyngeal tissues when performed with contrast.
If there is an airway concern or a likelihood of surgical drainage, then sedating and intubating a child before CT scanning with a view to proceeding to the operating theatre should be considered.
Ultrasonography and plain x-ray of the neck will provide some evidence of an RPA, but these modalities are less sensitive and less specific than a CT scan.[21] They should only be used when a CT scanner is not available.[22][23]
MRI is not used to diagnose this condition, as CT gives such a clear result in most cases and is usually more readily available and cheaper as a resource.
[Figure caption and citation for the preceding image starts]: CT scan of neck demonstrating ring-enhancing lesionPhilpott CM, Selvadurai D, Banerjee AR. Paediatric retropharyngeal abscess. J Laryngol Otol. 2004;118:919-926 [Citation ends].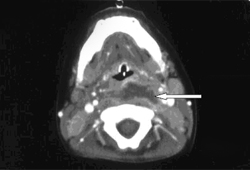
Surgery
Examination under anaesthetic (EUA) should be performed if diagnosis of RPA is strongly suspected and the airway is compromised or if a CT scanner is not available. EUA should also be performed if CT scan (or other imaging investigations if CT is not available) has been performed and the result is consistent with RPA. In cases where CT does not show well defined ring-enhancing lesions, trial of intravenous antibiotics can be tried before considering surgical drainage.[24]
EUA allows confirmation of diagnosis and allows transoral incision and drainage. A well circumscribed, uniloculated RPA may, in selected adults, be adequately treated with ultrasound guided drainage.[25][26] A specimen of pus should be taken for culture and sensitivity at the time of drainage.
Use of this content is subject to our disclaimer