Approach
Practitioners should recognise their limitations, and where necessary, seek further advice or refer the patient to an ophthalmologist.[11] The diagnosis of corneal epithelial defects is typically based on the history and clinical examination findings. Further investigations are rarely required.
History
Patients will typically present with a new corneal abrasion or a recurrent corneal erosion.
New corneal abrasions
Onset is usually sudden. Typical symptoms include a foreign body sensation (even if none is present), photophobia, excessive tearing, blepharospasm, and blurry vision. There is usually a history of trauma, such as an object striking the eye, a foreign body entering the eye and becoming stuck under the eyelid, or difficult contact lens removal.
Specific considerations include:
Exposure to airborne particles of dust, glass (e.g., in occupations that involve grinding and cutting); lack of protective eyewear increases the risk of abrasion.[7][9]
Children may not be able to recall or vocalise a history, but corneal abrasion should be considered a possibility in inconsolable infants (e.g., may occur unconsciously at night if the eye is scratched during sleep).
Poorly fitting, overly worn, or inadequately cleaned contact lenses may increase the risk of corneal abrasion (if the eye or the lens becomes dry, it may adhere to part of the underlying corneal epithelium, which is then removed with the contact lens, causing a defect).
Recurrent corneal erosions
Patients with recurrent or spontaneous erosions often have some history of distant trauma.[5] The injury might have occurred days, weeks, or months earlier, leaving an underlying structural defect in the epithelium that places them at risk for recurrent erosions. Patients usually report symptom onset immediately after opening their eyelids (e.g., on waking after sleep); symptoms may recur every day or at regular weekly or monthly intervals.[5] Together with the typical traumatic causes of corneal abrasion, enquire about a history of epithelial basement membrane degeneration or corneal dystrophies.[4][5]
Eye examination
The eye should be carefully examined, using a topical anaesthetic if necessary to ease any discomfort.[12][13][14] One drop in the eye may cause rapid pain relief that lasts about 10-20 minutes. However, repeat doses should be avoided due to the potential for toxicity and retarded healing of the corneal epithelium.[13][15][16]
The eye is typically injected with ciliary flush (a ring of red or violet around the cornea) and tearing, but without pus. A corneal opacity should raise the concern for a potential infection.
The pupillary reflexes should be checked using a pen torch. Examination of the red reflex will back-light any corneal defects, which will appear to move in the opposite direction to movement of the examiner’s head. A funduscopic examination can be attempted but is often difficult due to the presence of a small pupil and photophobia. Eversion of the eyelid may reveal a foreign body, but this may already have been expelled. Any obviously loose foreign bodies may be removed with a cotton-tipped applicator or by irrigation; otherwise, this should only be attempted by a practitioner who has been formally trained in foreign body removal.[14]
Iron- or metal-containing foreign bodies may leave a rust ring, which should be documented and receive ophthalmic follow-up in 1-2 days for removal. Corneal defects due to contact lenses are often round and centrally located, and can sometimes involve the entire corneal surface.
A same-day ophthalmology consultation is needed if there is an obvious penetrating injury, extruding aqueous humor, an irregular pupil, or pus (hypopyon) or blood (hyphema) in the anterior chamber.[11] Pressure on the globe must be avoided if a penetrating injury is suspected.
Investigations
Visual acuity should be tested and documented because defects in the visual axis accompanied by corneal oedema can cause changes in vision and acuity.
Slit lamp examination will reveal obvious corneal defects or foreign bodies (e.g., punctate epithelial erosions or linear vertical corneal abrasions). Include eyelid eversion with careful examination of the tarsal conjunctiva and gonioscopy to check the iris and angle. Fluorescein examination can be performed by placing an applicator strip, moistened with saline or topical anaesthetic, into the inferior cul-de-sac. On blinking, fluorescein is distributed over the corneal epithelium and stains any exposed basement membrane. A cobalt blue filter will identify the corneal defect. Fluorescein that changes colour or seems to stream (positive Seidel's test) should raise suspicion for a penetrating globe injury. Suspicion of a penetrating injury to the globe or a possible intraocular foreign body with a history of significant trauma suggests the need for computed tomography.[Figure caption and citation for the preceding image starts]: Corneal abrasion seen with fluorescein stainCourtesy of Dr Jonathan Smith, Royal Victoria Infirmary, Newcastle upon Tyne, UK; Dr Philip Severn, Sunderland Eye Infirmary, Tyne and Wear, UK; and Dr Lucy Clarke, Royal Victoria Infirmary, Newcastle upon Tyne, UK [Citation ends].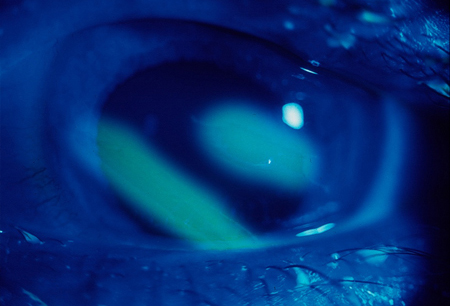
Use of this content is subject to our disclaimer