Aetiology
People who are at risk of PTSD include those who have been exposed to, or have witnessed, extreme traumatic stressors, such as intentional acts of violence, physical and sexual abuse, accidents, disaster, or military action. People who have experienced a threat to their own life or the life of others while in medical care, such as during anaesthesia, complications during childbirth, or as a result of medical negligence, are also at risk.
PTSD is unique among functional psychiatric disorders in that its presence can be directly attributed to an external causative factor. This has not always been accepted, and it was previously thought that only people with mental illness, an unstable personality, or pre-existing neurotic conflict could develop the symptoms of what is now recognised as PTSD. That it was possible for people without pre-existing mental illness or personality disorder/traits to develop the symptoms of PTSD after exposure to traumatic events became clear through studies, in particular of veterans of the Vietnam war and survivors of rape. The criteria for an event to be regarded as a traumatic stressor are that there must have been actual or threatened death, serious injury, or other threat to physical integrity. Factors that influence a person's susceptibility to develop PTSD have also been the subject of much research, and include previous psychiatric history, lower IQ, female sex, and prior exposure to trauma, among others.[13][14]
A number of psychological and neurobiological theories have been put forward to account for the pattern of symptoms characteristic of PTSD. However, the degree of variance explained by them is small. The current, principal psychological theories are: emotional processing theory, dual representation theory, and the cognitive model of PTSD.[15][16][17]
Emotional processing theory: implicates complex fear structures, which exist in memory and which produce cognitive, behavioural, and physiological reactions when activated.[15] It is argued that in PTSD, these have become pathological. Alterations in beliefs about the world and the self, brought about by difficulties in processing information about the traumatic event, lead to misinterpretation of benign stimuli as dangerous and of the self as being incompetent.
Dual representation theory: based on research into memory processing, and argues the existence of different types of memory, namely verbally accessible memories (VAMs) and situationally accessible memories (SAMs).[16] Whereas VAMs are easily recalled, SAMs remain unconscious until triggered, whereupon they give rise to symptoms such as dreams and flashbacks, during which the emotions felt during the traumatic event are re-experienced with the same degree of intensity.
Cognitive model of PTSD: argues that negative appraisals of the traumatic event lead to the development of views of the world as a dangerous place and of the self as incompetent.[17] This leads to a sense of current threat in which situations are misinterpreted as threatening.
There are a number of important maintaining factors in PTSD, including unhelpful coping strategies and lack of social support. Coping strategies that are thought to be helpful but that tend to prolong or exacerbate symptoms include conscious suppression of trauma memories, rumination about the event, dissociation, social withdrawal, avoidance, and substance use. Lack of social support, often made worse if the person feels alienated from others and withdraws from previously significant relationships, is associated with increased chronicity.[13][14]
Lengthy legal proceedings often follow traumatic experiences, and are very likely to contribute to the person's distress and make it more difficult to put the event in the past. There is a complex relationship between litigation and the symptoms of PTSD, but the idea that the symptoms are primarily due to compensation-seeking is not supported by the evidence.
Pathophysiology
Research has focused on the areas of the brain associated with fear processing and memory: namely, the amygdala, the hippocampus, and the medial prefrontal cortex, including the anterior cingulate gyrus.[Figure caption and citation for the preceding image starts]: Three-dimensional MRI scan showing the limbic system, including the hippocampus (mid-brown)Arthur Toga/UCLA/SPL [Citation ends].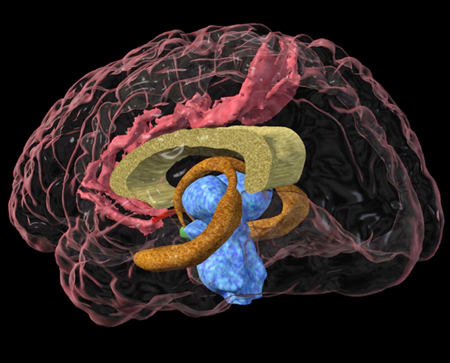 The principal areas of interest in neurobiological research currently are: reduced hippocampal size; failure of the medial prefrontal-anterior cingulate networks to regulate amygdala activity, resulting in hyper-reactivity to threat; and an oversensitive negative-feedback system whereby low levels of cortisol inhibit production of adrenocorticotropic hormone (ACTH) by the anterior pituitary gland, leading to failure to contain the sympathetic response, which is believed to lead to the consolidation of traumatic memories.[18][19][20][21]
The principal areas of interest in neurobiological research currently are: reduced hippocampal size; failure of the medial prefrontal-anterior cingulate networks to regulate amygdala activity, resulting in hyper-reactivity to threat; and an oversensitive negative-feedback system whereby low levels of cortisol inhibit production of adrenocorticotropic hormone (ACTH) by the anterior pituitary gland, leading to failure to contain the sympathetic response, which is believed to lead to the consolidation of traumatic memories.[18][19][20][21]
Studies in animals that have shown stress-induced hippocampal cell damage and loss have led to the suggestion that reduced hippocampal size is secondary to PTSD. However, studies of twins involved in the Vietnam war have led to debate as to whether reduced hippocampal size is a vulnerability factor for the development of PTSD, rather than a result.[18]
It has been hypothesised that PTSD represents a failure of the medial prefrontal-anterior cingulate networks to regulate amygdala activity, resulting in hyper-reactivity to threat.[19] This is based on magnetic resonance imaging studies of blood flow in the brains of people with PTSD when exposed to reminders of what happened. A replicated finding has been increased amygdala activity that correlates with decreased activity in the medial prefrontal cortex.
The hypothalamic-pituitary-adrenal axis plays a major role in maintaining homeostasis within the body. Fearful situations lead to production of cortisol through a loop involving the amygdala, hypothalamus, and anterior pituitary gland. Optimal cortisol levels reduce the risk of developing and maintaining PTSD by inhibiting traumatic memory retrieval and containing the sympathetic response. There is evidence that in PTSD, lower than normal levels of cortisol inhibit production of ACTH from the anterior pituitary gland. In addition, there is evidence of down-regulated sensitivity to corticotropin-releasing factor (CRF) resulting in suboptimal levels of cortisol.[20] The elevated CRF levels directly influence increased norepinephrine (noradrenaline) release by stimulating the locus coeruleus: it is believed that this failure to contain the sympathetic response leads to the consolidation of traumatic memories.[21] However, there is conflicting evidence regarding low cortisol levels.[22]
Other neurochemicals that have been implicated in PTSD include serotonin, gamma-aminobutyric acid, glutamate, neuropeptide-Y, and brain-derived neurotrophic factor. It is likely that the true neurobiology of PTSD is complex and involves a range of these and other factors.[23]
Classification
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR)[1]
Draws a distinction between acute stress disorder (also known as combat and operational stress reaction in the military; symptoms are present for <1 month) and PTSD (where symptoms are present for ≥1 month).
PTSD may be:
With a dissociative subtype when symptoms of depersonalisation (e.g., experience of being an outside observer) or derealisation (e.g., experience of unreality, distance, or distortion) are present.
With delayed expression when full diagnostic criteria are not met until at least 6 months after the stressor.
Clinical classification: symptom severity
Mild:
Distress caused by the symptoms is manageable by the patient, and the patient's social and occupational functioning are not significantly impaired.
Moderate:
Distress and impact on functioning lie somewhere between mild and severe and there is not considered to be a significant risk of suicide, harm to self, or harm to others.
Severe:
Distress caused by the symptoms is felt to be unmanageable by the patient, and/or they cause significant impairment in social and/or occupational functioning, and/or there is considered to be significant risk of suicide, harm to self, or harm to others.
Use of this content is subject to our disclaimer