Investigations
1st investigations to order
ECG
Test
A resting 12-lead ECG is recommended at the first clinic visit in all individuals with known or suspected hypertrophic cardiomyopathy (HCM) and should be repeated whenever there is a change in symptoms in patients with an established diagnosis.[1] Most patients have ECG abnormalities; these are not specific to HCM, but rather, should prompt further investigation with echocardiography. An abnormal ECG may predate the finding of hypertrophy on echocardiography.[23]
Repolarisation abnormalities are common. T-wave inversion commonly involves the inferior and lateral leads and T waves are deep and often preceded by ST-segment depression.[24] Deeply inverted T waves in the precordial leads are suggestive of apical HCM.[25]
Prominent abnormal Q waves may be seen in the inferior (II, III, aVF) and/or lateral (I, aVL, V5-6) leads, reflecting septal hypertrophy.[25]
Increased QRS voltages indicating left ventricular hypertrophy (LVH) may be present. These are nearly always associated with other ECG abnormalities in HCM.[24] The presence of isolated QRS voltage criteria for LVH in the absence of other ECG markers is present in fewer than 2% of patients with HCM.[26]
ECG signs of left and right atrial enlargement and P-wave prolongation (a known predictor of atrial fibrillation) may be observed. They rarely occur in isolation; other ECG abnormalities such as repolarisation changes or signs of LVH are generally present. Left atrial enlargement reflects diastolic dysfunction, high filling pressures, outflow obstruction, and functional mitral regurgitation. Left atrial dilatation and dysfunction are markers of adverse prognosis.[24]
Left-axis deviation (caused by LVH) and ventricular pre-excitation may also be seen.[24]
Some patients may present with arrhythmias; for example, atrial fibrillation or supraventricular tachycardia.[24]
The ECG is normal in only a small proportion (5% to 10%) of patients at presentation.[1][25] These patients have been reported to have a more favourable clinical course than those with ECG abnormalities.[26]
[Figure caption and citation for the preceding image starts]: ECG showing changes associated with LVHFrom the collection of Melanie Everitt MD, Heart Failure & Transplantation Program, Primary Children's Medical Center, Salt Lake City, UT; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Giant T-wave inversionFrom the collection of Dr Anji T. Yetman MD, University of Utah [Citation ends].
[Figure caption and citation for the preceding image starts]: Giant T-wave inversionFrom the collection of Dr Anji T. Yetman MD, University of Utah [Citation ends].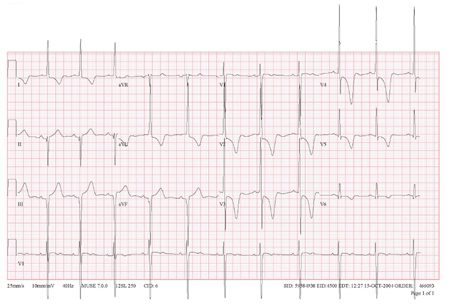
Result
ST-T wave abnormalities; prominent Q waves; LVH; P-wave abnormalities; left-axis deviation; ventricular pre-excitation; may be normal
creatine kinase (CK)
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy (HCM) should have routine laboratory tests done to establish aetiology, assess disease severity, and aid in the detection of extracardiac manifestations and assessment of secondary organ dysfunction.[1]
Raised CK levels are a useful clue when trying to establish aetiology; metabolic disorders such as Danon or mitochondrial disease, which can mimic HCM, should be considered.[50] When CK is persistently raised, a detailed examination by a neurologist should be considered.[1]
Result
normal; raised levels should raise suspicion of metabolic disorders
liver function tests
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy (HCM) should have routine laboratory tests done to establish aetiology, assess disease severity, and aid in the detection of extracardiac manifestations and assessment of secondary organ dysfunction.[1]
Liver dysfunction is prevalent in patients with chronic heart failure.[51] Abnormal liver function tests can also be a useful clue when trying to establish aetiology; metabolic disorders such as Danon's disease, which can mimic HCM, should be considered.[50]
Result
normal; may be abnormal in patients with chronic heart failure
renal function tests
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy should have routine laboratory tests done to establish aetiology, assess disease severity, and aid in the detection of extracardiac manifestations and assessment of secondary organ dysfunction.[1]
Impaired renal function may be seen with severe left ventricular dysfunction.[52]
Result
may be abnormal in patients with severe left ventricular dysfunction; normal
N-terminal pro-brain natriuretic peptide (NT-proBNP)
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy should have routine laboratory tests done to establish aetiology, assess disease severity, and aid in the detection of extracardiac manifestations and assessment of secondary organ dysfunction.[1]
High NT-proBNP levels are associated with cardiovascular events, heart failure, and death, and may have diagnostic, prognostic, and therapeutic monitoring value.[1]
Result
raised in heart failure; may be normal
troponin
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy should have routine laboratory tests done to establish aetiology, assess disease severity, and aid in the detection of extracardiac manifestations and assessment of secondary organ dysfunction.[1]
Raised troponin levels are associated with a higher risk of cardiovascular events, heart failure, and death, and may have diagnostic, prognostic, and therapeutic monitoring value.
Result
raised levels indicate increased risk of cardiovascular events; may be normal
urinalysis
Test
US guidelines do not recommend laboratory tests as part of the initial work-up.[2] However, European guidelines recommend that all patients with suspected or confirmed hypertrophic cardiomyopathy should have their urine checked for protein; proteinuria is suggestive of renal impairment.[1]
Result
proteinuria; normal
CXR
Test
This test is not particularly sensitive. Patients may have cardiomegaly secondary to left ventricular hypertrophy or left atrial enlargement, or the CXR may be normal.[4][Figure caption and citation for the preceding image starts]: CXR of a patient with HCM demonstrating cardiomegalyFrom the collection of Melanie Everitt MD, Heart Failure & Transplantation Program, Primary Children's Medical Center, Salt Lake City, UT; used with permission [Citation ends].
Result
cardiomegaly; normal
transthoracic echocardiography with Doppler
Test
At initial assessment of all patients with hypertrophic cardiomyopathy (HCM), transthoracic 2D and Doppler echocardiography are recommended. The classic finding is left ventricular hypertrophy (LVH), typically asymmetric hypertrophy of the septum.[4][27]
Echocardiography is also used for family screening of an affected individual, and for risk assessment of sudden cardiac death (SCD) in patients with a known diagnosis of HCM.
Clinical diagnosis of HCM is confirmed when maximal end-diastolic wall thickness ≥15 mm is imaged anywhere in the left ventricle (LV). More limited hypertrophy (≥13 mm) can be diagnostic when present in family members of a patient with HCM or in conjunction with a positive genetic test.[2][27]
Systolic anterior motion of the mitral valve may also be seen, along with mitral insufficiency.
LV outflow tract obstruction (LVOTO) may be present.[2] By convention, LVOTO is defined as a peak instantaneous Doppler LV outflow tract gradient of ≥30 mmHg, but the threshold for invasive treatment is usually considered to be ≥50 mmHg.[1]
There may also be abnormalities of diastolic function (present in 80% of patients independent of the presence of LVOTO).[2] Diastolic dysfunction should be assessed by Doppler tissue imaging as part of the echocardiographical screening test of first-degree relatives, as this abnormality may precede the onset of overt LVH.[27][28]
Result
LVH, typically asymmetric septal hypertrophy; left ventricular outflow tract obstruction may or may not be present; diastolic dysfunction may or may not be present
Investigations to consider
exercise ECG
Test
Exercise testing is performed to aid in risk stratification.
Abnormalities associated with an increased risk of sudden death include: abnormal blunted systolic BP response of <20 mmHg to exercise, ventricular arrhythmias, progressive ST depression, and symptoms.[29][30]
Result
may be normal or may demonstrate reduction in maximal oxygen consumption, abnormal blunted BP response, ST segment depression, arrhythmias
Holter monitoring
Test
Ventricular arrhythmias are associated with an increased risk of sudden death.
Result
may be normal or demonstrate ventricular or supraventricular arrhythmias
nuclear imaging exercise test
Test
Patients with exertional chest pain or ventricular tachycardia on Holter monitoring should undergo nuclear testing with either single-photon-emission computed tomography or positron emission tomography.[27] Myocardial perfusion imaging may demonstrate perfusion defects even in the absence of obstructive lesions.[2] Patients may have fixed or reversible defects. Patients with reversible defects should undergo cardiac catheterisation to identify possible causes of ischaemia.
Nuclear medicine can also play a role in diagnosis; it is particularly helpful in the aetiological diagnosis of cardiac amyloidosis.[1]
Result
may be evidence of ischaemia
cardiac magnetic resonance (CMR)
Test
Contrast-enhanced CMR can be a useful adjunct in patients with hypertrophic cardiomyopathy (HCM) at initial evaluation.[1][2] It can aid diagnosis and contribute to risk stratification and management. Left ventricular (LV) wall thickness can be assessed; the use of CMR may thus increase the diagnostic yield in patients with suspected HCM who have poor visualisation by echocardiogram of the LV walls or LV apex.[1][2][27]
Systolic and diastolic function can also be assessed, as well as mitral valve function, LV outflow tract obstruction, and left atrial dimensions.[1]
The use of late gadolinium enhancement techniques can identify areas of myocardial fibrosis that may be a marker for adverse outcomes, or may aid in differentiating HCM from an athletic heart.[31]
CMR is also emerging as a means of identifying patients who are at increased risk for arrhythmias. Several studies have found the presence of myocardial fibrosis by late gadolinium enhancement to be associated with the occurrence of ventricular arrhythmias, as well as an independent risk factor for death.[2][32][33][34][35][36][37]
Tissue characterisation on CMR can provide clues regarding aetiology, as characteristic findings are associated with certain diseases, for example, in sarcomeric HCM, a patchy mid-wall in hypertrophied areas is typical, while in amyloidosis-related cardiac hypertrophy, diffuse subendocardial late gadolinium enhancement is seen. These findings should be assessed collectively with genetic results and other clinical features by operators expert in cardiac imaging and the evaluation of heart muscle disease.[1]
Serial follow-up CMR, every 2-5 years depending on initial severity and clinical course, can assist in evaluating disease progression as well as the benefits of therapy.[1]
Result
LVH; may show left ventricular outflow tract obstruction, structural abnormalities of mitral valve and papillary muscle, systolic and/or diastolic dysfunction, and left atrial enlargement; later in disease course: may demonstrate myocardial fibrosis
cardiac computed tomography (CT)
Test
Although not used commonly, CT can provide important insights when echocardiography is technically limited and imaging is contraindicated or unavailable.[2] Cardiac CT provides clear definition of left ventricular structure (including hypertrophy pattern, wall thickness measurement, detection of subaortic membrane, and intracardiac thrombus) and function. Disadvantages of CT are the use of radiation and radioiodine contrast and inferior temporal resolution compared with echocardiography.[2]
Result
LVH; may show systolic anterior motion of mitral valve, intracardiac thrombi and patchy or diffuse delayed iodine enhancement
CT coronary arteriography
cardiac catheterisation
Test
In symptomatic patients with hypertrophic cardiomyopathy and inconclusive non-invasive cardiac imaging, left and right heart catheterisation may be considered to assess the severity of left ventricular outflow tract obstruction and to measure LV filling pressures.[1][2]
Patients with exertional chest pain, ischaemia on nuclear testing, or an increased probability of coronary artery disease based on risk factors should undergo cardiac catheterisation to rule out co-existent atherosclerotic coronary disease or myocardial bridging.[2] Also recommended for patients who are candidates for septal reduction therapy.[2]
Result
usually normal; may be evidence of atherosclerotic coronary artery disease
stress echocardiography
Test
Can be helpful in selected patients to evaluate myocardial ischaemia.[1]
Result
normal; myocardial ischaemia
exercise echocardiography
Test
Can be useful to identify provocable left ventricular outflow tract obstruction and exercise-induced mitral regurgitation in symptomatic patients with hypertrophic cardiomyopathy.[1]
Result
normal; myocardial ischaemia
trans-oesophageal echocardiography
Test
Limited to select indications, such as the exclusion of atrial thrombi related to atrial fibrillation, investigating the method of obstruction in patients with left ventricular outflow tract obstruction where this is not obvious, elucidating the mechanism of mitral regurgitation, or planning invasive interventions such as septal myectomy.[1]
Result
LVH; may show other abnormalities such as atrial thrombi or intrinsic mitral valve abnormality
endomyocardial biopsy
Test
Not usually recommended for diagnosis of hypertrophic cardiomyopathy but may be considered on rare occasions, especially when the pattern of hypertrophy is diffuse and there is suspicion for other cardiomyopathies presenting with hypertrophy.[1]
Result
may show features of alternative cause for LV hypertrophy, such as storage disease (e.g., Fabry disease) or infiltrative process (e.g., amyloidosis)
genetic mutation analysis
Test
Currently identified disease-causing genes are thought to account for 80% of cases of the disease, and the sensitivity of commercially available genetic testing may be lower depending on the number of genes screened for by the particular laboratory. When the eight most common sarcomeric mutations are screened for, the clinical sensitivity approaches 60%.[17] In up to 40% of patients with hypertrophic cardiomyopathy (HCM), no sarcomere variant is identified, and there is no family history of disease.[43] The absence of a monogenic disease-causing variant on conventional genetic testing leaves three possibilities: (i) either there is a monogenic cause that has not been identified (i.e., not detected or recognised as causative by current testing); (ii) the cardiomyopathy does not have a genetic aetiology; or (iii) the cardiomyopathy is attributable to the effects of multiple variants of individually smaller effect.[1]
When a mutation is identified, genetic testing is useful for screening other relatives to determine requirement for ongoing cardiology follow-up. Relatives with the identified mutation should continue to be screened for the clinical development of HCM. The development of clinically apparent disease may occur late in adulthood, so screening should be lifelong. Gene-negative relatives can be reassured that they do not have the disease-causing mutation and do not require further screening.[1][2][43][44]
Clinical variability exists despite identical gene mutations. The risk of sudden death may be low or high for the same mutation.[46]
Genetic counselling should be available for all patients who are offered genetic testing, to inform decision-making and ensure that results can be reviewed and their clinical significance appropriately determined.[1] The importance of potential psychologic, social, legal, ethical, and professional implications of having a genetic disease should also be discussed, and appropriate support provided.[2]
Antenatal genetic counselling should be offered to parents who have had a previous affected child with an inherited HCM due to a single or multiple pathogenic variant(s), or to couples where one or both partners carries a known pathogenic variant.[1][47] The risk of disease transmission should be discussed, as well as potential reproductive options (e.g., in-vitro fertilisation with preimplantation genetic diagnosis, antenatal genetic screening, and postnatal genetic testing).[2][43]
Advances in genetic sequencing technology and increased accessibility to testing have led to an increasing number of incidentally identified genetic variants associated with HCM. Interpreting the clinical relevance of such findings can be challenging; the American Heart Association has produced guidance on how to manage them, with emphasis on a multi-disciplinary team approach.[48] The American College of Medical Genetics and Genomics has recommended that cardiomyopathy-associated genes be evaluated for secondary findings whenever broad clinical sequencing is undertaken, regardless of the initial indication for testing.[49] There is currently no international consensus around this recommendation, however.[1]
Result
mutation in 1 of the identified genes
Use of this content is subject to our disclaimer