Investigations
1st investigations to order
therapeutic trial of parenteral thiamine
Test
Treatment with parenteral administration of thiamine should never be delayed if Wernicke's encephalopathy is suspected.
A positive diagnosis is often considered established if there is a manifest reversal of clinical signs with parenteral administration of thiamine administration, which is usually seen within a few hours or days.[26]
The degree of response will depend on the duration and severity of symptoms before correction of thiamine deficiency.
Result
clinical response to treatment (usually seen within hours or days)
serum thiamine
Test
Where possible, serum thiamine should be measured prior to treatment with parenteral administration of thiamine, however this should not delay its administration.[1] A normal thiamine level does not always exclude the condition as up to 8% of patients with Wernicke's encephalopathy may have a normal or high thiamine level.[70] In rare cases, this may be explained by mutations in thiamine metabolism and transport genes.
Result
serum thiamine: low (may be high or normal in a small number of patients)
MRI of brain
Test
The preferred imaging modality in the work-up of Wernicke's encephalopathy.[1][74][75][76]
Has been shown to have a sensitivity of 53% and a specificity of 93% in diagnosis.[74] On T2-weighted and fluid attenuated inversion recovery (FLAIR) sequences, edematous lesions that would appear as low-density abnormalities on CT appear as signal hyperintensities in affected regions.[76]
Typical MRI findings include symmetrical signal abnormalities in the periventricular thalamic region, hypothalamus, mammillary bodies, periaqueductal region, and floor of the fourth ventricle.[76]
Imaging characteristics may differ in patients without concurrent alcohol-use disorder. Selective involvement of cranial nerve nuclei, cerebellum, red nuclei, dentate nuclei, fornix, splenium, cerebral cortex, and basal ganglia typically characterise imagining in patients with non-alcoholic-related Wernicke's encephalopathy. In patients with a history of alcohol-use disorder, lesions may more commonly demonstrate contrast enhancement in the mamillary bodies and thalamus.[77][Figure caption and citation for the preceding image starts]: Fluid attenuated inversion recovery (FLAIR) MRI brain of patient with Wernicke's encephalopathyRamulu P, Moghekar A, Chaudhry V, et al. Wernicke's encephalopathy, Neurology 2002;59:846; used with permission [Citation ends].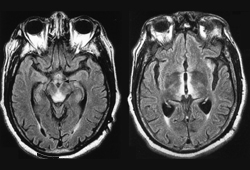
Result
typical MRI findings on T2-weighted and FLAIR sequences: symmetric hyperintensities within the mammillary bodies, dorsomedial nucleus of the thalami, periaqueductal grey matter, floor of the fourth ventricle, and cerebellar vermis
blood glucose
Test
May be abnormal in patients presenting with comorbidities.
Hypoglycaemia may be evident in patients with poor dietary intake, for example, secondary to chronic alcohol-use disorder.
Result
usually normal unless there are coexisting conditions (e.g., alcoholic liver disease, acute alcohol intoxication, sepsis, hypotension)
FBC
Test
An infection may trigger acute decompensation in a patient at risk for thiamine deficiency.
Result
usually normal unless WBC count elevated by concomitant infection
serum electrolytes
Test
Including magnesium, calcium, and phosphate.
Electrolytes may be deranged as a result of pre-existing conditions or malnutrition.
Hypotension may cause renal dysfunction and electrolyte abnormalities.
Magnesium is a key electrolyte; deficiency may impair the therapeutic benefit of thiamine as magnesium serves as a co-factor in enzymes involved in thiamine metabolism.[48]
Result
usually normal at presentation unless pre-existing conditions or malnutrition present; may be abnormal in late-stage disease
renal function
Test
Renal function may be deranged as a result of pre-existing conditions or malnutrition.
Hypotension and lactic acidosis may cause renal dysfunction.
Result
usually normal at presentation unless pre-existing conditions or malnutrition present; may be abnormal in late-stage disease
LFTs
Test
May be abnormal if patient has a history of alcohol-use disorder or has severe hypotension from unrecognised Wernicke's encephalopathy.
Result
usually normal at presentation; may be deranged if history of alcohol-use disorder
toxicology screen
Test
To exclude concomitant drug intake.
Result
negative
serum ammonia
Test
A metabolic encephalopathy due to hyperammonaemia can mimic Wernicke's encephalopathy.
Result
typically normal unless there is decompensation of coexistent alcoholic liver disease
blood alcohol level
Test
An elevated blood alcohol level may be evident in patients with alcohol-use disorder or acute alcohol intoxication.
Result
elevated levels may be found in patients with alcohol-use disorder or acute alcohol intoxication
Investigations to consider
lumbar puncture
Test
Its value is in excluding meningitis, encephalitis, and subarachnoid haemorrhage, which may present with similar findings.
The cerebrospinal fluid (CSF) is typically normal in most patients with Wernicke's encephalopathy. Elevated CSF protein may be seen in late cases.
Result
normal, excludes other pathology
Use of this content is subject to our disclaimer