Approach
The key to diagnosing ankylosing spondylitis (AS) is to identify the characteristics of inflammatory back pain.[6][9] Early referral to a specialist centre for comprehensive evaluation is essential. Treatments are available that may prevent accumulation of structural damage and ultimately disability. BMJ: identifying and referring spondyloarthritis (infographic) Opens in new window
History
AS usually manifests as back pain in people aged 20 years and older. Inflammatory back pain comprises a variety of symptoms, which can include:
Early morning back stiffness
Improvement of stiffness with exercise
Resolution of symptoms using non-steroidal anti-inflammatory drugs (NSAIDs)
Alternating buttock pain
Waking in the second half of the night with back pain.
At least two of these symptoms need to be present to be highly suggestive of inflammatory back pain. Refer patients with back pain that appears to be inflammatory and has lasted more than 3 months to a specialist with an interest in spondyloarthropathy.
Obtain further history to establish the presence of disease-associated features such as:
Iritis
Enthesitis (affecting tendon or ligament attachments to bone)
Family history of spondyloarthropathy
Psoriasis
Uveitis
Inflammatory bowel disease
Dyspnoea
Fatigue
Sleep disturbance.
Results from one systematic review and meta-analysis suggest that, with the exception of uveitis, peripheral and extra-articular manifestations of spondyloarthropathies are present to the same extent in those with AS or non-radiographical axial spondyloarthropathy.[80] Uveitis is more prevalent in those with AS.[80]
Physical examination
Findings on examination may include:
Loss of lumbar lordosis and flexion
Tenderness at sacroiliac joints
Kyphosis (in chronic cases)
Peripheral joint involvement.
A physical assessment of mobility includes:
Measuring the tragus-to-wall distance (distance between the tragus of the ear and the wall when the patient stands with his/her heels and back against the wall, chin retracted and head in the neutral position [i.e., no neck extension])
Lumbar flexion
Cervical rotation
Lumbar side-flexion
Intermalleolar distance.
These measurements are extrapolated to form a composite validated score known as the Bath Ankylosing Spondylitis Metrology Index (BASMI).[81] Bath Ankylosing Spondylitis Metrology Index (BASMI) Opens in new window
Investigations
There is no test that is diagnostic of AS.
A history suggestive of inflammatory back pain should prompt the clinician to request an x-ray of the pelvis to confirm the presence of radiographical sacroiliitis.[82] A negative radiograph does not exclude the diagnosis as radiographically apparent sacroiliitis may take many years to develop, and plain radiography has been demonstrated to have low sensitivity, but reasonable specificity, in diagnosis of sacroiliitis in patients with suspected axSpA.[83] Early referral to a rheumatologist, preferably one with a special interest in spondyloarthropathy, is critical at this point.[Figure caption and citation for the preceding image starts]: Plain x-ray showing bilateral sacroiliitis in a patient with ASBMJ 2006 Sep 16;333(7568):581-5. © BMJ Publishing Group Ltd 2009 [Citation ends].
If inflammatory back pain is diagnosed clinically but the patient has a normal pelvic x-ray, consider magnetic resonance imaging of the pelvis to look for inflammatory changes in the sacroiliac joints.[84][85] HLA-B27, although not diagnostic, is also helpful in this scenario, especially if it is positive.[Figure caption and citation for the preceding image starts]: Coronal STIR (short tau inversion recovery) magnetic resonance image showing unilateral (right) sacroiliitisBMJ 2006 Sep 16;333(7568):581-5. © BMJ Publishing Group Ltd 2009 [Citation ends].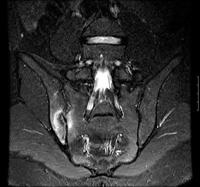
Other tests:
Radiographs of the cervical, thoracic, and lumbar spines should be performed at baseline once diagnosis is established
An ultrasound may be necessary to confirm and/or quantify the extent of enthesitis.
Bone scans are of limited diagnostic value.[86] Inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are generally unhelpful in diagnosing or monitoring AS.[87]
Baseline patient-completed outcome questionnaires
AS can be a progressive disease in a large percentage of patients, leading to long-term disability. Thus, it is important that patients be followed longitudinally, in order that those with poor outcomes are identified as early as possible.
Reliable prognostic markers in AS are lacking. Clinicians rely on clinical evaluation to assess a patient. Many if not most standard outcome measures for AS are patient-completed questionnaires. These have been validated for use in everyday practice. The Assessment in Ankylosing Spondylitis (ASAS) International Working Group has suggested that the following areas be assessed at regular intervals, at least annually, in every patient with AS:[88]
Patient global assessment
Spinal pain and stiffness
Spinal mobility
Physical function
Peripheral joints
Fatigue
The instruments ASAS recommend to assess the domains include the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) to assess disease activity and the Bath Ankylosing Spondylitis Functional Index (BASFI) to assess function.[89][90] Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) Opens in new window Bath Ankylosing Spondylitis Functional Index (BASFI) Opens in new window
Use of this content is subject to our disclaimer