Investigations
1st investigations to order
urinalysis
Test
Reagent strip testing can be used to screen for the presence of protein in the urine. Reagent strip testing with automated readers is more accurate than visual analysis. Proteinuria in association with elevated blood pressure in the pre-eclampsia range requires referral to a specialist unit or hospital admission for assessment.
Urinary protein can be estimated in a 24-hour urine collection. A urinary excretion of ≥300 mg of protein in 24 hours is diagnostic.[1][2][34]
The presence of proteinuria ≥5 g/24 hours is no longer used as a marker of severity, as the level of proteinuria does not relate to outcome.[1]
However, completing a 24-hour urine collection is awkward for women, and, if available, an alternative spot test such as protein:creatinine ratio (PCR, for which a result of ≥30 mg/mmol is diagnostic) is preferred.[1][16][34][54] If the proteinuria measurement is above the diagnostic threshold but there is still diagnostic uncertainty, consider re-testing on a new sample in addition to clinical review.
The presence of proteinuria is no longer mandatory in the diagnosis of pre-eclampsia; systemic involvement or fetal growth restriction together with hypertension are enough to fulfil the diagnosis, even in the absence of proteinuria.[1][2]
Result
positive reagent strip test; urinary excretion of ≥300 mg of protein in 24 hours; or urine protein:creatinine ratio ≥30 mg/mmol; may be normal
fetal ultrasound
Test
Provides immediate information about fetal wellbeing, including size of baby and amniotic fluid volume. If fetal movements are reduced, there is a need for immediate fetal ultrasound assessment.
[  ]
]
Fetal biometry should be used to diagnose or exclude fetal growth restriction. Growth can only be fully assessed by scans done 2 weeks apart.
Single scan can give an estimation of fetal weight and an assessment of whether the baby is small for dates, and gives the neonatologist important information about the need for immediate delivery.
Result
variable depending on severity; fetal biometry may reveal fetal growth restriction
umbilical artery Doppler velocimetry
Test
The main assessment tool; its use reduces perinatal mortality and supports better decision-making, leading to more appropriate delivery decisions. [Figure caption and citation for the preceding image starts]: Umbilical artery Doppler velocimetry: (1) normal pattern; (2) reduced end diastolic flow; (3) absent end diastolic flow; (4) reverse end diastolic flowFrom the personal collection of Dr James J. Walker; used with permission [Citation ends].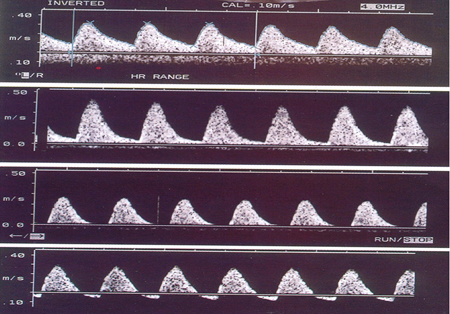
Should be carried out on admission and, if normal, repeated twice weekly.[16] Presence of end diastolic flow is reassuring.
If abnormal, more intensive monitoring may be required using other means, including Doppler assessment of other fetal vessels and fetal cardiotocography.
[  ]
Delivery is likely to be necessary within a few days.[16]
]
Delivery is likely to be necessary within a few days.[16]
New evidence suggests that placental vascular indices obtained from three-dimensional power Doppler may be predictive of pre-eclampsia. However, large studies are required to validate its use in the wider population.[62]
Result
absence of end diastolic flow is a sign that delivery will probably be necessary in the near future
amniotic fluid assessment
Test
Seems to be beneficial (rather than full biophysical profiling) with the single deepest vertical pocket being preferred over the amniotic index.
Easily combined with umbilical artery Doppler velocimetry.[1][16][54]
Can assess fetal wellbeing and inform about the need to deliver immediately.
Result
deepest vertical pocket ≥2 cm implies normality; <2 cm is associated with increased fetal morbidity and delivery should be considered
fetal cardiotocography
Test
Assesses immediate fetal wellbeing, but is of little prognostic value.
Should be used to assess fetal wellbeing initially, and then no more than twice weekly, unless there is a cause for concern such as vaginal bleeding, reduced fetal movements, or increased severity of disease.
[  ]
]
Result
no abnormalities in tracing indicate assured fetal wellbeing
FBC
Test
Useful indicator of disease progression and recommended in all women.
Decreased platelet count is partly diagnostic for HELLP syndrome. HELLP syndrome is a subtype of severe pre-eclampsia characterised by haemolysis (H), elevated liver enzymes (EL), and low platelets (LP).
If the platelet count is <100,000/microlitre, a full coagulation screen and blood film should be carried out to diagnose/exclude HELLP syndrome.
Result
may reveal low platelet count
liver function tests
Test
Useful indicator of disease progression and recommended in all women.
Increased transaminase levels are partly diagnostic for HELLP syndrome. HELLP syndrome is a subtype of severe pre-eclampsia characterised by haemolysis (H), elevated liver enzymes (EL), and low platelets (LP).
Result
may be elevated
serum creatinine
Test
Useful indicator of disease progression and recommended in all women.
Elevated serum creatinine implies underlying renal disease.
Renal failure is a rare complication, and when it occurs, it is usually acute tubular necrosis associated with co-existing sepsis or placental abruption.
Result
may be elevated
Investigations to consider
coagulation screen
Test
Usually normal in a woman with pre-eclampsia. May be abnormal with advanced disease affecting the liver, or in association with abruption.
Should also be carried out as an assessment of risk for interventions such as spinal or epidural analgesia, or surgical intervention where excessive bleeding may increase the morbidity or mortality risk.
Result
typically normal
Use of this content is subject to our disclaimer