Aetiology
The causative pathogen varies depending on the patient's age and other factors such as presence of immunocompromising conditions.[3]
In children and young people aged ≥3 months, the most common pathogens are Neisseria meningitidis (meningococcus) and Streptococcus pneumoniae (pneumococcus).[2][3] Haemophilus influenzae is no longer a major cause of bacterial meningitis following widespread introduction of the H influenzae type b (Hib) vaccine.[3][12] H influenzae meningitis may occur incidentally in unvaccinated children or may be due to serotypes other than type b.[3][14]
In neonates, the most common pathogens are Streptococcus agalactiae (group B streptococcus), and Escherichia coli.[1] S pneumoniae and Listeria monocytogenes account for a smaller proportion of cases.[1]
Patients who are immunosuppressed are also susceptible to meningitis caused by other organisms such as L monocytogenes, Cryptococcus neoformans, Nocardia species, and Toxoplasma gondii.[15]
The route of transmission varies depending on the causative organism.[16] N meningitidis, S pneumoniae, and H influenzae are carried in the nose and throat, and spread between people through respiratory droplets or throat secretions (nosocomial or horizontal transmission).[16] Group B streptococcus is usually carried in the gut or vagina and can spread from mother to child around the time of birth (vertical transmission).[16] The primary mode of transmission of early neonatal meningitis (occurring during the first week of life) is by vertical transmission through the birth canal.[3] However, in late neonatal meningitis (occurring between the second and sixth weeks) transmission is nosocomial or horizontal.[3][Figure caption and citation for the preceding image starts]: Gram-positive bacterium, Streptococcus pneumoniaeUS Centers for Disease Control and Prevention Public Health Image Library [Citation ends].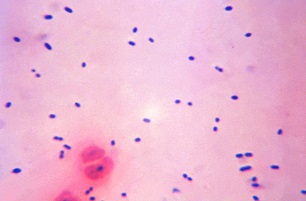
Pathophysiology
Bacteria reach the central nervous system either by haematogenous spread (the most common route) or by direct extension from a contiguous site such as the paranasal sinuses or the mastoid bone. Neonates can acquire pathogens from vertical transmission of maternal genital tract flora, through the placenta, or from their surroundings.[3][17] The bacteria multiply quickly once they have entered the subarachnoid space. Bacteria in the cerebrospinal fluid induce the production of various inflammatory mediators, which in turn enhance the influx of leukocytes into the cerebrospinal fluid.[18] The inflammatory cascade leads to cerebral oedema and increased intracranial pressure, which contribute to neurological damage and even death.
Classification
Common types of bacterial meningitis: children ≥3 months
Pneumococcal meningitis
Caused by Streptococcus pneumoniae[3]
Meningococcal meningitis
Caused by Neisseria meningitidis[3]
Common types of bacterial meningitis: children <3 months
Group B streptococcal meningitis
Caused by Streptococcus agalactiae[3]
Gram-negative meningitis
Caused by Escherichia coli and other gram-negative bacilli
Listeria meningitis
Caused by Listeria monocytogenes[3]
Use of this content is subject to our disclaimer