Investigations
1st investigations to order
non-contrast CT head
Test
Request brain imaging as soon as possible (at most within 1 hour of arrival at hospital).[30]
Practical tip
Aim to take a collateral history from relatives regarding medications/past medical history while the patient is in the scanner.
[Figure caption and citation for the preceding image starts]: Intracranial haemorrhage on CT scanMassachusetts General Hospital personal case files; used with permission [Citation ends].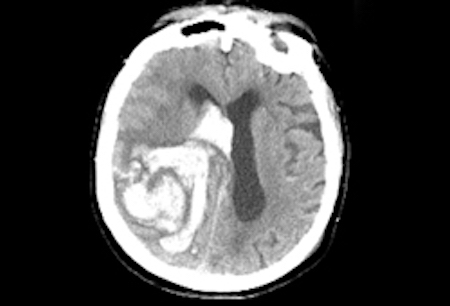
Use an urgent non-enhanced CT head to differentiate between ischaemic stroke and ICH, which must be done before reversing anticoagulation in anticoagulation-induced ICH and before starting thrombolysis in ischaemic stroke.[23][30][56] See Ischaemic stroke.
Result
hyperattenuation (brightness), suggesting acute blood, often with surrounding hypoattenuation (darkness) due to oedema
serum glucose
serum electrolytes
Test
To exclude electrolyte disturbance (e.g., hyponatraemia) as a cause for neurological signs.
Result
may be normal; may show electrolyte disturbances
serum urea and creatinine
Test
To exclude renal failure because it may be a potential contraindication to some stroke interventions.
Result
may be normal; may show renal failure
liver function tests
Test
To exclude liver dysfunction as a cause of haemorrhage.
Significant liver dysfunction can seriously compromise the coagulation system and induce bleeding, and also promote the development of cerebral oedema (mainly due to impaired ammonia metabolism) and intracranial hypertension, especially in cases of acute liver failure.
Result
may be normal; may show liver dysfunction
FBC
Test
To exclude thrombocytopenia as a cause of haemorrhage.
Thrombocytopenia suggests a secondary cause of haemorrhage.
Result
may be normal; may show anaemia or thrombocytopenia
clotting screen
Test
To exclude coagulopathy as a cause of haemorrhage.
Check INR or factor Xa levels, if available.
If elevated, results suggest a secondary cause of haemorrhage.
Result
usually normal
ECG
Test
To assess for active coronary ischaemia or prior cardiac injury; ECG abnormalities can indicate concomitant myocardial injury.[23]
Result
may be normal; may show arrhythmia or signs of ischaemia
Investigations to consider
serum toxicology screen
Test
Consider a toxicology screen if you suspect use of toxic substances. Signs and symptoms may mimic stroke.
Cocaine and other sympathomimetic drugs are associated with ICH, especially in younger people.[23]
Result
may exclude alcohol and drug ingestion
CT angiography (CTA) or magnetic resonance angiography (MRA) head
Test
Consider for all patients with acute spontaneous intracerebral haemorrhage aged 18-70 years who were independent, without a history of cancer, not taking an anticoagulant, except if they are aged more than 45 years with hypertension and the haemorrhage is in the basal ganglia, thalamus, or posterior fossa.[30] If this early CTA/MRA is normal or inconclusive, MRI/MRA with susceptibility-weighted imaging (SWI) should be considered at 3 months. Early CTA/MRA and MRI/MRA at 3 months may also be considered in patients not meeting these criteria where the probability of a macrovascular cause is felt to justify further investigation.
Result
arteriovenous malformation, dural arteriovenous fistula, or intracranial aneurysm
CT venography or magnetic resonance venography head
Test
Consider in patients with intracerebral haemorrhage in whom the haemorrhage location or other imaging features suggest cerebral venous thrombosis.[30]
Result
cerebral venous thrombosis
Intra-arterial cerebral angiography
Test
The DIAGRAM score (or its components: age; intracerebral haemorrhage location; CTA result where available; and the presence of white matter low attenuation [leukoaraiosis] on the admission non-contrast CT) should be considered to determine the likelihood of an underlying macrovascular cause and the potential benefit of intra-arterial cerebral angiography.[30]
Result
arteriovenous malformation, dural arteriovenous fistula, or intracranial aneurysm
Use of this content is subject to our disclaimer