Approach
Most cases of folliculitis present with a history of lesions in a hair-bearing area and do not require diagnostic tests.
Physical examination typically reveals erythematous lesions around the ostia of the hair follicles.
Diagnosis is almost always clinical although laboratory tests requested include skin swabs sent for bacterial fungal culture. If herpetic infection is suspected, swabs may also be sent for viral polymerase chain reaction (PCR). Skin biopsy may be considered in persistent or unusual cases (e.g., if eosinophilic folliculitis is suspected).
History
Patients with folliculitis typically present with multiple erythematous, folliculocentric papules and pustules in the hair-bearing regions. Most cases of superficial folliculitis are associated with pruritus and only mild discomfort. However, when the inflammatory infiltrate extends deeply and becomes extensive, painful furuncles or carbuncles can form.[Figure caption and citation for the preceding image starts]: Superficial folliculitis of chin due to S aureusFrom the personal collection of Professor Baden, MD [Citation ends].
Physical examination
Physical examination reveals erythematous papules, pustules, or cysts around the ostia of the hair follicles, with or without the presence of a hair shaft extending from the ostia. The papules may be eroded or have crusts. When the inflammation extends to several contiguous hair follicles, the papules may coalesce to form large carbuncles. It is important to recognise folliculitis primarily involving the scalp (e.g., folliculitis decalvans). In people with dark skin tone, folliculitis lesions often resolve with significant post-inflammatory hyperpigmentation, which can take months to years to fade completely.[Figure caption and citation for the preceding image starts]: Superficial folliculitis with prominent erythematous papules and pustulesFrom the personal collection of Professor Baden, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Folliculitis of the scalpFrom the personal collection of Professor Baden, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Folliculitis of the scalpFrom the personal collection of Professor Baden, MD [Citation ends].
Staphylococcus aureus folliculitis
The superficial form of S aureus folliculitis (impetigo of Bockhart) typically presents in the bearded distribution and the upper lip. The lesions appear as erythematous papules and pustules that are eroded or crusted. When the infection and inflammation involve deeper portions of the follicles, the condition is termed sycosis barbae and is characterised by indurated, erythematous nodules, and plaques.[Figure caption and citation for the preceding image starts]: Bacterial folliculitis of chin due to S aureusFrom the personal collection of Professor Baden, MD [Citation ends].
Gram-negative folliculitis
Gram-negative folliculitis typically affects patients with acne treated with oral antibiotics, and is associated with infection with Klebsiella, Enterobacter or Proteus species. Patients present with multiple small pustules on the cheeks, chin and perinasal regions.
Hot tub folliculitis is most commonly caused by Pseudomonas aeruginosa. About 2 to 3 days after immersion in a hot tub, multiple, large, erythematous papules and pustules on the trunk or areas occluded by swimwear tend to emerge. [Figure caption and citation for the preceding image starts]: Hot tub folliculitis due to P aeruginosaFrom the personal collection of Professor Baden, MD [Citation ends].
Fungal folliculitis
Dermatophytic folliculitis includes tinea capitis, tinea barbae, and Majocchi granuloma.
Tinea capitis can present as alopecia with scaling of the scalp, brittle hair breaking off at the surface of the scalp, or occasionally an erythematous, boggy plaque known as a kerion.[26]
Tinea barbae is most commonly seen in male farmers and affects the chin and the submaxillary region.[27]
Majocchi granuloma refers to a deep fungal folliculitis involving the entire hair follicle. It is most commonly caused by Trichophyton rubrum. Majocchi granuloma exists in 2 clinical forms.[23] In the follicular form, it occurs on the upper thighs of people who shave, and it is sometimes associated with tinea cruris. In the subcutaneous nodular form, Majocchi granulomas are found in immunocompromised hosts, such as those undergoing bone marrow or organ transplantation and those receiving long-term suppressive therapy for leukaemia or lymphoma.[23]
Malassezia folliculitis (Pityrosporum folliculitis) is caused by Malassezia furfur, and occurs most commonly in young adults, those living in tropical climates, and immunosuppressed individuals. Malassezia folliculitis presents as monomorphic, intensely pruritic papules on the upper back, upper arms, and chest.[28] Folliculitis caused by Candida species may occur on the backs of bedridden patients or areas of skin occluded by dressing. It has also been reported in patients who use heroin.[26][Figure caption and citation for the preceding image starts]: Fungal folliculitis: a kerionFrom the personal collection of Professor Baden, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Pityrosporum folliculitisFrom the personal collection of Professor Baden, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Pityrosporum folliculitisFrom the personal collection of Professor Baden, MD [Citation ends].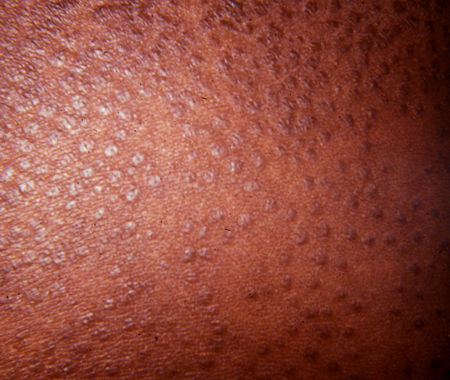
Viral folliculitis
Herpetic folliculitis, caused by Herpes simplex 1 (HSV1) or Herpes simplex 2 (HSV2), occurs most commonly in the beard region in men. It is typically spread to adjacent areas by shaving. Molluscum sycosis refers to the presence of multiple umbilicated, skin-coloured papules in the beard region as a result of Molluscum contagiosum infection.[29]
Varicella zoster primarily affects the hair follicles, but clinically presents as erythematous plaques with haemorrhagic crusts in a dermatomal distribution.
Demodex folliculitis
Demodex folliculitis, caused by a saprophytic parasitic mite, manifests as erythematous papules or pustules, against a background of diffuse erythema, typically occurring on the face. The papules sometimes show perifollicular scaling. However, the diagnosis of Demodex folliculitis is difficult due to the clinical resemblance to other common conditions, such as rosacea or acne. When a thorough work-up for other infectious aetiologies has not yielded an infectious pathogen, consider the diagnosis of Demodex folliculitis.[30] Alternatively, consider a referral to a dermatologist for further evaluation.
Folliculitis decalvans
Folliculitis decalvans is a rare form of folliculitis that occurs on the scalp and predominantly involves the vertex and occipital regions. Clinically, folliculitis decalvans presents with painful and recurrent purulent follicular exudation resulting in scarred and atrophic alopecic patches with red and inflamed margins. Surviving hairs may group so that they protrude from a single follicular opening (known as tufted hairs).[14]
Drug-induced folliculitis
This condition develops secondary to drugs such as corticosteroids, androgenic hormones, epidermal growth factor receptor inhibitors, halogenated drugs, lithium, isoniazid, and corticotrophin.[5][6][7]
It most commonly affects those prone to acne. Within 2 weeks of starting the offending drug, patients present with an acute onset of monomorphic erythematous, folliculocentric papules and pustules on the shoulders, torso and upper arms.
Eosinophilic pustular folliculitis (Ofuji disease)
This subtype is characterised by recurrent, intensely pruritic papules and pustules that develop in an explosive fashion, typically on the face, back, and arms.[1] It can also present with erythematous patches with central clearing, which appear as annular and serpiginous lesions. Lesions spontaneously resolve in 7 to 10 days but tend to recur in 3 to 4 weeks. Peripheral eosinophilia may be seen with this condition.
HIV-associated eosinophilic folliculitis
HIV-associated eosinophilic folliculitis is seen in patients with HIV, usually with low CD4+ count <300 cells/mm³.[2] Clinically, this condition is characterised by chronic, intensely pruritic, oedematous folliculocentric papules involving the upper torso and the head.
Eosinophilic pustular folliculitis in infancy
Eosinophilic pustular folliculitis in infancy presents as pustules and vesicles primarily involving the scalp. The lesions often have an erythematous base and crusting. The condition is self-limiting but can recur in cycles of 3 months to 5 years.[3][4]
Investigations
The diagnosis of folliculitis is primarily made on clinical grounds based on history and physical examination. However, cases that are resistant to therapy warrant further laboratory and histological investigation. Laboratory evaluation includes Gram stain, potassium hydroxide (KOH) preparation, Tzanck smear, culture for micro-organisms, and skin biopsy.
Bacterial skin swab
When a bacterial aetiology is suspected, the physician can unroof a pustule with a No.15 blade and deposit the contents onto a glass slide for PCR or Gram stain and bacterial culture.
Nasal, groin, and axillary swab cultures may be obtained for patients who have recurrent S aureus folliculitis to check for colonisation.
Viral skin swab
PCR for herpes simplex virus (HSV) or Tzanck smear is sometimes useful for suspected HSV folliculitis. However, direct fluorescent antibody testing for Herpes simplex and Varicella zoster viruses or skin biopsies are a fast and accurate means of diagnosing viral folliculitis. Some clinicians have suggested performing PCR on lesional skin can identify HSV and Varicella zoster DNA.[31][32]
Skin scraping for mycology
PCR or KOH preparations are helpful in diagnosing most dermatophytic infections, whereas skin biopsy is best to visualise Pityrosporum yeast forms.
Skin biopsy and histology
Skin biopsies can also help identify non-infectious folliculitis, such as eosinophilic folliculitis. In bacterial and fungal folliculitis, skin biopsies typically show follicular infiltration of neutrophils, with variable admix of lymphocytes and macrophages depending on the chronicity of folliculitis. Micro-organisms can often be appreciated within the hair follicle. In viral folliculitis, a predominantly lymphocytic infiltrate surrounds the hair follicle.
The histological presentation of Ofuji disease shows exocytosis of eosinophils into a spongiotic follicular infundibulum and accompanying sebaceous gland, ultimately forming eosinophilic micropustules.[33]
The histological presentation of HIV-associated eosinophilic folliculitis is similar to that of Ofuji disease.
In eosinophilic pustular folliculitis in infancy, the inflammatory infiltrate may not invade the sebaceous glands or the outer root sheath of the hair follicle.
The histology of drug-induced folliculitis can appear similar to acute superficial folliculitis.[7] However, lack of micro-organisms in the hair follicle, the presence of sterile pustules, and recent history of drug ingestion help differentiate drug-induced folliculitis.
Use of this content is subject to our disclaimer