The overall goal of treatment is to manage wounds properly in order to prevent morbidity and mortality; this includes prevention and/or treatment of infectious complications. Animal scratches such as superficial tooth scratches should be treated as bite wounds, as they are often contaminated with saliva. However, common superficial claw scratches, such as cat scratches, do not require bite wound treatment.
Wound care
All animal bites should be considered contaminated and require wound care. The affected skin surface should be cleaned and the unclosed wound copiously irrigated with water, normal saline, or lactated Ringer's solution under high pressure (with an 18- or 19-gauge needle or catheter tip and large syringe).[39]Ellis R, Ellis C. Dog and cat bites. Am Fam Physician. 2014 Aug 15;90(4):239-43.
https://www.aafp.org/afp/2014/0815/p239.html
http://www.ncbi.nlm.nih.gov/pubmed/25250997?tool=bestpractice.com
[40]Evgeniou E, Markeson D, Iyer S, et al. The management of animal bites in the United kingdom. Eplasty. 2013 Jun 10;13:e27.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681434
http://www.ncbi.nlm.nih.gov/pubmed/23837110?tool=bestpractice.com
Irrigation with a dilute povidone-iodine solution may also be considered, particularly if the animal is believed to be rabid.[31]Morgan M, Palmer J. Dog bites. BMJ. 2007 Feb 24;334(7590):413-7.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1804160
[41]Centres for Disease Control and Prevention. Rabies postexposure prophylaxis (PEP): what medical care will I receive if I may have been exposed to rabies? May 2022 [internet publication].
https://www.cdc.gov/rabies/medical_care/index.html
Devitalised or necrotic tissue should be debrided and abscesses drained.
Clenched fist injuries require special consideration. A hand specialist should evaluate these injuries for penetration into the synovium, joint capsule, and bone. These wounds may extend deeply and carry organisms in the deep compartments and potential spaces of the hand. Antibiotic prophylaxis is recommended in all cases.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
Wound closure and repair
Wound closure is a controversial issue. There is general agreement that infected wounds and those seen >24 hours after the bite should be left open. Some physicians recommend consideration of wound closure after irrigation and debridement in patients presenting <8 hours after the injury, if there is no visible evidence of infection.
Wounds with a high risk of complication or infection, such as limb wounds, should be left open. In wounds where there are significant cosmetic concerns, such as facial wounds, primary closure is often undertaken by a plastic surgeon or other expert.[43]Xiaowei Z, Wei L, Xiaowei H, et al. Comparison of primary and delayed wound closure of dog-bite wounds. Vet Comp Orthop Traumatol. 2013;26(3):204-7.
http://www.ncbi.nlm.nih.gov/pubmed/23460356?tool=bestpractice.com
[44]Rui-feng C, Li-song H, Ji-bo Z, et al. Emergency treatment on facial laceration of dog bite wounds with immediate primary closure: a prospective randomized trial study. BMC Emerg Med. 2013;13(suppl 1):S2.
http://www.biomedcentral.com/1471-227X/13/S1/S2
http://www.ncbi.nlm.nih.gov/pubmed/23902527?tool=bestpractice.com
[45]Paschos NK, Makris EA, Gantsos A, et al. Primary closure versus non-closure of dog bite wounds. A randomised controlled trial. Injury. 2014 Jan;45(1):237-40.
http://www.ncbi.nlm.nih.gov/pubmed/23916901?tool=bestpractice.com
[46]Chen E, Hornig S, Shepherd SM, et al. Primary closure of mammalian bites. Acad Emerg Med. 2000 Feb;7(2):157-61.
http://www.ncbi.nlm.nih.gov/pubmed/10691074?tool=bestpractice.com
The decision around primary wound closure weighs function and cosmesis against infection, and should be shared between clinician and patient.[10]Colmers-Gray IN, SP Tulloch JSP, Dostaler G, et al. Management of mammalian bites. BMJ. 2023 Feb 02;380:e071921. One 2019 Cochrane systematic review on dog bites found no indication that primary closure reduces infection rates or has an impact on cosmesis, based on weak evidence.[10]Colmers-Gray IN, SP Tulloch JSP, Dostaler G, et al. Management of mammalian bites. BMJ. 2023 Feb 02;380:e071921.[47]Bhaumik S, Kirubakaran R, Chaudhuri S. Primary closure versus delayed or no closure for traumatic wounds due to mammalian bite. Cochrane Database Syst Rev. 2019 Dec 6;12(12):CD011822.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011822.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/31805611?tool=bestpractice.com
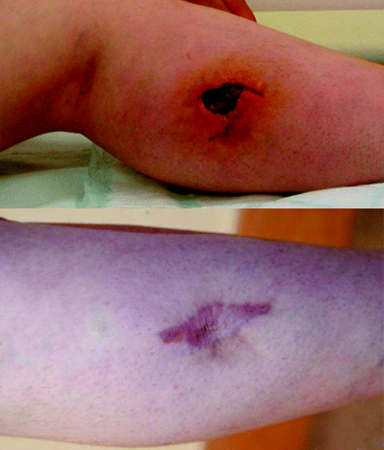
[Figure caption and citation for the preceding image starts]: Top: breakdown of a leg bite wound and infection seven days after it was sutured in primary care. Bottom: resultant scarring 18 months laterMorgan M, Palmer J. BMJ 2007;334:413 doi:10.1136/bmj.39105.659919.BE [Citation ends].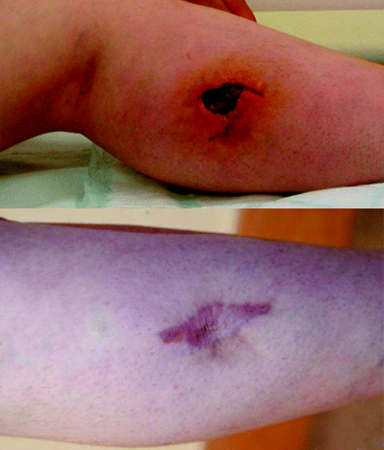
If wounds are complicated by fractures, communication into the joint space, loss of a significant amount of tissue, disruption of deep anatomical structures, or are serious hand or cranial bites, then orthopaedic or surgical consultation is required.
Prophylactic antibiotics for uninfected bite wounds
The indications for antibiotics as prophylaxis are unclear, and their effectiveness is uncertain.[10]Colmers-Gray IN, SP Tulloch JSP, Dostaler G, et al. Management of mammalian bites. BMJ. 2023 Feb 02;380:e071921.[48]Callaham M. Prophylactic antibiotics in dog bite wounds: nipping at the heels of progress. Ann Emerg Med. 1994 Mar;23(3):577-9.
http://www.ncbi.nlm.nih.gov/pubmed/8135437?tool=bestpractice.com
[49]Cummings P. Antibiotics to prevent infection in patients with dog bite wounds: a meta-analysis of randomized trials. Ann Emerg Med. 1994 Mar;23(3):535-40.
http://www.ncbi.nlm.nih.gov/pubmed/8135429?tool=bestpractice.com
[50]Jones N, Khoosal M. Infected dog and cat bites. N Engl J Med. 1999 Jun 10;340(23):1841.
http://www.ncbi.nlm.nih.gov/pubmed/10366325?tool=bestpractice.com
[51]Mederios I, Saconato H. Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev. 2001;(2):CD001738.
http://www.ncbi.nlm.nih.gov/pubmed/11406003?tool=bestpractice.com
[52]Henton J, Jain A. Cochrane corner: antibiotic prophylaxis for mammalian bites (intervention review). J Hand Surg Eur Vol. 2012 Oct;37(8):804-6.
http://www.ncbi.nlm.nih.gov/pubmed/23042781?tool=bestpractice.com
Prophylactic (also known as pre-emptive) antibiotics are recommended in all cases of clenched fist injury and should be considered in patients with factors that increase the likelihood of infection, or have serious implications of infection.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
Wound factors include:[14]Greene SE, Fritz SA. Infectious complications of bite injuries. Infect Dis Clin North Am. 2021 Mar;35(1):219-36.
http://www.ncbi.nlm.nih.gov/pubmed/33494873?tool=bestpractice.com
[31]Morgan M, Palmer J. Dog bites. BMJ. 2007 Feb 24;334(7590):413-7.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1804160
[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
Bites to the hand, head, neck, or genital region
Puncture or crush wounds
Deep structure involvement or requiring surgical repair
Bite or laceration from a human or cat that results in broken skin
Wounds over or near bone, tendons, ligaments, or joints
Limbs with impaired vasculature or lymphatic return.
Patient factors include:[14]Greene SE, Fritz SA. Infectious complications of bite injuries. Infect Dis Clin North Am. 2021 Mar;35(1):219-36.
http://www.ncbi.nlm.nih.gov/pubmed/33494873?tool=bestpractice.com
[31]Morgan M, Palmer J. Dog bites. BMJ. 2007 Feb 24;334(7590):413-7.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1804160
[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
Previous medical procedures, for example, splenectomy or lymph node removal
Underlying medical conditions, for example, advanced liver disease, diabetes mellitus, or other immunosuppressive conditions.
For a single, uninfected animal bite to a person with no penicillin allergy, treatment with agents that cover both aerobic and anaerobic bacteria (e.g., a beta-lactam, or a second- or third- generation cephalosporin plus clindamycin or metronidazole) may be considered.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
With penicillin allergy, treatment with a combination of agents, including clindamycin or metronidazole plus a sulfonamide (e.g., trimethoprim/sulfamethoxazole) or a fluoroquinolone (e.g., ciprofloxacin, levofloxacin), is an alternative option.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
The combination of doxycycline plus metronidazole may also be considered.[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
[54]Dendle C, Looke D. Management of mammalian bites. Aust Fam Physician. 2009 Nov;38(11):868-74.
https://www.racgp.org.au/afp/2009/november/mammalian-bites
http://www.ncbi.nlm.nih.gov/pubmed/19893832?tool=bestpractice.com
Moxifloxacin has good anaerobic cover and may be considered as a single agent in patients with penicillin allergy.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
For pregnant women, azithromycin and metronidazole is an option. Always seek consultant advice before prescribing.[55]The British Association for Forensic Odontology. Management of injuries caused by teeth. May 2021 [internet publication].
https://fflm.ac.uk/wp-content/uploads/2021/05/Management-of-Injuries-caused-by-teeth-May-2021.pdf
In general, prophylactic therapy is given for 3 to 5 days.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
It is recommended that local guidance for antimicrobial therapy is used where available.
Treatment of infected single bite wounds
Antibiotic therapy is indicated in patients with overt signs of infection. People with a single, uncomplicated, infected bite with the infecting organism unknown, and who are not allergic to penicillin, should be treated with agents that cover both aerobic and anaerobic bacteria (e.g., a beta-lactam, or a second- or third-generation cephalosporin plus clindamycin or metronidazole).[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
Those who are penicillin-allergic should receive a combination of agents, including clindamycin or metronidazole plus a sulfonamide (e.g., trimethoprim/sulfamethoxazole) or a fluoroquinolone (e.g., ciprofloxacin, levofloxacin).[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
The combination of doxycycline plus metronidazole is also an option.[53]National Institute for Health and Care Excellence. Human and animal bites: antimicrobial prescribing. November 2020 [internet publication].
https://www.nice.org.uk/guidance/ng184
[54]Dendle C, Looke D. Management of mammalian bites. Aust Fam Physician. 2009 Nov;38(11):868-74.
https://www.racgp.org.au/afp/2009/november/mammalian-bites
http://www.ncbi.nlm.nih.gov/pubmed/19893832?tool=bestpractice.com
Moxifloxacin has good anaerobic cover and can be used as a single agent in patients with penicillin allergy.[42]Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
http://cid.oxfordjournals.org/content/59/2/e10.full
http://www.ncbi.nlm.nih.gov/pubmed/24973422?tool=bestpractice.com
No standard guidelines exist for length of therapy, but treatment of established uncomplicated infection is usually 10 to 14 days.[14]Greene SE, Fritz SA. Infectious complications of bite injuries. Infect Dis Clin North Am. 2021 Mar;35(1):219-36.
http://www.ncbi.nlm.nih.gov/pubmed/33494873?tool=bestpractice.com
Treatment of complicated bites
Hospital admission for parenteral therapy should be considered for patients with:
Multiple or severe bites
Severe local infection
Evidence of systemic infection
Joint or bone involvement
Severe underlying illnesses or immunocompromising conditions.
No standard guidelines exist for length of therapy, but treatment of 10 to 14 days of therapy is recommended for localised infection (e.g., cellulitis, skin abscess), whereas complex infections (including osteomyelitis) may need to continue for 4 to 6 weeks.[14]Greene SE, Fritz SA. Infectious complications of bite injuries. Infect Dis Clin North Am. 2021 Mar;35(1):219-36.
http://www.ncbi.nlm.nih.gov/pubmed/33494873?tool=bestpractice.com
Post-exposure prophylaxis
Post-exposure prophylaxis (PEP) for transmissible diseases, especially rabies and tetanus, should be considered.[38]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases - rabies. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/rabies
[56]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases - tetanus. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/tetanus
See Rabies and Tetanus.
Notification of public health/law enforcement
Local law enforcement and/or public health departments may need to be contacted about a bite injury. Local practices and regulations vary.[18]Manning SE, Rupprecht CE, Fishbein D, et al. Advisory Committee on Immunization Practices Centers for Disease Control and Prevention (CDC). Human rabies prevention - United States, 2008: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2008 May 23;57(RR-3):1-28.
http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5703a1.htm
http://www.ncbi.nlm.nih.gov/pubmed/18496505?tool=bestpractice.com
[38]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases - rabies. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/rabies
These agencies may be helpful in animal bite investigation, post-bite rabies quarantines, identification and regulation of feral animals, and public health reporting.