Investigations
1st investigations to order
serum acetylcholine receptor (AChR) antibody analysis
Test
Results may vary between laboratories and assay techniques.
Antibodies against AChR are detectable in 80% to 90% of patients with generalised MG and up to 50% of patients with ocular MG, with 99% specificity in both cases.[70]
Low-binding titres are rarely seen in patients with other autoimmune diseases including Lambert-Eaton myasthenic syndrome (LEMS) and neuromyelitis optica spectrum disorder (NMOSD).
A cell-based assay for AChR antibodies using clustered receptors identifies patients with MG who in general appear similar to patients identified by standard AChR binding and modulating assays, with an increased percentage of pre-pubertal onset disease.[73]
Result
positive (titre above reference range; varies with assay used)
muscle-specific tyrosine kinase (MuSK) antibodies
Test
MuSK antibody assay is performed if standard serum acetylcholine receptor (AChR) antibody analysis is negative or equivocal.
Positive test in up to 70% of patients with generalised MG who are seronegative for AChR antibodies.[5][62] Cell-based assays may increase the percentage of positive results.[25]
In the US, MuSK antibodies are common in the black population; 70% of black women with generalised seronegative MG have MuSK antibodies.[5]
Consider testing earlier in patients with classic phenotype.
Result
may be positive
serial pulmonary function tests
Test
Indicated for patients with shortness of breath and suspected myasthenic crisis or pre-crisis.
Serial measurements of forced vital capacity (FVC) and negative inspiratory force (NIF) are taken. Indications for mechanical ventilation are FVC 15 mL/kg or less (normal ≥60 mL/kg) and/or NIF of 20 cm H₂O or less (normal ≥70 cm H₂O).
Physicians should not wait for abnormal arterial blood gas (ABG) as it occurs late in the course after clinical decompensation. Arterial pCO₂ is elevated before any changes are seen in pO₂ or O₂ saturation.
Result
myasthenic crisis: low FVC and low NIF
Investigations to consider
striational receptor antibody assays
repetitive nerve stimulation
Test
If serological testing is unremarkable, electrophysiological testing should be performed.
Sensitivity: 79% in generalise MG, 50% in ocular MG. Specificity: 97%.[70]
Brief exercise of a muscle prior to the test may enhance decrement response.
Positive decrement also seen in Lambert-Eaton myasthenic syndrome (LEMS) and amyotrophic lateral sclerosis (ALS). Patients with LEMS improve with rapid stimulation; patients with ALS have characteristic findings on electromyogram.
In MuSK-MG, generally the abnormal result yield is high in proximal muscles: for example, the trapezius, deltoid, and facial muscles. For patients with neck and respiratory weakness, it is important to evaluate clinically affected muscles as the test may be normal in limb and face muscles.[5]
Result
>10% decline in compound muscle action potential (CMAP) amplitude between the first and fourth potential in a train of 10 stimulations of the motor nerve at 2 to 3 Hz is considered a positive response
single-fibre EMG
Test
If repetitive nerve stimulation is negative or equivocal, single-fibre EMG (SFEMG) is recommended.
Sensitivity 86% to 92% and specificity 70% to 96% in facial muscles in ocular MG; sensitivity and specificity 98% in generalised MG.[70]
Abnormal test may be seen in Lambert-Eaton myasthenic syndrome (LEMS) and amyotrophic lateral sclerosis (ALS), inflammatory myopathies, or patients injected with botulinum toxin. Therefore it is important to ensure that muscles have been tested with needle examination.
Test is not specific for MG, and it is important to be certain that there is no evidence of denervation or myopathy in the tested muscles.
Result
increased variability in motor latencies (jitter) or complete failure of neuromuscular transmission (block) in some muscle fibres
CT of chest
Test
Should be performed in all newly diagnosed patients with adult onset MG to detect thymoma (which occurs in about 15% of patients with MG) or thymic hyperplasia (which occurs in 75% of MG patients). [Figure caption and citation for the preceding image starts]: Computed tomography showing anterior mediastinal massHamid UI, Jones JM. Mediastinal mass. BMJ Case Reports 2010 Oct 4;2010:bcr1120092471. [Citation ends].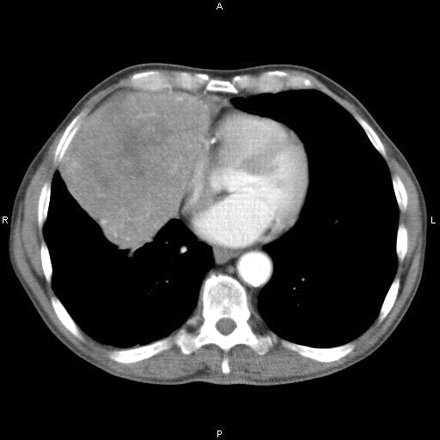
Result
thymic enlargement
Use of this content is subject to our disclaimer