Investigations
1st investigations to order
reverse transcriptase-polymerase chain reaction (RT-PCR)
Test
Non-pregnant symptomatic individuals: the Centers for Disease Control and Prevention (CDC) currently recommends testing for people living in or with recent travel to an area with an active CDC Zika travel health notice, or to an area with current or past Zika transmission outside of the US and its territories. Testing should be performed on serum collected ≤7 days after symptom onset. Routine testing is not currently recommended in non-pregnant asymptomatic individuals.[161]
Pregnant asymptomatic women: the CDC currently recommends considering testing for pregnant women with recent travel to an area with an active Zika travel health notice during pregnancy, up to 12 weeks after travel. Routine testing is not currently recommended in pregnant asymptomatic women who do not meet these criteria.[161]
Pregnant symptomatic women: the CDC currently recommends testing for these women if certain epidemiological criteria are met. Specimens (both serum and urine) should be collected as soon as possible after the onset of symptoms, up to 12 weeks after symptom onset. If the test is positive, it should be repeated on newly extracted RNA from the same specimen to rule out a false-positive result.[161]
Pregnant with antenatal ultrasound findings consistent with congenital Zika virus infection: the CDC currently recommends testing for women who have lived in or travelled to an area with an active CDC Zika travel health notice or current or past Zika virus transmission during pregnancy, or had sex with someone who lived in or travel to an area with an active CDC Zika travel health notice or current or past Zika virus transmission during pregnancy. Recommended specimens are maternal serum and urine.[161]
Infants: CDC currently recommends testing in infants with clinical findings consistent with congenital Zika syndrome born to mothers with possible Zika virus exposure in pregnancy (regardless of maternal testing results), or infants without clinical findings consistent with congenital Zika syndrome who were born to mothers with laboratory evidence of possible Zika virus infection. Serum and urine should be collected from the infant in the first 2 days of life if possible (note: specimens collected within the first few weeks to months after birth still may be useful, especially in infants born in areas without risk of Zika).[2] Cerebrospinal fluid testing can be considered in infants with clinical findings of possible congenital Zika syndrome but whose initial laboratory tests on serum and urine are negative.[2]
Testing recommendations may differ between guidelines and locations.[162][171] Consult your local guidance.
Result
positive for Zika virus RNA
serology
Test
Non-pregnant symptomatic individuals: the CDC currently recommends Zika and dengue IgM antibody testing on RT-PCR-negative serum specimens and serum collected >7 days after onset of symptoms. If either Zika or dengue IgM antibody testing is positive, plaque-reduction neutralisation testing (PRNT) should be performed against Zika, dengue, and other flaviviruses endemic to the region where exposure occurred to confirm the diagnosis (if confirmation is required).[161]
Pregnant symptomatic women: the CDC currently recommends Zika and dengue IgM antibody testing (at the same time as RT-PCR) for these women if certain epidemiological criteria are met. If either antibody test is positive (and Zika and dengue RT-PCR is negative), PRNT should be performed against Zika, dengue, and other flaviviruses endemic to the region where exposure.[161]
Pregnant with antenatal ultrasound findings consistent with congenital Zika virus infection: the CDC currently recommends Zika IgM antibody testing for women who have lived in or travelled to an area with an active CDC Zika travel health notice or current or past Zika virus transmission during pregnancy, or had sex with someone who lived in or travel to an area with an active CDC Zika travel health notice or current or past Zika virus transmission during pregnancy. The recommended specimen is maternal serum. If serology is positive (and Zika RT-PCR is negative), confirmatory PRNT testing should be performed for Zika and dengue.[161]
Infants: the CDC currently recommends testing in infants with clinical findings consistent with congenital Zika syndrome born to mothers with possible Zika virus exposure in pregnancy (regardless of maternal testing results), or infants without clinical findings consistent with congenital Zika syndrome who were born to mothers with laboratory evidence of possible Zika virus infection. Serum should be collected from the infant in the first 2 days of life if possible (note: specimens collected within the first few weeks to months after birth still may be useful, especially in infants born in areas without risk of Zika). A positive result (with positive RT-PCR) confirms infection. A non-negative result (with negative RT-PCR) indicates probable infection.[2]
Testing recommendations may differ between guidelines and locations.[162][171] Consult your local guidance.
Result
positive for Zika virus IgM antibodies; PRNT ≥10
testing for other arboviruses
Test
It is important to differentiate between Zika, dengue, and chikungunya virus infection as the three diseases can produce similar symptoms, particularly during the acute phase.[137] Co-infection with chikungunya and/or dengue is possible.[138]
The Centers for Disease Control and Prevention recommends testing for dengue at the same time as Zika in select patients with a clinically compatible illness and risk for infection with both viruses.[161][165]
Result
depends on test and organism
Investigations to consider
antenatal ultrasound
Test
Microcephaly can sometimes be diagnosed on antenatal ultrasound, especially if performed in late pregnancy. Intrauterine diagnosis of microcephaly is made when the head circumference is ≥2 standard deviations below the mean for sex and gestational age.[166]
Pregnant women with laboratory evidence of possible Zika virus infection should have serial ultrasounds every 3 to 4 weeks to monitor fetal anatomy and growth, and be referred to a specialist.[163] In Brazil, 3 ultrasounds are recommended during low-risk pregnancies, with monthly ultrasounds recommended in pregnant women with confirmed infection.[172]
Antenatal ultrasound frequently detects structural findings associated with Zika virus infection; however, not all abnormalities are detected. Antenatal detection may vary with timing of infection or ultrasound, technical expertise, and severity of abnormalities.[173] One systematic review and meta-analysis found that overall diagnostic test accuracy of ultrasound for predicting microcephaly at birth is limited as it varies with the applied cut-offs, and that it appears more accurate at detecting the absence of microcephaly rather than its presence.[174]
Result
may show microcephaly, intracranial calcifications, or brain/eye abnormalities
amniocentesis
Test
If amniocentesis is performed as part of routine clinical care, Zika RT-PCR should be performed on amniocentesis specimens and results interpreted in the context of the limitations of amniotic fluid testing. Testing placental and fetal tissues may also be considered.[161] Amniocentesis is not recommended until after 15 weeks gestation. However, the optimal time to perform amniocentesis in order to diagnose congenital Zika virus infection is unknown.[175]
Result
positive for Zika virus RNA
head circumference measurement (newborn)
Test
Infant’s head circumference should be measured at birth, 24 hours after birth, and then regularly during early infancy using standardised methods and compared with growth standards.[166][176]
The Centers for Disease Control and Prevention defines definite microcephaly as head circumference at birth less than the third percentile for gestational age and sex, or head circumference less than the third percentile for age and sex within the first 2 weeks of life (if head circumference at birth is not available).[103]
The World Health Organization (WHO) defines microcephaly as a head circumference of ≥2 standard deviations below the mean for age and sex, and severe microcephaly as a head circumference of ≥3 standard deviations below the mean for age and sex. WHO Child Growth Standards or the INTERGROWTH-21 Size at Birth Standards should be used to interpret measurements.[176]
Some infants may present with craniofacial disproportion (i.e., the head appears disproportionately small relative to the face).[176]
Poor head growth with microcephaly developing after birth has been reported in a small number of patients in Brazil.[157]
Result
third percentile or ≥2 standard deviations below the mean (for age and sex)
newborn further evaluation
Test
A standard evaluation is recommended in all infants born to mothers with possible or confirmed infection, regardless of whether the infant has clinical findings consistent with congenital Zika syndrome. The evaluation should include: a comprehensive physical examination including growth parameters; developmental monitoring and screening using validated tools; vision screening; and newborn hearing screen at birth, with automated auditory brainstem response (ABR) if possible.[2]
In addition to this, infants with clinical findings consistent with congenital Zika syndrome, and infants without clinical findings born to mothers with laboratory evidence of possible Zika virus infection, should have the following investigations: head ultrasound; comprehensive ophthalmological examination by 1 month of age; and automated ABR by 1 month of age (if not already done as part of standard newborn evaluation).[2]
Infants with clinical findings consistent with congenital Zika syndrome should also have the following: referral to a development specialist, early intervention service programmes, and family support services; and consultation with infectious disease, clinical genetics, and neurology specialists, as well as any other clinical specialists based on the infant’s clinical findings (e.g., endocrinologist, lactation specialist, gastroenterologist, speech or occupational therapist, orthopaedist, physiotherapist, pulmonologist).[2]
Result
abnormalities consistent with congenital Zika virus infection
CT/MRI head (newborn)
Test
Recommended in infants with microcephaly (or craniofacial disproportion) where Zika infection is suspected in the mother during pregnancy, or if any neurological signs/symptoms are present in the infant.[176]
Either CT or MRI can be performed; however, an MRI may provide more detail and can potentially detect other conditions.[176]
The most common feature found on CT is brain calcifications in the junction between the cortical and subcortical white matter, often with a simplified gyral pattern and predominance of pachygyria or polymicrogyria in the frontal lobes. These calcifications often resolve; therefore, the absence of calcifications should not exclude the diagnosis, and the presence of calcifications should not be consIdered a major criterion for diagnosis.[177]
Other findings include abnormalities of the corpus callosum (hypogenesis or hypoplasia), enlarged cisterna magna, ventriculomegaly, delayed myelination, and hypoplasia of the cerebellum and brainstem.[178][179]
Some infants have been found to have vision-threatening eye findings (e.g., macular and perimacular lesions, pigmentary retinopathy and atrophy, torpedo maculopathy, haemorrhagic retinopathy).[180][181][182][183][184][185] Ocular findings were seen more often in infants with smaller cephalic diameter at birth, and infants born to mothers who reported symptoms in the first trimester.[186]
Although the risk appears to be greatest with infection in the first or second trimester, signs of congenital brain injury (e.g., subependymal cysts, lenticulostriate vasculopathy) due to Zika virus infection acquired during the third trimester of pregnancy have been reported.[156]
Fetal MRI should not be used as a screening tool. It requires specialised expertise and has limited availability in some countries.[175]
[Figure caption and citation for the preceding image starts]: CT scan of the head of an infant with Zika virus infection showing a clear distribution of periventricular calcificationsFrom the personal collection of Dr Geraldo Furtado, MD, MSc (used with permission) [Citation ends].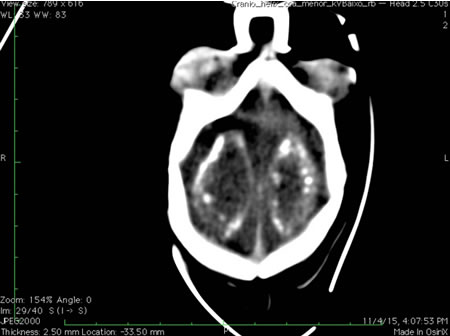
Result
may show intracranial calcifications, ventriculomegaly, cerebellar hypoplasia, callosal abnormalities, or ocular findings
tests for Guillain-Barre syndrome
Test
Nerve conduction studies/electromyography and cerebrospinal fluid (CSF) examination should be performed in patients with suspected Guillain-Barre syndrome if available; however, these investigations are not needed to make a clinical diagnosis and should not delay treatment.[143]
Interpretation of these studies and definitive diagnosis requires consultation with a neurologist.
Result
slowing of nerve conduction velocities; elevated CSF protein
Use of this content is subject to our disclaimer