Aetiology
The major causes of easy bruising can be broadly divided into the following categories:
Vascular fragility
Examples include:
Purpura simplex: the most common type, especially in females, and presents in an otherwise-healthy person without known trauma and carries no clinical significance.
Actinic purpura (also known as senile purpura): occurs commonly in older people and carries no clinical significance.
Hereditary haemorrhagic telangiectasia: a rare autosomal-dominant genetic disorder that leads to abnormal blood vessels in the skin, mucous membranes, and organs, and, therefore, may be associated with increased bruising.[3]
Excess or chronic corticosteroid use or source of endogenous cortisol (e.g., overproduction of adrenocorticotrophic hormone by the pituitary in Cushing's disease, or overproduction of cortisol by an adrenal tumour) may cause Cushing's syndrome and vascular fragility, resulting in easy bruising.
External factor-related
External factors that commonly cause easy bruising include:
Medications: anticoagulants, antiplatelet agents, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and antidepressants are common causative medications.[4][5][6][7][8][9] Herbal medicines should also be considered.
Alcohol abuse: can be associated with liver failure, thrombocytopenia, and decreased coagulation factor production, which can lead to easy bruising.
Physical abuse: should be considered as an important differential of easy bruising in children or older people with multiple bruises and other physical signs of abuse.
Platelet disorders
Platelet disorders are divided into quantitative and qualitative disorders. Platelet dysfunction is associated with increased bleeding in the microvasculature, especially after trauma, and can result in easy bruising.[10]
Quantitative platelet disorders (non-bone marrow-related):
Immune thrombocytopenia (also known as idiopathic thrombocytopenic purpura or ITP), thrombotic thrombocytopenic purpura, haemolytic uraemic syndrome, and disseminated intravascular coagulation (DIC) can all be associated with severe thrombocytopenia and result in easy bruising; however, ITP is more commonly associated with easy bruising compared with the other conditions.
DIC is a manifestation of severe underlying medical problems, most commonly malignancy, sepsis, organ failure, or obstetric conditions such as placental abruption. Treatment of the underlying disease is crucial.
Drug-induced thrombocytopenia can also be associated with easy bruising. Many drugs can induce platelet-reactive antibodies (which results in accelerated platelet destruction) or bone marrow suppression. The list of drugs reported to be associated with thrombocytopenia is extensive; however, there are databases available that collate this information. University of Oklahoma Health Sciences Center: platelets on the web - drug-induced thrombocytopenia Opens in new window Common causative drugs include chemotherapy, anticonvulsants, NSAIDs, and antibiotics. Some drugs can also cause an ITP-like phenomenon where platelet destruction persists even after the causative drug has been withdrawn. Clinicians should consider this diagnosis when evaluating a patient, as it is a common cause of thrombocytopenia.
Inherited thrombocytopenias include Wiskott-Aldrich syndrome, MYH9-related disorders (formerly known as May-Hegglin anomaly), thrombocytopenia with absent radius syndrome, as well as other rarer diseases.[11]
They are all potentially life-threatening and require prompt treatment.
Qualitative platelet disorders:
Easy bruising may be a feature of genetic disorders that affect platelet function, including:[12]
Bernard-Soulier disease (abnormal platelet adhesion)
Glanzmann's thrombasthenia (abnormal platelet aggregation)
Platelet storage pool disease, the most common type being dense granule/secretion defects (abnormal platelet secretion)
Gi signalling or thromboxane pathway defects (rare).
Bone marrow disorders
These diseases result in severe thrombocytopenia, which causes easy bruising because of the lack of platelets available to participate in the coagulation processes. The most common diseases in this group include:
Leukaemia (e.g., acute lymphocytic or myelogenous leukaemia)
Lymphoma (e.g., Hodgkin's or non-Hodgkin's lymphoma)
Other malignancies with extensive bone marrow involvement (e.g., multiple myeloma, solid tumours).
In myelofibrosis, the bone marrow can be replaced by clonal stem cells and/or extensive fibrosis resulting in thrombocytopenia. Aplastic anaemia and myelodysplastic syndrome should also be considered, although these are less common.
Coagulation factor disorders
Coagulation factor disorders cause prolonged bleeding after trauma because of an abnormal coagulation pathway, resulting in easy bruising. The most common disorders include:
von Willebrand disease: the most common inherited bleeding disorder, and one that can be life-threatening in severe cases.[13]
Haemophilia: although not a common cause of easy bruising in the general population, haemophilia is an important diagnostic consideration as it may be life-threatening. It is a bleeding disorder with an X-linked inheritance pattern that occurs secondary to a deficiency of coagulation factor VIII (haemophilia A) or factor IX (haemophilia B).[14]
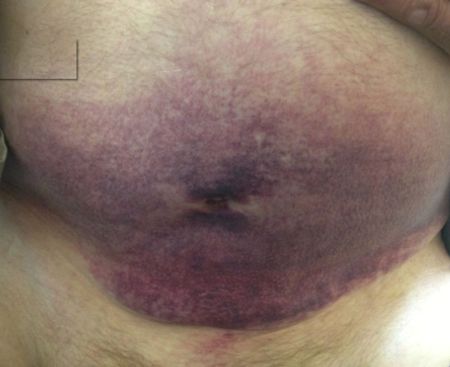
Acquired coagulation inhibitors: this is rare, with the most common inhibitors directed against factor VIII and von Willebrand factor. Associated with life-threatening bleeding if not diagnosed and managed appropriately. Occurs more commonly in older people and can be associated with malignancy and autoimmune or other inflammatory conditions.[15] Patients may also develop factor inhibitors in the postnatal period.[15][16][Figure caption and citation for the preceding image starts]: Large bruise on the abdomen of a patient on warfarin with acquired factor V inhibitorBMJ Case Reports; doi:10.1136/bcr-2013-010018. Copyright © 2014 by the BMJ Publishing Group Ltd [Citation ends].
Connective tissue disorders
Marfan's syndrome and Ehlers-Danlos syndrome are genetic connective tissue disorders that can cause easy bruising, although they are an uncommon aetiology, mainly due to the rarity of these diseases. The defective connective tissue in these diseases cause increased vascular fragility and microvascular bleeding underneath the skin.
Vitamin deficiency
Vitamin C and K deficiency can be associated with easy bruising. Vitamin K deficiency is commonly seen in hospitalised patients who have received prolonged intravenous antibiotics or in patients with malnutrition, while vitamin C deficiency may be seen in people with a history of a lack of fresh fruit and vegetable intake over prolonged periods of time.[Figure caption and citation for the preceding image starts]: Bruising affecting the thigh and pelvic area in a patient with vitamin C deficiencyBMJ Case Reports; doi:10.1136/bcr.08.2008.0750. Copyright © 2014 by the BMJ Publishing Group Ltd [Citation ends].
Systemic illness
Systemic illnesses such as cirrhosis, acute liver failure, and vasculitis are common causes of easy bruising.[Figure caption and citation for the preceding image starts]: Bruising in patient with vasculitis (drug-induced)BMJ Case Reports; doi:10.1136/bcr-2012-007319. Copyright © 2014 by the BMJ Publishing Group Ltd [Citation ends].
Other
Gardner-Diamond syndrome (also known as autoerythrocyte sensitisation syndrome or psychogenic purpura) is a rare condition typically found in young females with psychiatric disorders characterised by painful bruising.[17]
Use of this content is subject to our disclaimer